Bad News Good News: The Basics of Infection Prevention and Control
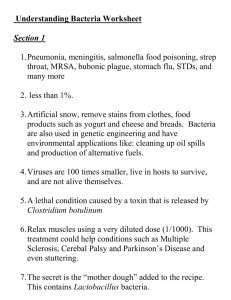
advertisement

Bad News – Good News: The Basics of Infection Prevention and Control July 2012 Judith Conway, RN, BS, CIC Infection Control Coordinator Communicable Disease Control Section Office of Health Protection Illinois Department of Public Health E-mail: judith.conway@illinois.gov Telephone: 217/557-3472 1 Session Overview 1. 2. 3. 4. Fundamental information “Germology terminology” “Antibiotic resistance 101” Chain of infection – routes of infectious disease transmission 5. Brief review of basic infection prevention/control recommendations used to prevent transmission 6. Problematic pathogens 7. Scenarios 2 Fundamental Information • It’s a “bug-drug” war – “Bug” = bacteria – “Drug” = antibiotic • Bad news: Some bacteria have become increasingly resistant to antibiotics • Good news: We can help prevent infectious disease transmission by understanding and applying basic infection prevention/control practices 3 Antibiotic Resistant Germs Antibiotic resistance can travel the globe “Resistance anywhere is resistance everywhere” 4 Welcome to Your New Normal… 5 FUNdamental Information: Pre-Assessment 1) Antibiotics are drugs that fight infections caused by: A) Bacteria B) Viruses C) Bacteria and viruses 2) FILL IN THE BLANKS: ____________ ___________ is the primary strategy recommended by CDC as the foundation to prevent transmission of infectious agents in all healthcare settings. 3) TRUE or FALSE? MRSA is spread by airborne transmission. 6 FUNdamental Information: Pre-Assessment 4) Antibiotic-resistant pathogens are most frequently spread from one patient to another in healthcare settings by: A) B) C) D) Airborne spread resulting from patients coughing and sneezing Patients coming in contact with contaminated equipment The contaminated hands of healthcare workers Substandard environmental maintenance 5) What is the IDPH recommendation for the length of time to perform proper hand washing? 6) TRUE of FALSE? Clostridium difficile is readily killed by alcoholbased hand hygiene products. 7 Is this a good thing or a bad thing? “Germology Terminology” Microorganisms • Microorganisms: bacteria, viruses, fungi, protozoa, helminths, rickettsia, prions – Biologic agents capable of causing disease – Also known as infectious agents or pathogens – Commonly called “germs” or “bugs” NOTE: In today’s session, we will focus exclusively on bacteria 9 “Germology Terminology” Infection versus Colonization • Infection: Bad news, bad news, bad news – Bad news: You’ve got it (it = bacteria “X”) – Bad news: It’s making you sick (invading your tissues and cells) – Bad news: It can be spread to others • Colonization: Bad news, good news, bad news – Bad news: You’ve got it (it = bacteria “X”) – Good news: It’s not making you sick – Bad news: It can be spread to others 10 Antibiotic Resistance 101 • What are antibiotics? –Drugs used to fight infections caused by bacteria • It is important to remember that antibiotics have no effect on viruses • How do antibiotics work? –2 main types of action • Bacteriostatic: inhibit bacterial growth • Bactericidal: kill bacteria 11 Antibiotic Resistance 101 • What is antibiotic resistance? –Ability of bacteria to resist the effects of an antibiotic • How does it occur? –Occurs when bacteria change in some way that reduces or eliminates the effectiveness of antibiotics • Because the antibiotic isn’t effective, the bacteria survive and continue to multiply and cause harm 12 Antibiotic Resistance 101 • How do bacteria become resistant to antibiotics? –Bacteria have several mechanisms • Some bacteria develop the ability to neutralize the antibiotic • Other bacteria rapidly pump out the antibiotic • Still other bacteria change the antibiotic attack site (on the bacterial cell wall) so that the antibiotic can’t do its work of affecting bacterial metabolism • Additionally, some bacteria can transfer pieces of DNA that code for resistance to other bacteria 13 Antibiotic Resistance 101 • What happens when bacteria become resistant to antibiotics? –Selective pressure: resistant bacteria survive, multiply, and replace all the sensitive (susceptible) bacteria that were killed off –Just like antibiotic-susceptible bacteria, resistant bacteria can spread to other people and cause colonization or serious infections 14 Antibiotic Resistance 101 • Why are bacteria becoming resistant to antibiotics? – Antibiotic use promotes development of antibiotic-resistant bacteria • Every time a person takes