ODONTOGENIC TUMOURS LECTURE FOR 3RD YEAR
advertisement
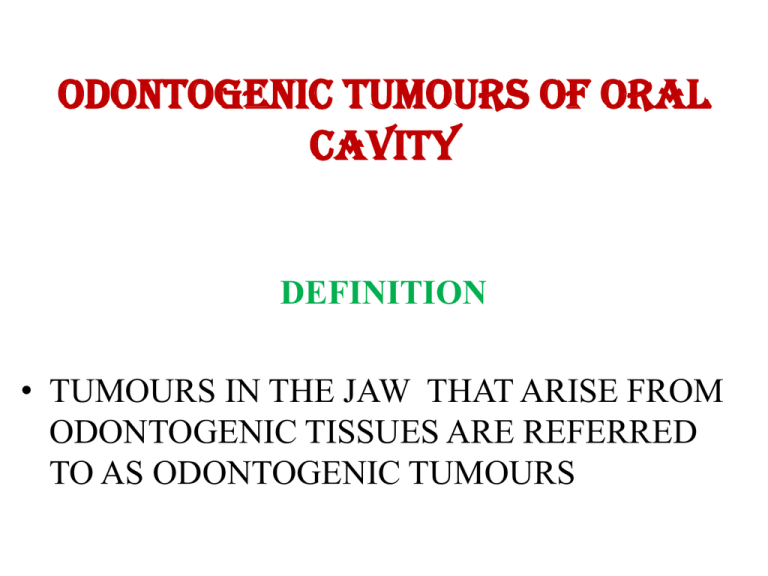
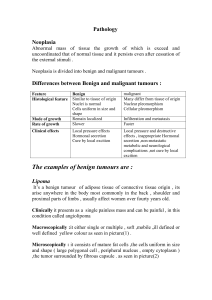
ODONTOGENIC TUMOURS OF ORAL CAVITY DEFINITION • TUMOURS IN THE JAW THAT ARISE FROM ODONTOGENIC TISSUES ARE REFERRED TO AS ODONTOGENIC TUMOURS CLASSIFICATION OF ODONTOGENIC TUMOURS (W.H.O CLASSIFICATION) BENIGN 1. ODONTOGENIC EPITHELIUM WITHOUT ODONTOGENIC ECTOMESENCHYME • • • • AMELOBLASTOMA SQUAMOUS ODONTOGENIC TUMOUR CALCIFYING EPITHELIAL ODONTOGENIC TUMOUR (PINDBORG) ADENOMATOID ODONTOGENIC TUMOUR 2. ODONTOGENIC EPITHELIUM WITH ODONTOGENIC ECTOMESENCHYME 1. 2. 3. 4. 5. 6. 7. AMELOBLASTIC FIBROMA AMELOBLASTIC FIBRODENTINOMA AMELOBLASTIC FIBRO ODONTOMA ODONTO AMELOBLASTOMA CALCIFYING ODONTOGENIC CYST COMPLEX ODONTOMA COMPOUND ODONTOMA 3.ODONTOGENIC ECTOMESENCHYME WITH OR WITHOUT ODONTOGENIC EPITHELIUM • ODONTOGENIC FIBROMA • MYXOMA • CEMENTOBLASTOMA MALIGNANT 1. ODONTOGENIC CARCINOMAS: • • • • MALIGNANT AMELOBLASTOMA PRIMARY INTRAOSSEOUS CARCINOMA CLEAR CELL ODONTOGENIC CARCINOMA GHOST CELL ODONTOGENIC CARCINOMA 2. ODONTOGENIC SARCOMAS: • • • AMELOBLASTIC FIBROSARCOMA AMELOBLASTIC FIBRO DENTINO SARCOMA AMELOBLASTIC FIBRO ODONTO SARCOMA BENIGN VS MALIGNANT TUMOUR Depending upon their spread by invasion and metastasis, tumours are classified as benign or malignant. Benign tumors cannot spread by invasion or metastasis; hence, they only grow locally. Encapsulated, enlargement by peripheral expansion, pushes away the adjoining tissues and structures. Malignant tumors spread by invasion and metastasis. Rapidly infiltrates the surrounding tissue. By definition, the term "cancer" applies only to malignant tumors. GENERAL PRINCIPLES OF DIAGNOSIS & MANAGEMENT OF JAW LESIONS HISTORY OF LESION • DURATION LONG HISTORY OF DURATION CONGENITAL LONG HISTORY OF DURATION (SLOW GROWTH) NO-PAIN BENIGN SHORT HISTORY OF DURATION, FAST GROWTH MALIGNANT • Mode of onset & ProgressE.g; history of trauma Osteogenic Sarcoma Rapid growth Malignant Slow growth Benign • Size & Shape To know the origin of the lesion. • Progression of the lesion: Slowly growing and same size for long time Benign Same size for long time and the again growing Malignant transformation of Benign lesion. Continuously growing Malignant • Change in character of lesion Ulceration, fluctuation, softening noticed by the patient. If painless swelling has become painful, can be infection. • Associated symptoms Pain Abnormal sensations like anesthesia, paresthesia Nasal obstruction Difficulty in breathing Tenderness Lymphadenopathy Trismus Similar swellings elsewhere in the body to rule out metastasis Loss of body weight Any habits Recurrence after previous surgery CLINICAL EXAMINATION • General physical examination • Examination of oral cavity, external face, regional lymph nodes. • Inspection • Palpation (Bimanual palpation) • Percussion • Auscultation Imaging & biopsy • PLAIN RADIOGRAPHS • CT SCAN • MRI • HISTO-PATHOLOGICAL EXAMINATION AFTER BIOPSY PRINCIPLES OF SURGICAL MANAGEMENT OF JAW TUMOURS • • • • • • ENUCLEATION CURETTAGE MARSUPIALIZATION RESECTION WITHOUT CONTINUITY DEFECTS RESECTION WITH CONTINUITY DEFECTS DISARTICULATION RESECTION WITHOUT CONTINUITY