Masters 2.pptx
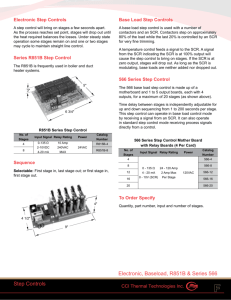
advertisement

Evaluation of Polymyxin B Toxicodynamics & Development of an Adaptive Feedback Control Algorithm ELIZABETH A. LAKOTA, PHARM.D., M.S. CANDIDATE ADVISOR: ALAN FORREST, PHARM.D. Background Polymyxins -Group of antibiotics discovered in 1947 -Spectrum of coverage: Gram negative aerobes (except proteus) -Parenteral polymyxin B and polymyxin E (colistin) used clinically -Associated with significant nephrotoxicity -Used until late 1960s when aminoglycosides came to market Polymyxins -Significant increase in multidrug resistant organisms over past decade -Polymyxins reemerged in clinical practice -Few to zero other therapeutic alternatives in many situations -Polymyxin B may be less nephrotoxic than colistin -Often used in critically ill patients ◦ Narrow therapeutic window Objectives Objectives 1. Determine an target AUC window for polymyxin B ◦ Lower edge pre-determined, focus on upper edge (toxicodynamics) 2. Develop an adaptive feedback control (AFC) algorithm to increase target attainment Methods Part 1 DEVELOPING POLYMYXIN B TARGET WINDOW Therapeutic Window for Polymyxin B - AUC/MIC drives polymyxin B efficacy - AUC, duration of treatment, and baseline CLcr drive colistin nephrotoxicity - Polymyxin B nephrotoxicity related to dose and duration of treatment - Lower edge pre-determined to be 50 mg·h/L (ssAUC0-24h) ◦ Based on preclinical animal data ◦ Free drug ssAUC0-24h/MIC values of 24.7 mg·h/L and 22.5 mg·h/L needed murine lung and thigh studies ◦ Plasma protein binding in humans ~50% ◦ Css ~ 2 mg/L needed for efficacy (unpublished data) Dudhani et al., J. Antimicrob. Chemother., 65(9):1984-90, 2010 Upper Edge of Therapeutic Window Toxicodynamic Meta-Analysis 1. Data from literature gathered using search terms ‘polmyxin’, ‘polymyxin B’, ‘nephrotoxicity’, ‘adverse event’, and ‘toxicity’ 2. Data collected from each study: number of subjects, definition of nephrotoxicity, number of nephrotoxicity events, dosing guidelines used, statistics on the doses patients received, and statistics on weight 3. Excluded if dosing or rates of nephrotoxicity unclear or not provided Toxicodynamic Meta-Analysis - Monte Carlo Simulation of 1000 subjects for each study - Steady state AUC0-24h simulated: ssAUC0-24h=Dose24h/CL ◦ CL(L/h)=0.0276*WT, BSV=32.4% - Nephrotoxicity rates unified into 3 categories: > 25%, > 50%, and > 75% decrease in CLcr - Regression analyses used to evaluate data Sandri et al., Clin. Infect. Dis., 57(4):524-531, 2013 Results Part 1 DEVELOPING POLYMYXIN B TARGET WINDOW Toxicodynamic Meta-Analysis - Total of 16 articles collected, 2 excluded - Publication dates ranged from 2003-2013 - Number of study subjects ranged from 11-235 ◦ Total subjects 971 - Mean/median daily polymyxin b dose ranged from 62.9-200 mg/day Results of ssAUC0-24h Simulations Author (year) Ouderkirk et al. (2003) Holloway et al. (2006) Teng et al. (2007) Pastweski et al. (2008) Ramasubban et al. (2008) Mendes et al. (2009) Oliveira et al. (2009) Elias et al. (2010) Kvitko et al. (2011) Esaian et al. (2012) Kubin et al. (2012) Toun et al. (2013) Mandal et al. (2013) Akajagbor et al. (2013) Median (Min-Max) 25th Percentile AUC (mg·h/L) 43.1 47.7 28.5 48.1 46.6 37.5 35.8 49.4 51.1 46.8 45.3 52.5 39.3 47.6 46.7 (28.5-52.5) 50th Percentile AUC (mg·h/L) 57.4 67.4 42.4 48.1 59.7 50.8 51.0 77.1 75.7 54.2 62.2 76.8 57.0 62.3 58.6 (42.5-77.1) 75th Percentile AUC (mg·h/L) 73.9 90.6 58.9 60.1 81.0 70.2 69.2 116.6 108.0 67.6 88.0 105.3 79.8 76.4 78.1 (60.1 – 117) Results of ssAUC0-24h Simulations Author (year) Ouderkirk et al. (2003) Holloway et al. (2006) Teng et al. (2007) Pastweski et al. (2008) Ramasubban et al. (2008) Mendes et al. (2009) Oliveira et al. (2009) Elias et al. (2010) Kvitko et al. (2011) Esaian et al. (2012) Kubin et al. (2012) Toun et al. (2013) Mandal et al. (2013) Akajagbor et al. (2013) Median (Min-Max) 25th Percentile AUC (mg·h/L) 43.1 47.7 28.5 48.1 46.6 37.5 35.8 49.4 51.1 46.8 45.3 52.5 39.3 47.6 46.7 (28.5-52.5) 50th Percentile AUC (mg·h/L) 57.4 67.4 42.4 48.1 59.7 50.8 51.0 77.1 75.7 54.2 62.2 76.8 57.0 62.3 58.6 (42.5-77.1) 75th Percentile AUC (mg·h/L) 73.9 90.6 58.9 60.1 81.0 70.2 69.2 116.6 108.0 67.6 88.0 105.3 79.8 76.4 78.1 (60.1 – 117) Portion of Subjects with >50% Decrease in CLCr 0.140 0.261 0.266 0.370 0.244 0.310 0.20 0.0938 0.0313 0.284 0.264 (0.0313 – 0.370) Toxicodynamic Results Methods Part 2 ADAPTIVE FEEDBACK CONTROL (AFC) ALGORITHM DEVELOPMENT Inf CLD C1 V2 V1 Population PK Model - Linear 2 compartment model C2 CL ◦ Total body weight as covariate ◦ Tested covariates: TBW, LBW, sex, age, CLcr, albumin, APACHE II score Parameter CL (L/h/kg) V1 (L/kg) V2 (L/kg) CLD (L/h/kg) SDintercept (mg/L) SDslope Population Estimate Between Subject Variability (%CV) Standard Error (%SE) 0.0276 0.0939 0.330 0.146 0.0392 9.59% 32.4 73.3 70.1 50.4 7.49 23.6 19.5 22.2 Sandri et al., Clin. Infect. Dis., 57(4):524-531, 2013 Sampling Strategies -Optimal sparse sampling strategies on day 1 determined -Andi et al population PK model used with 2.5 mg/kg loading dose following by 1.25 mg/kg q12h -D-optimality criterion in ADAPT-5 evaluated -Generalized linear regression approach also evaluated Simulations with AFC -Monte Carlo Simulations of 5000 subjects with PK samples at proposed times - Concentrations simulated with sampling error (10%) -Sandri et al population PK model was used as a MAP-Bayesian PK estimator in ADAPT-5 -New doses calculated for each simulated subject - New Dose = estimated CL · 75 mg·h/L (middle of target ssAUC0-24h) -ssAUC0-24h computed for each subject based on new dose and true clearance -Probability of target attainment determined for each sampling scheme Results 2 ADAPTIVE FEEDBACK CONTROL (AFC) ALGORITHM DEVELOPMENT Sparse Sampling Strategies D-optimality: 2h, 4h, 12h when constrained between 2 -12h 2h, 4h, 12h, 24h when constrained between 2-24h Generalized Linear Model Approach: Number of Samples Sample Time Variability in ssAUC0-24h Explained 1 24h 82.5% 2 12h,24h 88.5% 3 4h,12h,24h 90.5% Adaptive Feedback Control Simulations Adaptive Feedback Control Simulations Number of Samples 0 1 1 2 2 2 2 3 3 3 4 Time of Samples 12 h 24 h 2, 12 h 2, 24 h 4, 24 h 12, 24 h 2, 4, 12 h 4, 12, 24 h 2, 12, 24 h 2, 4, 12, 24 h Probability of Target Attainment 71.0% 93.6% 95.3% 92.2% 96.5% 97.7% 98.5% 