antibiotics, sensitive (susceptible) bacteria are killed, but resistant bacteria may be left to grow and multiply – Overuse and misuse • Antibiotics are not effective against viral infections 15 Chain of Infection Causative Agent Mode of Transmission 16 Chain of Infection: Modes of Transmission • Microorganisms are spread through 3 primary routes: –AIRBORNE –DROPLET –CONTACT • Direct contact • Indirect contact 17 Airborne Spread • Least common mode of transmission • Dissemination of airborne droplet nuclei (small-particle residue [5 microns or smaller in size] of evaporated droplets that contain the infectious pathogen and remain suspended in the air) or dust particles containing the infectious pathogen • Examples of diseases spread through airborne transmission: – – – – – – – – Anthrax spores from contaminated environment Chickenpox Disseminated herpes zoster (shingles) Measles (rubeola) Novel Strain Influenza: airborne spread may occur, extent unknown Severe Acute Respiratory Syndrome (SARS) Smallpox Tuberculosis 18 Droplet Spread • Pathogen is spread in large respiratory droplets that don’t stay suspended in the air; they travel about 3 - 6 feet and then drop to the ground/surfaces • Studies have shown that the nasal mucosa and conjunctivae (and, less frequently, the mouth) are susceptible portals of entry for respiratory viruses • Examples of diseases spread through droplet transmission: – Influenza (seasonal influenza) – Meningococcal Meningitis – Mumps – Pertussis (Whooping cough) – Rubella (German measles) – Severe Acute Respiratory Syndrome (SARS) 19 Contact Spread • Most common mode of transmission • Direct contact: germs (microorganisms) are transferred directly from one person to another person through physical contact • Indirect contact: transferred from contact with a contaminated item or contaminated hands • Short list of examples of diseases spread through contact transmission: – Chickenpox – C. diff – Lice – MRSA and other multidrug-resistant organisms (MDRO) – Norovirus – Scabies – Smallpox 20 Chain of Infection: Preventing Transmission CDC recommended these isolation precautions in 1996: • Standard Precautions • Transmission-based Precautions –Airborne Precautions –Droplet Precautions –Contact Precautions 21 Standard Precautions • Primary strategy recommended by CDC as the foundation to prevent transmission of infectious agents in all healthcare settings • Basic level of infection prevention/control practices to be used in the care of all patients at all times and in all healthcare settings, regardless of suspected or confirmed infection – Intended to reduce the risk of transmission of bloodborne and other pathogens from recognized and unrecognized sources of infection – Designed to both protect the healthcare worker and prevent the healthcare worker from spreading infections among patients 22 Standard Precautions • Five components of Standard Precautions: 1. Hand hygiene before and after touching a patient 2. Personal protective equipment (PPE) (gloves, gowns, face protection [masks, goggles, face shields]) is used as indicated to prevent exposure to blood, body fluids, secretions, and excretions (except sweat), mucous membranes, non-intact skin, or contaminated equipment 3. Safe injection practices (recommended in 2007) • One & Only campaign: ONE needle, ONE syringe, ONLY ONE time 4. Safe handling of potentially contaminated equipment or surfaces in the patient environment 5. Respiratory hygiene/cough etiquette (recommended in 2007) • Cover Your Cough 23 24 Alcohol-Based Hand Hygiene Products “Alcohol-based products are more effective for standard handwashing or hand antisepsis by healthcare workers (HCW) than soap or antimicrobial soaps… In studies examining antibiotic-resistant organisms, alcohol-based products reduced the number of multidrugresistant pathogens recovered from the hands of HCWs more effectively than did hand washing with soap and water.” SOURCE: CDC Hand Hygiene Guideline, 2002; page 11. 