case report
advertisement
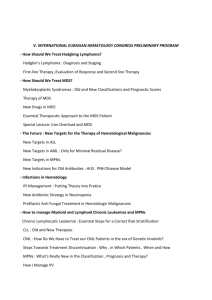
Case report Lymphocyte Rich Hodgkin's Lymphoma Presenting with Immune Pancytopenia: A Case Report and Literature Review. Dr. I. A. Adam1, Dr. O. H.Musa1, Dr. A. Kordofani2, Dr. L. Gafaar2 We report a case of LRHL presenting with autoimmune pancytopenia that resolves after steroid and four cycles of ABVD chemotherapy. Review of the literature revealed 3 previous cases of same histological type with AIHA; however immune pancytopenia has not been reported so far. Clinicians should consider cHL as possible differential in patients affected by what is thought to be idiopathic AIHA. More data recruitment and analysis are very crucial to exactly define the pathophysiology of this rare entity. 1- Introduction: Hodgkin's disease is an uncommon, but, currently highly curable disorder accounting for ten percent of all diagnosed lymphoma, and only approximately one percent of cancer registered in developed countries each year. Fatigue is almost constantly seen at the time of diagnosis mostly secondary to anaemia. The pathogenesis of anaemia varies; it could be secondary to chronic disease reflecting the underlying malignancy. In advanced disease, anaemia occurs from marrow suppression by the infiltrating malignant cells. It can be iatrogenic due to bone marrow suppression by chemotherapeutic agents. Rarely does it result from autoimmunehaemlolytic process. Autoimmune haemolytic anaemia (AIHA) is rarely seen in Hodgkin's lymphoma with reported incidence of 0.2- 4.2%. reported cases and literature reviews have shown that when AIHA occurs in HL, it happens mostly at stages III and IV of nodular sclerosis HL (NSHL) or mixed cellularity HL (MCHL). Here, we discuss a case of lymphocyte rich HL (LRHL) with immune pancytopenia [1-8]. 2- Case Report: A thirty six year old Sudanese male presented complaining of generalized fatigue, fever, palpitations and mild loss of weight for three months. He also mentioned a history of similar condition few months ago which was diagnosed as malaria complicated by anaemia and was treated accordingly. No past medical history or family history of note. Examination revealed severe pallor, jaundice, and generalized lymphadenopathy including cervical, axillary, and inguinal groups, but, no hepatosplenomegally. Examination of the chest, cardiovascular system, abdomen, and central nervous system was unremarkable. The CBC revealed WBC 2500 x 109 /L, neutrophils 800 x 109 /L, Hb 6.8 g/dl, MCV 112.8 fl, platelets 22000x109/L, and reticulocytes 16%. Lactate dehydrogenase (LDH) was high at 348 U/L, total bilirubin was 1.47 mg/dl mainly direct. Direct Coomb's Test (DAT) was strongly positive (+++). Other biochemical profiles were normal. Bone marrow aspiration and biopsy showed no evidence of malignant infiltration, but, revealed marked trilineage hyperplasia, especially of erythropoiesis consistent with a haemolytic process. In the interim a biopsy from axillary lymph node was taken for histopathological assessment. 1 Abdominal sonography and chest X-ray were normal. The patient was admitted, transfused two units of PRBC, 6 units of platelets, and started intravenous methyl prednisolone. A prompt increase of platelets to 66000x 109 /dl and then to 202000x109 /dl within one week was appreciated, by that time, the histopathological report was obtained and demonstrated an effaced architecture with numerous small cells, large Reed- Sternberg cells, few eosinophils and neutrophils. Immunohistochemical stains indicated RS cells being positive for CD30 and CD15 and negative for CD45 (LCA) and CD20. Biopsy results were interpreted as classical lymphocyte rich Hodgkin's lymphoma. Table 1-1: Laboratory data of our patient. Variables Haemoglobin (g/dl) Reticulocyte % WBC ( x 109/L) Neutrophils (x109/L) Platelets (x109/L) T. bilirubin(mg/dl) D.bilirubin (mg/dl) LDH (IU/L) Direct Coomb's test 0n admission 6.8 16 2.5 0.8 22 1.47 0.51 348 +++ 1 week of steroid 9.6 Following End of 3th st the 1 cycle of cycle of ABVD ABVD 7.8 7 4.9 3.2 202 4.1 2.9 66 10.5 2.7 1.3 224 243 3- Results: The patient was started on ABVD (Adriamycin, bleomycine, , vinblastine, and dacarbazine) chemotherapy, and has so far completed four cycles and showed both clinical improvement in terms of symptoms and signs, and laboratory improvement i.e. resolution of immune cytopenia. 