DEFECTS • MARGINAL RESECTION / EN-BLOCK RESECTION RESECTION WITH CONTINUITY DEFECTS • INFERIOR BORDER OF MANDIBLE • PARTIAL RESECTION • HEMI-MANDIBULECTOMY • DISARTICULATION • TOTAL RESECTION • COMPOSITE RESECTION AMELOBLASTOMA INCIDENCE - MOST COMMON ODONTOGENIC NEOPLASM AGE-THIRD DECADE OF LIFE SEX (M:F) - EQUAL SITE: MANDIBLE - 80% (70% IN THE POSTERIOR MOLAR REGION AND RAMUS REGION) Recurrence is common • True neoplasm of enamel organ type tissue • Definition : ACCORDING to ROBINSON “ usually uni-centric, non functional, intermittent in growth, anatomically benign and clinically persistent”. Pathogenesis Cell rests of enamel organ Epithelium of odonotogenic cysts – dentigerous cyst Disturbances of developing enamel Basal cells of surface epithelium Presently – alteration or mutation in the genetic material of the cells that are programmed for tooth development Etiology Irritation: Infection – ROBINSON – 1/3rd of cases- oral infections Trauma: Dietary deficiency – defect in development of tooth germ Virus – polyoma virus Classification • CENTRAL- INTRAOSSEOUS • PERIPHERAL- EXTRAOSSEOUS • • • • • • • • • • CLINICAL FEATURES Usually asymptomatic at its early phase Late stage Intra-oral & extra-oral jaw swelling Disturbed normal occlusion and tooth eruption. Teeth in the region are mobile ill-fitting dentures Ulcerations Nasal obstructions Nerve involvement, lower lip paresthesia Egg shell cracking of bone RADIOGRAPHIC FEATURES • Appears as Unilocular - Monocystic OR Multilocular - Multicystic radiolucency. • Honey - Comb / Soap Bubble Appearance. TNM CLASSIFICATION OF CARCINOMAS OF ORAL CAVITY • • • • • • • • • T – PRIMARY TUMOUR TX – Primary tumour can not be assessed T0 – No evidence of primary tumour TIS – Carcinoma in situ T1 – Tumour 2cm or less in greatest dimention T2 – Tumour more than 2cm but less than 4cm T3 – More than 4cm T4a – LIP (Tumour invades through cortical bone, inferior alveolar nerve, floor of mouth, or skin ) T4a – ORAL CAVITY (Tumour invades through cortical bone, into deep/extrinsic muscle of tongue (genioglossus, hyoglossus, palatoglossus, and styloglossus), maxillary sinus, or skin of face. T4b – LIP & ORAL CAVITY ( Tumour invades masticator space, pterygoid plates, or skull base; or encases internal carotid artery ) N – Regional lymph nodes metastasis • NX - Regional lymph nodes cannot be assessed • N0 - No regional lymph node metastasis • N1 - Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension • N2 - Metastasis as specified in N2a, 2b, 2c below • N2a - Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm in greatest dimension • N2b - Metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension • N2c - Metastasis in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension • N3 - Metastasis in a lymph node more than 6 cm in greatest dimension M – Distant metastasis • MX - Distant metastasis cannot be assessed • M0 - No distant metastasis • M1 - Distant metastasis • • • • • • • Stage grouping Stage 0 - Tis N0 M0 Stage I - T1 N0 M0 Stage II - T2 N0 M0 Stage III - T1, T2 N1 M0 T3 N0, N1 M0 Stage IVA - T1, T2, T3 N2 M0 T4a N0, N1, N2 M0 Stage IVB - Any T N3 M0 T4b Any N M0 Stage IVC - Any T Any N M1