Does Maternal HSV-2 Infection Increase Risk of
advertisement

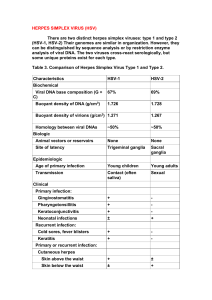
DOES MATERNAL HSV-2 INFECTION INCREASE RISK OF INTRA-PARTUM TRANSMISSION OF HIV-1? Frances M Cowan, Jean Humphrey, Robert Ntozini, Kuda Mutasa, Peter Iliff • Herpes simplex virus type 2 infection • Role of HSV-2 on sexual acquisition and transmission of HIV • How HSV-2 might effect intra-partum HIV transmission • Zvitambo study • Nested case control study to examine the role of HSV-2 in MTCT of HIV • Implications Herpes simplex virus type 2 - the cause of genital herpes Sexually transmitted Commonest cause of genital ulceration Infection may be symptomatic (65%) or asymptomatic (35%) Only one third of those infected are aware of diagnosis Following infection the virus becomes latent, periodically reactivating to cause recurrences. HIV and HSV-2 co-infection results in more frequent and severe recurrences Aciclovir suppresses genital herpes reactivation What explains the variability in rates of HIV infection in Africa? • 4 Cities Study – 2 cities in West Africa (low HIV prevalence) - 2 cities in East Africa (high HIV prevalence) AIDS 2001; 15: S15-30 Yaounde HIV-1: 7% W, 3.6% M HSV-2: 51% W, 27% M Cotonou HIV-1: 2.8% W, 2.8% M HSV-2: 30% W, 12% M Kisumu HIV-1: 29% W, 18% M HSV-2: 68% W 35% M Ndola HIV-1: 32% W, 24% M HSV-2: 55% W, 36% M What explains the variability in rates of HIV infection in Africa? • Circumcision • HSV-2 infection Sexual behavior not very different AIDS 2001; 15: S15-30 HSV-2 and sexual acquisition of HIV-1 • Sexual acquisition of HIV-1 is likely increased by presence of HSV-2 infection (AIDS 2006) • Meta-analysis of 19 studies suggests that prevalent HSV-2 infection increases risk of acquisition in men (adjusted RR 2.7 [95% CI 1.9-3.9]) and women (aRR 3.1 [95% CI 1.7-5.6]. • Studies looking at effect of incident HSV-2 infection are less methodologically sound. • Intervention trials ongoing to see if suppressing HSV-2 infection with antiviral drugs can reduce this risk. (HPTN 039 and Mwanza Herpes Trial) Effect of HSV-2 on sexual transmission of HIV • Much less data than for acquisition • Very few studies on HIV transmission overall • Relatively few events observed • Risk factors: high viral load, more advanced HIV disease or primary disease, Genital Ulcer Disease • Only one study which has looked at effect of HSV-2 on sexual transmission of HIV HSV-2 and sexual transmission of HIV-1 • Genital ulceration increases risk of transmission five fold Per contact risk = 0.0062 vs 0.0012 for those without genital ulceration, p=0.002 • HSV-2 seropositivity per se not associated with increased transmission risk. Lancet 2001;357:1149-53 How does HSV-2 facilitate sexual HIV-1 transmission? • Increased genital shedding of HIV from both clinical and sub-clinical HSV-2 lesions (JAIDS 2003; 33:121-4 . AIDS 2002;16:2425-30) • Possibly by increasing HIV-1 plasma viral load (Nagot et al CROI . 2006) Intra-partum transmission of HIV • Maternal health • Obstetric factors • Infant prematurity • Linear relationship between maternal plasma HIV-1 viral load and risk of transmission Intra-partum transmission - 2 • Role of STIs in intra-partum transmission unclear. • Presumptive treatment of bacterial STIs does not reduce risk of intra-partum transmission. (Am J Ob Gyn 2005;185:1209-17) • No data on whether HSV-2 infection increases risk of intra-partum transmission of HIV-1 • Clinical genital herpes during pregnancy is associated with increased transmission risk (adj OR 4.8 (95%CI 1.317.0). (Obst Gynec 2005;186:1341-8) Pre-ARV era MCTC rates • ACTG 076 - 25.5% (95%CI 18.8-32.5) • European collaborative study - 14.4% (95% CI 12.0-17.1%) • Sub-Saharan Africa 35-50% Rates of HSV-2 vary globally • NHANES 3 - 22% of adults in the USA infected. Higher rates among women and African-American women. • European studies show sero-prevalences of 2-6% (higher in Eastern Europe) • Rates in sub-Saharan Africa are high Seroprevalence of HSV-2 in Tanzania 80 70 60 50 HSV-2 prevelance 40 (%) 30 Female Male 20 10 0 15 16 17 18 19 2024 25- 30- >35 29 34 Age (years) JID 1999; 179:16-24 DOES MATERNAL HSV-2 INFECTION INCREASE RISK OF INTRA-PARTUM TRANSMISSION OF HIV-1? Zvitambo Study Randomised placebo controlled trial Aimed to discover if giving Vitamin A to mothers and babies in the immediate post-partum period i) improved infant mortality ii) reduced risk of mother to child transmission of HIV-1 through breast feeding iii) reduced the risk of women acquiring HIV-1 in the year after delivery. Recruitment took place in Harare, Zimbabwe from November 1997 to January 2000. Trial design • 14,110 mother-baby pairs