4- Discussion: Lymphocyte rich HL represents about 1% of cases, typically found in older individual with early stages (I or II). Bulky disease, B symptoms and extra-nodal involvement are not typical for this class, so our patient displayed a unique clinical presentation by exhibiting both B symptoms and advanced disease stage (stage III) [2,911]. Fifty four percent of AIHA in adults are secondary to underlying diseases such as autoimmune diseases and malignancy. The relationship of AIHA with classical HL (cHL) has been recognized for more than forty years; however there is no extensive primary literature that has characterize this association , except for sporadic reported cases. Q. Feng and colleague recently reviewed 40 published cases including 8 paediatric, of HL with AIHA and summarized the general, clinical and pathological characteristics. Our patient differs from all of their reported cases, in the fact that he presented with immune pancytopenia rather than isolated AIHA or ITP. DCT was positive in 93% of their patients, mostly specified as IgG and/or C3. Our patient had appositive DCT, but antibody specificity was not tested. Regarding the pathological 2 subtypes MCHL and NSHL were the most common encountered classes in their series 48% and 34% respectively, while only 10% of cases were similar to our case i. e. LRHL (3 cases). The higher incidence of AIHA in MCHL and NSHL is reasoned out by their higher incidence compared with other subtypes. AIHA is the onset symptom in 40% of cases,; according to the same series, but it may precede the disease. Its development in patient previously treated for HD indicate relapse of the disease. Some authors claimed that steroid treatment may masks HL clinical courses making it difficult to diagnose, lack of regular follow-up may also delay diagnosis [3,12,13] It was not clear how autoantibody production is induced in AIHA. Normally low titer of autoimmunogenic IgM are found in healthy individual. It is postulated that Bcell clone that produce these antibodies lose their regulation mechanisms and switch to produce high titer. Other studies suggested a role of T-cell deregulation in pathogenesis. This theory arises from observations in paediatric patients with autoimmune lymphoprliferative syndrome, these individuals have a defective Fasreceptor-mediated lymphocyte apoptosis making them susceptible for repeated episodes of AIHA and other autoimmune cytopenias. In other patients AIHA seems to be triggered or exacerbated by viral infection. Less common causes includes posttransplant, post-transfusion and drugs such as cephalosporins [14,15] The pathophysiology of AIHA that arises during the course of malignancies, most commonly CLL, remains mysterious. Some researchers have suggested that it is a paraneoplastic syndrome that develops secondary to the aberrant production of hormones, cytokines, or autoantibodies by neoplastic cells. It has been also hypothesized that these antibodies cross react with the red blood cells leading to their destruction. These assumptions are based on the clinical observation that AIHA responds well to chemotherapy and steroids, readily resolving shortly after treatmentis started. In addition, sporadic population based studies have demonstrated the presence of AIHA