Skeletal muscle contraction
advertisement

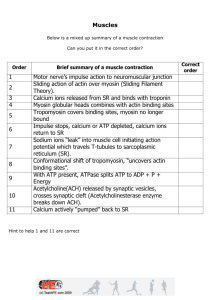
Skeletal Muscle Contraction Dr Asma Jabeen Learning objectives At the end of this lecture the students should be able to: a. Identify the internal structure of skeletal muscle fiber. b. Describe mechanism of action of actin and myosin during muscle contraction. c. Identify the role of calcium in muscle contraction. d. Explain mechanism of contraction in different muscle fibers. e. Explain the Sources of energy for muscle contraction. f. Distinguish between fast versus slow muscle fibers. g. Identify clinical application (Muscle fatigue, denervation and electromyography). Skeletal Muscle Skeletal muscles attach to skeleton. Contraction moves bones, allowing the body to perform a variety of motor activities Homeostatic functions: Acquiring, chewing and swallowing food Essential for breathing To move the body away from harm Heat generating muscle contractions Physiologic Anatomy of Skeletal Muscle Cellular Organization Muscle fibers • single cells • multinucleated • Surrounded by the sarcolemma • Outer coat: thin layerof polysaccharide material with numerous thin collagens Myofibrils • contractile elements • surrounded by the sarcoplasm Cellular organelles - lie between myofibrils (mitochondria, sarcoplasmic reticulum etc.) Molecular Organization E F Myosin Filament Multiple myosin molecules, mol wt 480,000 Each molecule composed of six polypeptide chains Two heavy, mol wt 200,000, Four light chains.. mol wt 20,000 Tails of molecules bundled together to form BODY of the filament Many heads hang outward along with part of the body called arm forming the CROSS BRIDGES Two HINGES taking part in actual contraction process ATPase activity of myosin head Myosin Filament The Actin Filament − the I band filament − tethered at one end at the Z disc − 1 mm long: v. uniform nebulin forms guide for synthesiT F-actin • double-stranded helix • composed of polymerized G-actin • ADP bound to each G-actin (active sites) • myosin heads bind to active sites Tropomyosin • covers active sites • prevents interaction with myosin Troponin • I - binds actin • T - binds tropomyosin • C - binds Ca2+ Structure of Actin and Myosin Interaction of one myosin filament, two Actin filaments and calcium ions to cause contraction A pure actin filament binds strongly and instantly with myosin heads. Binding is prevented by presence of toponin- tropomyosin complex. Before contraction, the Inhibitory effect should be inhibited Role of calcium ions Calcium binding with troponin C , causes a conformational change in troponin complex that tugs on the tropomyosin molecule and moves it deeper into Groove between the two actin strands Steps in skeletal muscle contraction (excitation contraction coupling) Action potential along sarcolemma II. AP down to T-tubule III. Calcium released from terminal cisternae SR into myoplasm IV. Increased intracellular calcium V. Binding of calcium to troponin C VI. Displacement of tropomyosin exposing myosin binding site on actin VII. Thus CROSS BRIDGE form between actin and myosin VIII. Conformational change in myosin IX. Shortening of sarcomere and contraction of the muscle fibre I. Walk along Theory of contraction OR Ratchet theory of contraction Walk along Theory of contraction The heads of the cross bridges bend back and forth and step by step walk along the actin filament, pulling the ends of the two successive actin filaments towards the center of the myosin filament Greater the number of cross bridges in contact with the actin filament at any given time, the greater is the force of contraction. The attachment of head to the active site of actin causes profound changes in intramolecular forces between head and arm of its cross bridge. The new alignment of forces causes the head to tilt towards the arm and to drag the actin filament This tilt of the head is called “POWER STROKE” Tilting causes detachment of head, it extends back and attaches to another active site Actin and Myosin Interaction SLIDING FIALMENT THEORY Role of calcium and ATP in skeletal muscle contraction Contraction of skeletal muscle requires increase in intracellular calcium Calcium-binding protein (calsequestrin) helps hold calcium ions in SR (Ca+2 concentration 10,000 times higher than in cytosol) ATP is required for the release of myosin head from actin. After death since ATP is no longer available the skeletal muscles of the body remains in sustained contracted state as known as rigor mortis. Sources of energy 1. Phosphocreatine: carrying a high energy Phosphate bond. Immediately cleaved and energy released is used to reconstitute ATP. Along with ATP provide energy for 5 to 8 sec. 2. Glycolysis : of glycogen previously stored in muscle. Formation of pyruvic acid and lactic acid liberates energy, used to convert ADP to ATP ATP is then used directly for muscle contraction and also to reform the stores of phosphocreatine 3. Oxidative metabolism: It is combining of oxygen with end products of glycolysis and with various other cellular foodstuffs like CHO, fats and proteins to liberate ATP. Fast twitch muscles (=IIA or IIB) e.g. lateral rectus muscle II. Slow twitch muscle (=IA) e.g. soleus muscle Fast fibres are used for short time period , their activity is fast but they fatigue quickly Slow fibres are used for sustained activity like maintenance of posture Most muscles contain a mixture of these three fiber function of the muscle. types, and their proportion Types of skeletal muscle fibres depends upon the I. Type I:Slown oxidative (red) Type IIB: fast Type IIA :fast glycolytic oxidative (white) (red) Myosin isoenzyme (ATPase rate) slow fast Fast Sarcoplasmic reticulum calcium pumping capacity Moderate High High Oxidative capacity: mitochondria content, caplillary density, myoglobin high Low Very high Glycolytic activity Moderate High High Diameter Moderate Large Small CHARACTERIS SKELETAL TICS MUSCLES CARDIAC MUSCLE SMOOTH MUSCLE STRUCTURE STRIATED STRIATED NON STRIATED SHAPE CYLINDRICAL CYLINDRICAL SPINDLE SHAPED SARCOTUBULAR SYSTEM PRESENT, T TUBULE AT A-I JUNCTION POORLY DEVELOPED T TUBULE AT Z LINE PRESENT BUT NOT CHARACTERISTIC SARCOPLASMIC RETICULUM DEVELOPED MORE DEVELOPED POORLY DEVELOPED NERVE SUPPLY SOMATIC NERVES AUTONOMIC NERVES AUTONOMIC NERVES CONTROL VOLUNTARY INVOLUNTARY INVOLUNTARY EXCITATION CONTRACTIO N COUPLING RAPID MORE RAPID VERY SLOW I. Muscle fatigue Muscle fatigue is the decline in ability of a muscle to generate force. Fatigue is not the result of depletion of energy stores rather it is due to accumulation of metabolic by products. Accumulation of lactic acid decreases myoplasmic pH and inhibits actin myosin interactions. Fast fibres are more sensitive to the effects of low pH. II. Electromyography Electromyography (EMG) is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph, to produce a record called an electromyogram. An electromyograph detects the electrical potential generated by muscle cells when these cells are electrically or neurologically activated. Denervation When motor nerve to a skeletal muscle is cut it causes i. Disuse atrophy- ultimately fibrous muscle ii. Flaccid paralysis iii. Abnormal excitability of the muscle and its increased sensitivity to circulating acetylcholine III. Thank You