Impaired Joint Mobility
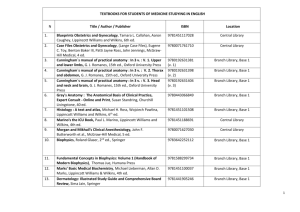
advertisement

Chapter 7 Impaired Joint Mobility and Range of Motion Copyright 2005 Lippincott Williams & Wilkins Mobility Impairment Arthrokinematic Movements of the joint surfaces Descrptive terms – roll, spin, glide Necessary component of osteokinematic motion Osteokinematics Movements of the bones Described in terms of planes (e.g., elevation in the sagittal plane) Copyright 2005 Lippincott Williams & Wilkins Continuum Hypomobility – Contracture/adaptive shortening. Contracture – Condition of fixed high resistance to passive stretch of tissue resulting from fibrosis or shortening of the soft tissues around a joint or of the muscles. Copyright 2005 Lippincott Williams & Wilkins Continuum Result of remodeling of dense tissue after surgery, immobilization, etc. Adaptive Shortening – May result from holding a limb in a posture. Copyright 2005 Lippincott Williams & Wilkins Instability Excessive range of osteokinematic or arthrokinematic movement for which there is no protective muscular control. Hypermobility Excessive joint mobility, laxity, or length of a tissue. Hypermobility may lead to or have instability as well. Copyright 2005 Lippincott Williams & Wilkins Relative Flexibility Comparative mobility at adjacent joints If Hypomobile Adjacent segment/joint are hypermobile Copyright 2005 Lippincott Williams & Wilkins Morphology and Physiology of Normal Mobility Normal mobility – Osteokinematic motion, arthrokinematic motion, and neuromuscular coordination to achieve purposeful movement. Joint ROM – Quantity of motion available at a joint or series of joints. Muscle ROM – Functional excursion from its fully lengthened position to its fully shortened position. Requires adequate tissue length to allow full ROM of articular surfaces Interposed tissues Joint capsule Ligaments Tendons Muscles Bursae Fascia Skin Copyright 2005 Lippincott Williams & Wilkins Causes and Effects of Decreased Mobility Adaptive Trauma to soft tissue Surgery (e.g., joint replacement) Joint disease (e.g., osteoarthritis) Prolonged immobilization Neuromuscular disease shortening of soft tissues Disuse Weakness Pain Decreased loading Mobility limitation Compensation Copyright 2005 Lippincott Williams & Wilkins Effects On Muscle Immobilization The longer the immobilization, the greater the atrophy Muscle fiber atrophy (Type I > Type II) Decrease in electrical activity Remobilization Factors affecting rate and end point – position and time of immobilization Decrease in stiffness Copyright 2005 Lippincott Williams & Wilkins Effects On Tendon Immobilization Reduced collagen fiber bundles, water content, glycosaminoglycans (GAG), stiffness, tissue weight, elastic stiffness Remobilization Acceleration of collagen synthesis Early remobilization – improvement of tensile strength and energy absorption Less adhesions postsurgically Copyright 2005 Lippincott Williams & Wilkins Effects On Ligament Immobilization Decreased collagen mass, strength, and stiffness, ligament’s mechanical properties Remobilization May restore mechanical and structural properties of insertion sites Structural properties inferior to mechanical stress Tissue response is dependant on immobilization period Copyright 2005 Lippincott Williams & Wilkins Effects On Articular Cartilage Immobilization Degeneration of articular surface Increased water content Altered proteoglycan organization Decrease in GAG content, cartilage thickness, hyaluronic acid content, proteoglycan synthesis Remobilization Depends on length of immobilization, injury, status prior to immobilization, available joint motion & load distribution Remobilization may prevent associated degeneration, degradation of articular cartilage and progression to osteoarthritis Copyright 2005 Lippincott Williams & Wilkins Effects On Bone Immobilization Resorption in early phases Bone mineral loss Effects are more profound than in other tissues Remobilization Response exceeds that of all other tissues Depends on bone quality Restoration of mechanical forces reverses bone loss Copyright 2005 Lippincott Williams & Wilkins Mobility Examination and Evaluation Goniometric measurements (actively or passively – reliability is greater for active ROM) Ensure proper positioning of patient Selective tissue tension testing Joint play maneuvers (arthrokinematics) Muscle ROM (flexibility tests) Copyright 2005 Lippincott Williams & Wilkins Therapeutic Intervention for Decreased Mobility Stretching Joint mobilizations Adjunctive agents may enhance the effectiveness of exercise interventions Copyright 2005 Lippincott Williams & Wilkins Elements of the Movement System Elements of the movement system must be prioritized and amenable to the determined physical therapy intervention. Copyright 2005 Lippincott Williams & Wilkins Activities to Increase Mobility Passive ROM (PROM) – Mobility activities performed without any muscular activation. Performed w/in available ROM Pulleys, CPMs, dynamic splinting Use of family members, various household objects PROM – commonly used when active ROM may disrupt the healing process Goal – Prevention of negative effects of immobilization, joint contractures, soft tissue tightness, decreased pain & enhancement of vascular dynamics and synovial diffusion. Copyright 2005 Lippincott Williams & Wilkins Activities to Increase Mobility Active Assisted ROM (AAROM) Mobility activities in which some muscle activation takes place. Indicated when some activation is desired or approved. Used to initiate gentle muscle activity after musculotendinous surgical procedures. Indicated for pts unable to complete ROM actively b/c of weakness from trauma, neuro injury, neuromuscular disease, or pain. Goal – same as PROM Copyright 2005 Lippincott Williams & Wilkins Activities to Increase Mobility Active ROM (AROM) Mobility activities performed by active muscle contraction. Goal – same as PROM + benefits muscle contraction Requires more muscle coordination (can be gravity loaded or minimized). Should follow any passive technique to reinforce proper movement patterns. Copyright 2005 Lippincott Williams & Wilkins Considerations When Performing ROM Ensure patient comfort and safety. Ensure clinician safety by using good body mechanics. Support any areas at risk of injury resulting from hypermobility, fracture, etc. Perform ROM slowly and rhythmically. Copyright 2005 Lippincott Williams & Wilkins Considerations When Performing ROM (cont.) Move through full range as possible. Avoid excessively tight grip by grasping over large surface area. Use cardinal plane motions, combined motions, or functional movement patterns. Copyright 2005 Lippincott Williams & Wilkins Stretching Used to increase the extensibility of the muscle tendon unit and the periarticular connective tissue. Contraindicated in acute inflammation and tissue infection cases. Caution is used in patients with recent fractures, osteoporosis, the elderly, prolonged immobilization, very weak musculature. Copyright 2005 Lippincott Williams & Wilkins Stretching (cont.) Held a minimum of 30 seconds – younger patients, 60 seconds older patients Position should be comfortable, in proper alignment, and stable to allow proximal stabilization. Copyright 2005 Lippincott Williams & Wilkins Categories of Stretching – 3 1. Static (muscles held at a certain length) 2. Ballistic (quick movements impose a rapid change in length) 3. Proprioceptive neuromuscular facilitation (PNF) Copyright 2005 Lippincott Williams & Wilkins Exercise Dosage Dictated by: Stage of healing Response to loading Dosage is matched to the patient’s individual needs. Copyright 2005 Lippincott Williams & Wilkins Sequence Depends on the purpose of the ROM activity. Least amount of muscle activation increasing amount of voluntary activation Copyright 2005 Lippincott Williams & Wilkins Frequency, Intensity, Duration Frequency Inversely related to intensity & duration Relative to physiologic, kinesiologic (performed 2–5 times per day) Learning factors (e.g., postural re-education – performed numerous times daily) Copyright 2005 Lippincott Williams & Wilkins Precautions and Contraindications PROM, AAROM, AROM Contraindicated when motion could disrupt healing process. Copyright 2005 Lippincott Williams & Wilkins Joint Mobilization “Continuum of skilled passive movements to the joints and/or related soft tissues that are applied at varying speeds and