in patients later diagnosed with HD. Clonal lymphocytes have been identified in individual with apparently idiopathic AIHA as well. They may or may not develop lymphoma in the future. These findings support the theory that AIHA could result from a syndrome of a clinically silent Hodgkin's or non-Hodgkin's lymphoma. It is not clear why sometimes AIHA manifest after successful treatment and when the patient is in complete remission. Further studies are needed to explain these observations[3, 10, 13, 17, 18]. Among 40 reported cases the predominant treatment was combination of steroid, chemotherapy, and radiation, albeit few cases showed spontaneous recovery or respond to steroid treatment alone[13]. Our patient showed excellent initial response to steroid which is followed by chemotherapy. 4- References: 1- Bonadonna G.: Historical Review of Hodgkin's Disease.British Journal of Haematology.2000; 110: 504511. 2- A.C. Jones, “Epidemiology, pathology features, and diagnosis of classical Hodgkin's lymphoma," 2010, http://www.Upto-date.com/. 3 3- Lechner K, Chen Y.A. Paraneoplastic autoimmune cytopenia in Hodgkin's lymphoma.LeukLymphoma. 2010; 51:469-471. 4- Siddiqui N, Aleen A. Autoimmune Haemolyticanaemia preceding the diagnosis of Hodgkin's disease: A report of two cases and review of the literature.Journal Park MedicineAssociation.2009; 59: 316- 318. 5- Starn M, Buser A. S,Lohri A, Tichelli, Nissen- Druey A. Autoimmunity and malignancy in Haematology – more than an association. Critical Reviews in Oncology/ Haematology.2007; 63:100- 110. 6- Xiros N, Binder T, Anger B, Bohlke J, HeimpelH. Idiopathic thrombocytopenic purpura and autoimmune haemolyticanaemia in Hodgkin's disease. Eur J Haematol. 1988; 40:437- 441. 7- Andrieu J M, Younou P, Marcelli A. [Autoimmune haemolyticanaemia associated with Hodgkin's disease. Characteritics, prognosis and incidence ( authortransl). New press Med. 1981; 10: 2951- 2954. 8- Levine AM, Thorcon P, Forman SJ, et al. Positive Coomb's test in Hodgkin' disease: significance and implications. Blood.1980; 55: 607- 611. 9- Pileri S. A, Ascani S, Leoncini L, et al. Hodgkin's lymphoma: the pathologist point of view. Journal of Clinical Pathology.2002; 55: 162- 176. 10- P.P. Picculuga, C. Agostinelli, A. Gazzola et al., “Pathobiology of Hodgkin's lymphoma," Advances in Haematology, vol. 2011,Article ID920898,18 pages, 2011. 11- Anderson A, Gadalla S, Morton L. M, et al,. Population based study of autoimmune conditions and risk of specific lymphoid malignancies. International Journal of Cancer.2009; 125: 298- 405. 12- Engelfriet CP, OverbeekeMA,vondem Borne EA. Autoimmune aemolyticanaemia. SeminHematol. 1992; 29: 3- 12. 13- Feng Q, Zak D, Daya R. Autoimmune haemolyticanaemia and classical Hodgkin's lymphoma: Acase report and literature review. Clincal Advances in Hematology & Oncology.2012;10: 270-277. 14- Stahl D, Lacroix- Desmazes S, Heudes D, Mouthon L, Kaveri SV, Kazatchkine MD. Altered control of self-reactive IgG by autologous IgM in patient with warm autoimmune haemolyticanaemia.Blood.2000; 95: 328- 335. 15- Straus M.SE, Sneller M, Lenardo MJ, Puck JM, Strober W. An inherited disorder of lymphocyte apoptosis: the autoimmune lymphoproliferative syndrome. Annals of Internal Medicine.1999; 130: 591- 601. 16- FawellK, Jarrett R.F. The molecular pathogenesis of Hodgkin's lymphoma.Histopathology.2011; 58: 1525. 17- Moncharm P, Ghesquieres H, Sebban C, et al,. Severe IgA-mediated autoimmune haemolyticAnaemai in Hodgkin's lymphoma: a very rare event. Leuk and lymphoma.2007; 48: 633635. 18- Saitoh T, Matsushima T, Saito Y, et al,.Hodgkin's lymphoma presenting with various immunologic abnormalities, including autoimmune hepatitis, Hashimoto's thyroiditis, autoimmune haemolyticanaemia and immune thrombocytopenia.Clinical Lymphoma and myeloma.2008; 8: 6264. 4