CLINICAL STEPS FOR COMPLETE DENTURE
advertisement

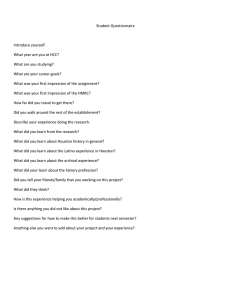
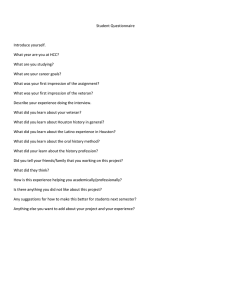
CLINICAL STEPS FOR COMPLETE DENTURE 1. 2. 3. 4. 5. 6. 7. 8. EXAMINATION,DIAGNOSIS & TREATMENT PLANING. PREPROSTHETIC SURGERY ( IF REQUIRE) PRIMARY IMPRESSION SECONDARY IMPRESSION JAW RELATION RECORD TRY-IN PROCEDURE DENTURE INSERTION POST INSERTION FOLLOW-UP CONTENTS • • • • • • INTRODUCTION PRINCIPLES OF IMPRESSION MAKING OBJECTIVES OF IMPRESSION MAKING CLASSIFICATION OF IMPRESSION TECHNIQUES STEPS IN IMPRESSION MAKING PRIMARY IMPRESSION MAKING INTRODUCTION • The beginning of a good denture starts with making of a good impression,so a good impression is a stepping stone Definition A complete denture impression is a negative registration of the entire denture bearing, stabilizing and border seal areas present in the edentulous mouth ( GPT-7) Principles of making an impression: 1. 2. 3. 4. 5. 6. 7. 8. 9. Tissues of the mouth must be healthy. Impression should include all of the basal seat within the limits of the health and function of the supporting and limiting tissues. The borders must be in harmony with the anatomical and physiological limitations of the oral structures. Selective pressure should be placed on the basal seat during the making of the impression Proper space for the selected impression material should be provided within the tray Impression must be removed from the mouth without damage to the mucous membranes of the residual ridges. Guiding mechanism should be provided for correct positioning of the imp. tray. Tray and impression material should be made of dimensionally stable materials. External shape of the material should be similar to the complete denture OBJECTIVES OF IMPRESSION MAKING 1. 2. 3. 4. 5. Support Retention Stability Esthetics Preservation of Alveolar Ridges SUPPORT It is the foundation area on which a dental prosthesis rests. GPT-8 Dental support is the resistance to vertical forces of mastication and to occlusal or other forces in a direction towards the basal seat. The mucoperiosteum along with the alveolar ridges is not meant to receive functional loads. It is thus necessary, to enhance the available support by utilizing maximum coverage of all usable ridge bearing areas. Areas of support: The areas of support are divided into: • PRIMARY • SECONDARY • SLIGHT PRIMARY: These are the areas of the edentulous ridge that are at right angles to occlusal forces and usually do not resorb easily. MAXILLARY: Posterior ridges and flat areas of the palate. MANDIBULAR: Buccal shelf area and posterior ridges. SECONDARY: Areas of the edentulous ridge that are greater than at right angles to occlusal forces or are parallel to them; also the areas of the edentulous ridge that are at right angles to occlusal forces but tend to resorb under load. MAXILLARY: Anterior alveolar ridge and rugae area. MANDIBULAR: Anterior alveolar ridge and posterior ridge crest. SLIGHT: Areas of very displacable tissues, that is ; all the vestibular areas that provide very little support but are needed for the very important peripheral seal. Importance of buccal shelf area: It is the area of bone between the extraction sites of molars and the external oblique ridge. It has an intact cortical plate and tends not to resorb under load. The buccinator muscle in this region has its fibres in a horizontal direction which is relatively inactive and flaccid during function Importance of covering the pear shaped pad: Craddock coined the term pear shaped pad and refers to the area formed by residual scar of the third molar and the retromolar papilla. Sicher has described retromolar pad as a soft elevation of mucosa that lies distal to the third molar. The mucosa of the pear shaped pad is usually attached gingiva. An examination after drying will reveal that the mucosa is firm, stippled and has a dull appearance. The retromolar pad has a shiny and soft appearance. The pad can be also used for determining the occlusal plane of the lower denture. Palatal support: The palate requires relief only when there is a presence of torus or the area over the midpalatine raphae is thin. In most of the cases horizontal part of the hard palate can be used for gaining support. Methods to improve support are • • • • • Surgical removal of pendulous tissue Use of tissue conditioning materials Surgical removal of sharp or spiny mandibular ridges Surgical enlargement of ridge Implants RETENTION It is the resistance to removal in a direction opposite to that of insertion The factors of retention are : • Adhesion • Cohesion • Interfacial surface tension • Capillarity • Mechanical locking into undercuts • Peripheral seal and atmospheric pressure • Oral and facial musculature ADHESION • The physical attraction of unlike molecules to one another. • Role of saliva • The amount of adhesion present is proportional to denture base area. COHESION • The physical attraction of like molecules for each other. • Watery serous saliva can form a thinner film and is more cohesive than thick mucous saliva. INTERFACIAL SURFACE TENSION • The tension or resistance to separation possessed by the film of liquid between two well adapted surfaces. • Saliva should be thin and even. • Perfect adaptation between tissues and denture base. • Cover large area • Good adhesive and cohesive forces. CAPILLARY ATTRACTION • That quality or state, because of surface tension causes elevation or depression of the surface of a liquid that is in contact with a solid. • Closeness of adaptation. • Greater surface of denture bearing area. • Thin film of saliva. ATMOSPHERIC PRESSURE & PERIPHRAL SEAL • Peripheral seal is area of contact between peripheral borders of denture and resilient limiting structures. • Prevents air entry between denture surface and soft tissue. • Retention by atmospheric pressure is directly proportional to denture base area. • UNDERCUTS: Unilateral undercuts aid in retention. • ORAL MUSCULATURE: Supplementary retentive forces. • Forces from buccal musculature and tongue are neutralized- neutral zone. • Artificial teeth arranged in neutral zone to achieve good retention. STABILITY : Stability of a denture is its ability to remain securely in place when it is subjected to horizontal movements. For the denture to be stable it requires • Good retention • Non interfering occlusion • Proper tooth arrangement • Proper form and contour of the polished surfaces • Proper orientation of the occlusal plane • Good control and co ordination of the patients musculature. ESTHETICS • The role of esthetics in impression making refers to the development of the labial and buccal borders so that they are not only retentive but also support the lips and cheeks properly PRESERVATION OF ALVEOLAR RIDGES M.M.DE VAN DICTUM THE PRESERVATION OF THAT WHICH IS OF UTMOST IMPORTANCE AND NOT THE METICULOUS REPLACEMENT OF THAT WHICH HAS BEEN LOST . IMPRESSIONS SHOULD RECORD THE DETAILS OF THE BASAL SEAT AND PERIPHERAL STRUCTURES IN AN APPROPRIATE FORM TO PREVENT INJURY TO THE ORAL TISSUES. THE PERIPHERAL TISSUES SHOULD BE RECORDED ACCURATELY TO PREVENT OVER-EXTENSION OF THE DENTURE AND TISSUE IRRITATION. Impression techniques may be classified depending on: a) Amount of pressure used 1. Pressure technique( MUCOCOMPRESSIVE) 2. Minimal pressure technique( MUCOSTATIC) 3. Selective pressure technique b) Based on the position of the mouth while making impression 1. Open mouth 2. Close mouth c) Based on the method of manipulation for border molding. 1. Hand manipulation 2. Functional movements Pressure theory or mucocompressive theory: This theory was proposed on the assumption that tissues recorded under functional pressure provided better support and retention for the denture STEPSPrimary impression made with impression compound Special tray made Impression made with compound Bite rim made with compound Relief of mid palatine raphae Peripheral muscle trimming Borders are molded by asking the patient to perform functional movements. Minimal pressure or mucostatic theory – The main advantage of this technique is its high regard for tissue health & preservation. STEPS• A compound impression is made. • A baseplate wax space is adapted. • A special tray is made. • Spacer is removed and an impression is made with a free flowing material with little pressure. • Escape holes are made for relief. Selective pressure theory • Advocated by Boucher in 1950 it combines the principles of both pressure and minimal pressure technique. • In this technique idea of tissue preservation is combined with mechanical factor of achieving retention, through minimum pressure which is within physiologic limits of tissue tolerance. STEPS IN MAKING AN IMPRESSION( PRIMARY) Preliminary examination of the patient Seating the patient Selection of the tray Selection of the material Making impression SEATING OF THE PATEINT Position of the operator for maxillary impression ( 11 O’ CLOCK) Position of the operator for mandibular impression (7 O’ CLOCK) Types of Trays TRAYS DESIGN SECTIONAL STOCK EDENTULOUS PERFORATED TRIPLE DENTULOUS CUSTOM EDENTULOUS DENTULOUS NONPERFORATED TRAY MATERIALS PLASTIC RESIN HEAT CURE RESIN SHELLAC BASE PLATE SELF CURE RESIN METALLIC STOCK TRAYS PERFORATED TRAYS NON PERFORATED TRAYS CUSTOM TRAY