recruited • Included 4,495 HIV-1 positive mothers • HIV-1 positive mothers and their babies had blood taken at baseline, 6 weeks, 3 months then 3 monthly for 2 years • Where available specimens were archived from each visit Objectives of nested case control study To see if: • women with prevalent HSV-2 infection at delivery had an increased risk of intra-partum transmission of HIV-1; • women who acquired HSV-2 antibodies within 6 weeks of delivery had an increased risk of intrapartum transmission of HIV-1; • women with serological evidence of active syphilis at delivery had an increased risk of intrapartum transmission. • Case control study using archived sera Case control study design Cases: 509 HIV+ve women whose babies were presumed HIV infected intra-partum (baby HIV PCR-negative at delivery and PCR-positive at 6 weeks) Controls: 1018 HIV-positive women whose babies remained PCR-negative at 1 year Power If 80% of controls group are co-infected with HSV-2, the study had > 90% power to detect a 50% increase in the risk of intra-partum transmission. If incidence of HSV-2 is 1% in the control arm the study has 80% power to show that incident HSV-2 increases the risk of intra-partum by a factor >3. Testing strategy • Maternal serum taken within 96 hours of delivery was tested for HSV-2 antibody – HerpeSelect (Focus Diagnostics) – Low +ves / indeterminates re-tested using HerpeSelect – Those remained LP/Ind re-tested using western blot (11%) – Those remained LP/Ind re-tested using Biokit Elisa – Random sample of positives and negatives retested using western blot and Biokit Elisa • 6 week samples were tested for HSV-2 if HSV-2 seronegative at delivery and for syphilis (RPR and TPHA). HSV-2 Testing Flowchart: determination of baseline HSV-2 result 1527 women selected (509 cases and 1018 controls) 18 cases and 23 controls insufficient baseline sample Baseline FocusELISA 1127 193 162 4 positive negative low positive indeterminate BIOELISA Retested by: Western blot & BioELISA W es ter nb lot Missing 4 1 0 0 5 Missing Pos Neg Ind Total Pos 0 41 0 0 41 Neg 0 24 45 15 84 Ind 30 2 0 4 36 Total 34 68 45 19 166 68 60 Final baseline result 1195 253 34 4 positive negative low positive indeterminate Results • Overall 82.5% [95% CI 80.6-84.5] of (HIV positive) women were HSV-2 antibody positive • Baseline Characteristics – Cases were less educated, and had more signs of advanced HIV-1 disease (lower CD4 count, lower haemoglobin, higher viral load, smaller arm circumference) and to have to lower birth weight babies than controls. Effect of prevalent HSV-2 infection • Cases were more likely than controls to be HSV-2 infected (unadj OR 1.49 [95% CI 1.10-2.02, p=0.01]) • Cases were more likely than controls to be HSV-2 infected after adjusting for factors assocd with intrapartum transmission (adj OR1.50 [95% CI 1.09-2.08, p=0.014]) • The proportion of HIV-1 intra-partum transmission potentially attributable to maternal HSV-2 infection at time of delivery was 28.4% [95% CI 7.3-44.7] Sensitivity analyses • Re-analysing data using differing testing algorithms for HSV-2 diagnosis did not change direction of effect but did alter significance of results • HerpeSelect + WB only (unadj OR 1.27 [95% CI 0.91-1.77], p=0.15, adj OR 1.28 [95% CI 0.901.83], p=0.17). • HerpeSelect + BioElisa only, (unadj OR 1.36 [95% CI 1.03-1.80], p=0.03, adj OR 1.31 [95% CI 0.97-1.76], p=0.08]. Effect of ‘incident’ HSV-2 infection • 27 / 158 women who were HSV-2 negative at delivery had ‘seroconverted’ to HSV-2 by 6 weeks (17.3%, 95% CI 11.3-23.3) • ‘Sero-conversion’ was associated with an increased risk of HIV-1 transmission although not significant (unadj OR 1.59 [95% CI 0.67-3.73, p=0.29]; adj OR 1.44 [95% CI 0.57-3.69, p=0.44] Effect of syphilis • 52 of 1289 women had evidence of active syphilis at 6 weeks (4.0%, 95% CI 3.05.1). • Unadj OR of intra-partum transmission associated with syphilis = 0.89 [95% CI 0.49-1.59, p=0.68] • Adj OR 0.63 [95% CI 0.34-1.20, p=0.16] Conclusion • HSV-2 is common among HIV positive women of child bearing age in Zimbabwe • Maternal HSV-2 is associated with an increased the risk of intra-partum transmission of HIV • Maternal seroconversion to HSV-2 is common and needs to be better defined. • Syphilis is not associated with an increased risk of intra-partum transmission of HIV Implications • Adding HSV-2 interventions to existing PMTCT programmes might further reduce intra-partum transmission of HIV • Unlikely to be worthwhile if using HAART but may have a significant impact where PMTCT uses nevaripine only approach • Trial of adding suppressive aciclovir to nevaripine only PMTCT may be warranted?