25 Respiratory Hygiene/Cough Etiquette 26 Who, What, Where, When, & Why • WHO: On whom is the Precaution(s) used? • WHAT: What type of personal protective equipment is used by healthcare worker(s)? • WHERE: Where is the patient placed in the hospital or LTCF? • WHEN: When is the Precaution(s) used? • WHY: Why is the Precaution(s) used? 27 Standard Precautions • WHO: All patients in all healthcare settings • WHAT: Hand hygiene and PPE: healthcare workers have clean hands and use of appropriate personal protective equipment (gloves, gown, face protection) as indicated by the nature of the interaction and the extent of anticipated blood, body fluid etc. exposure • WHERE: No special room placement is required • WHEN: During all healthcare encounters • WHY: Prevent transmission of bloodborne and other pathogens from recognized and unrecognized sources of infection 28 Airborne Precautions • WHO: Patient with known or suspected infection with airborne infectious agent • WHAT: Respirator and AIIR: healthcare workers will wear respiratory protection (respirator) upon entry into patient’s Airborne Infection Isolation Room (AIIR) • WHERE: Airborne Infection Isolation Room (AIIR): patient is placed in a room with special air handling and ventilation capacity (negative air pressure) • WHEN: During hospitalization or LTCF stay while patient is known/suspected to be contagious • WHY: Prevent transmission of airborne infectious agents 29 Droplet Precautions • WHO: Patient with known or suspected infection with droplet-spread infectious agent • WHAT: Mask: healthcare workers will wear mask upon room entry / when working within 6 feet of patient • WHERE: Private room: patient is placed in a private room, if available. Special air handling and ventilation capacity are NOT required or indicated. • WHEN: During hospitalization or LTCF stay while patient is known/suspected to be contagious • WHY: Prevent transmission of infectious agents spread through close respiratory or mucous membrane contact with infectious respiratory secretions 30 Contact Precautions • WHO: Patient with known or suspected infection with contact-spread infectious agent • WHAT: Gown and gloves: healthcare workers will wear gown and gloves for all interactions that involve contact with patient • WHERE: Private room: patient is placed in a private room, if available. Special air handling and ventilation capacity are NOT required or indicated. • WHEN: During hospitalization or LTCF stay while patient is known/suspected to be contagious • WHY: Prevent transmission of infectious agents spread through direct or indirect contact 31 How to Safely Don & Remove PPE • The addddddition of a mask for certain spinal procedures grew from recent evidence of an associated risk for developing meningitis caused by respiratroy flora • The use of a mask when performing certain high-risk, prolonged procedures involving spinal canal punctures (e.g., myelography, epidural anesthesia) 32 Problematic Pathogens 33 Clostridium difficile a.k.a. C. diff • Bacteria: spore-forming bacteria • Toxin-producer: produces exotoxins (toxin A and toxin B) that are pathogenic to humans • Exotoxins: toxin A and toxin B • Illness: diarrhea (known as Clostridium difficile infection – CDI) – Can also cause serious intestinal conditions, sepsis – CDC estimates that 14,000 deaths occur annually due to CDI Main Symptoms of CDI • • • • • Watery diarrhea Fever Loss of appetite Nausea Abdominal pain/tenderness Public Health definition of diarrhea: 3 or more loose stools within a 24-hour period Risk Factors for CDI • • • • • • • Antibiotic exposure Proton pump inhibitors Gastrointestinal surgery/manipulation Long length of stay in healthcare settings Serious underlying illness Immunocompromising conditions Advanced age CDI: New Difficulties With an Old Pathogen • Nationwide, increased rates of CDI, with more severe disease and increased mortality • Possible reasons include the emergence of a new strain of C. diff with increase virulence and/or antibiotic resistance – New strain has increased production of toxins A and B, and can produce an additional toxin known as binary toxin CDI: Healthcare Facility Infection Control • Contact Precautions for patients with known or suspected CDI – Soap & water hand hygiene; alcohol doesn’t kill spores • Continue Contact Precautions until diarrhea ceases and patient has been diarrhea-free for 3 days • Ensure adequate cleaning and disinfection of environmental surfaces, especially items likely to be contaminated with feces – During outbreaks, use a bleach-based disinfectant or an EPA-registered disinfectant with a sporicidal claim Multidrug-Resistant Organisms • Multidrug-resistant organisms (MDRO) are microorganisms, predominantly bacteria, that are resistant to 1 or more classes of antibiotics • In some cases, the microorganisms have become so resistant that no available antibiotics are effective against them 39 Facts About MDRO Transmission • Transmitted by the same routes as antibiotic susceptible infectious agents • Patient-to-patient MDRO transmission in healthcare settings is usually via contaminated hands of healthcare workers • Contact