amplitudes, including small-amplitude/high velocity therapeutic movement.” Classification systems focus on increasing joint mobility by increasing joint play or motion between the joint surfaces. Copyright 2005 Lippincott Williams & Wilkins Mobilization Grades Copyright 2005 Lippincott Williams & Wilkins Applications to Specific Joints Shoulder Elbow Wrist and hand Hip Knee Foot and ankle Spine Numerous modifications Positioning varies Copyright 2005 Lippincott Williams & Wilkins Causes and Effects of Hypermobility Cause Traumatic injury Genetic predisposition Effect May lead to instability Copyright 2005 Lippincott Williams & Wilkins Therapeutic Exercise Intervention for Hypermobility Spondylolysis at L4 Anatomic impairment Base element Faulty posture during movement Movement impairment Biomechanical element Pain Inability to run Impairment Choice of intervention – stabilization of biomechanical element Disability Copyright 2005 Lippincott Williams & Wilkins Stabilization Exercises Dynamic activities that attempt to limit and control excessive movement. Focus on increasing short muscles through static stretching, followed by active contraction of antagonist. Activity should be based on the direction in which the segment is susceptible to excessive motion. Supportive devices (taping, bracing) may be necessary initially. Copyright 2005 Lippincott Williams & Wilkins Closed-Chain Exercises Rationale Muscular cocontraction, decreased shear forces, increased joint compression Lower Extremity Squats, lunges, step ups etc. Upper Extremity Pushups, modified pushups, weight bearing with hands on table Copyright 2005 Lippincott Williams & Wilkins Open-Chain Stabilization Particularly effective in late stages of rehabilitation Sitting, prone, and supine activities combined with arm reaching and leg lifts can be used from early to advanced stages of stabilization Copyright 2005 Lippincott Williams & Wilkins Ballistic Exercises Produces cocontraction about a joint through triphasic muscle activation. Results in synchronous activation of agonists and antagonists. Rapid flexion & extension of the hip through a small range elicits co-activation of agonist & antagonist . Slow movement produces reciprocal activation of same group(s). Copyright 2005 Lippincott Williams & Wilkins Exercise Dosage Depends on purpose of exercise Signs of fatigue (e.g., substitution) alters performance and may be indicative of loss of desired stabilization Copyright 2005 Lippincott Williams & Wilkins Life Span Issues Flexibility remains stable through age 8 Declines until ages 11–15 Mobilizations, generally not used in children (except for some CNS disorders) Static stretching (as compared to PNF, etc.) may be less susceptible to contraction-induced injury for the elderly Declining ROM, joint capsule tensile strength, articular water content, bone fragility should be considered when treating the elderly Copyright 2005 Lippincott Williams & Wilkins Adjunctive Agents Superficial heat Deep heat Taking advantage of collagen’s response to increased intramuscular temperature. Copyright 2005 Lippincott Williams & Wilkins Summary Immobilization has detrimental effects on soft tissues, bone, and insertion sites. Effects are result of specific adaptations. Time required to restore structural and mechanical properties can be twice that of the immobilization period. Joint ROM should be differentiated from muscle ROM. Contractile and non-contractile tissues limit joint mobility. Copyright 2005 Lippincott Williams & Wilkins Summary (cont.) PROM – Mobility without muscle contraction. AAROM – Some muscle activity. AROM – Uses active muscle contraction. Joint mobilization is indicated when capsular restriction is a key finding. Various devices (home and clinical) can be used to assist in mobility exercises. Copyright 2005 Lippincott Williams & Wilkins Summary (cont.) Mobility exercise prescription depends on the specific goal of the activity and the environment in which it will be performed. Hypermobility can be as disabling as hypomobility. Stabilization exercises may be incorporated. Adjunctive agents (heat, etc.) can be used to enhance mobility activities. Copyright 2005 Lippincott Williams & Wilkins