Precautions are recommended to prevent MDRO transmission in healthcare settings 40 MRSA in the 21st Century 41 What is Staphylococcus aureus? • Bacteria often referred to as “Staph” • Carried on the skin or in the nose of healthy people – Approximately 30% of the population carry it on the skin or in the nose – Approximately 2% carry a type known as MRSA 42 What Is MRSA? • MRSA stands for Methicillin-Resistant Staphylococcus aureus • It is a type of Staph bacteria that is resistant to certain antibiotics including penicillin, methicillin, and amoxicillin • HA-MRSA stands for healthcare-associated MRSA • CA-MRSA stands for community-associated MRSA 43 MRSA Infection • In the community, most MRSA infections are skin infections • In healthcare settings, more severe or potentially life-threatening infections may occur among patients e.g., bloodstream infection, pneumonia, surgical site infection, urinary tract infection • MRSA is spread by contact transmission 44 ESBL-Producing Bacteria • ESBL = Extended-Spectrum Beta-Lactamase • Beta-lactams are a class of antibiotics • Beta-lactamase is an enzyme that deactivates the antibiotics • ESBLs are enzymes that confer resistance to a broad (extended) spectrum of beta-lactam antibiotics & third and fourth generation cephalasporins • ESBL-producing bacteria have been identified in E. coli, and also in Klebsiella, Proteus, Pseudomonas, Salmonella, and Serratia species • ESBL-producing bacteria are spread through contact transmission 45 Carbapenem Resistance and Carbapenemase-Producing Bacteria • Carbapenems: a class of beta-lactam antibiotics (imipenem, meropenem, ertapenem, doripenem) • Carbapenems have been used as a last line of defense in treating infections caused by ESBL-producing bacteria • Some bacteria have developed the ability to produce carbapenemase which is an enzyme that deactivates carbapenem antibiotics – KPC refers to Klebsiella pneumoniae carbapenemase – CRE refers to carbapenem-resistant Enterobacteriaceae • KPC / CRE are spread through contact transmission 46 Bad News • Antibiotic resistance is one of the world’s most pressing public health threats • Antibiotic overuse increases the development of drug-resistant germs • It will be many years before new antibiotics are available to treat some resistant infections • Klebsiella pneumoniae carbapenemase (KPC) infection -- a type of antibiotic resistant bacteria also known as CRE -- is found in 37 states • Resistance anywhere is resistance everywhere – Antibiotic resistance can travel the globe (Information source: CDC Web site “Get Smart for Healthcare”) 47 CDC: 2011 Location of CRE Caused by KPC Enzyme; CRE Caused by Other Enzymes Noted 48 Good News • Many healthcare facilities are making infection prevention a patient safety priority • Implementation and correct adherence to Standard Precautions, and Contact Precautions when indicated, are “low-tech” practices that help prevent MDRO transmission • CDC has launched educational programs and campaigns to promote the proper use of antimicrobial agents 49 FUNdamental Information: Knowledge Assessment 1) Antibiotics are drugs that fight infections caused by A) Bacteria B) Viruses C) Bacteria and viruses BACTERIA. 2) FILL IN THE BLANKS: ________ _________ is the primary strategy recommended by CDC as the foundation to prevent transmission of infectious agents in all healthcare settings. Standard Precautions 1) TRUE or FALSE? MRSA is spread by airborne transmission. FALSE: MRSA is spread by contact transmission. 50 FUNdamental Information: Knowledge Assessment 4) Antibiotic-resistant pathogens are most frequently spread from one patient to another in healthcare settings by A) Airborne spread resulting from patients coughing and sneezing B) Patients coming in contact with contaminated equipment C) The contaminated hands of healthcare workers D) Substandard environmental maintenance The contaminated hands of healthcare workers 5) What is the IDPH recommendation for the length of time to perform proper hand washing? 20 seconds of scrubbing 6) TRUE of FALSE? Clostridium difficile is readily killed by alcoholbased hand hygiene products. FALSE: alcohol doesn’t kill spores 51 Is this a good thing or a bad thing? Is this a good thing or a bad thing? Is this a good thing or a bad thing? Is this a good thing or a bad thing? Is this a good thing or a bad thing? 56 Is this a good thing or a bad thing? (Don’t be alarmed! This photo was staged – it’s not really blood!) 57 Is this a good thing or a bad thing? Is this a good thing or a bad thing? Concluding Comments 60