93.7% 99.5% 99.2% 99.3% % Above Target % Below Target 19.8% 5.0% 2.5% 4.6% 1.6% 1.7% 0.9% 4.1% 0.04% 0.5% 0.6% 9.2% 1.4% 2.2% 3.1% 1.9% 0.6% 0.6% 2.2% 0% 0.3% 0% Variability in ssAUC0-24h (CV%) Range of Adjusted Doses (mg/kg) 32.0% 17.8% 17.4% 19.1% 14.8% 12.5% 12.0% 17.5% 10.6% 11.1% 10.6% 2 0.77-4.6 0.83-4.4 0.52-4.8 0.66-4.9 0.65-5.5 0.67-5.3 0.50-5.2 0.64-6.8 0.68-5.0 0.71-5.8 Summary - Proposed target ssAUC0-24h window is 50-100 mg·L/h - Better studies/data needed - Window will need to be updated - Target attainment for polymyxin B without AFC is 71% - Developed AFC algorithm can improve target AUC attainment in silico >93% with just 1 sample - AFC algorithm needs to be tested in humans (future plans) Thank You Dr. Alan Forrest – Project Mentor and Advisor Dr. Donald Mager – Committee Member Dr. Gauri Rao Peter Bloomingdale, Veena Thomas, Vidya Ramakrishnan Department of Pharmaceutical Sciences Faculty The Institute for Clinical Pharmacodynamics Family & Fiancé Polymyxin B vs Colistin Nephrotoxicity 106 colistin, 47 polymyxin B patients Akajagbor et al., Clin. Infect. Dis., 2013;57(9):1300-1303, 2013 36 colistin, 96 polymyxin B patients Tuon et al. Int J Antimicrob Agents., 43(4):349-352, 2014 RIFLE Criteria Studies Used in Meta-Analysis 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Ouderkirk et al. Antimicrob Agents Chemother. 2003;47(8):2659-2662. Holloway et al. Ann Pharmacother. 2006;40(11):1939-1945. Teng et al. Int J Antimicrob Agents. 2008;31(1):80-82. Pastewski et al. Ann Pharmacother. 2008;42(9):1177-1187. Ramasubban et al. Indian J Crit Care Med.2008;12(4):153-157. Mendes et al. Ann Pharmacother. 2009;43(12):1948-1955. Oliveira et al. Diagn Microbiol Infect Dis.2009;65(4):431-434. Elias et al. Antimicrob Agents Chemother. 2010;65(10):2231-2237. Kvitko et al. J Antimicrob Chemother. 2011;66(1):175-179. Esaian et al. Ann Pharmacother. 2012;46(3):455-456. Kubin et al. J Infect.2012;65(1):80-87. Tuon et al. Int J Antimicrob Agents. 2014;43(4):349-352. Nandha et al. Indian J Crit Care Med. 2013;17(5):283-287. Akajagbor et al. Clin Infect Dis. 2013;57(9):1300-1303. Author (year) Comorbidities Mechanical Ave Age Sex Ventilation (years) (%M) Site of Infection Infecting Organism Other Nephrotoxic Agents Mortality 50% cardiac, Ouderkirk et 23% cancer, 18% al. (2003) DM, 18% AIDs 95% 61 65% 65% lung 65% A. Baumannii 47% aminoglycoside 70% vancomycin 20% Holloway et al. (2006) APACHE II Score 17 (7-38) N/A 41 78% 50% lung, 43% BSI 100% A. Baumannii 14% aminoglycoside 27% Teng et al. (2007) 48% cardiac, 26% DM N/A 63 59% 41% lung 78% A. Baumannii N/A 30% Pastweski et al. (2008) 73% cardiac, 55% DM 64% vancomycin 9% amphotericin 36% 62% aminoglycosides 16% vancomycin 52% 24% aminoglyc., 48% vanc., 21% amphotericin 62% 75% vancomycin 7% amphotericin 61% Ramasubban 29% cancer, 13% et al. DM (2008) Mendes et al. (2009) Oliveira et al. (2009) 32% cardiac, 25% DM APACHE II Score 16 (6-31) N/A 84% 72 53 54% N/A 56% 49% lung, 22% surgical wound 92% 69 67% 42% urinary, 27% lung 90% 64 45% 44% BSI, 42% lung 36% A. Baumannii 27% P. Aeruginosa 27% K. Pneumoniae 42% A. Baumannii 44% P. Aeruginosa 11% A. Baumannii 83% P. Aeruginosa 100% A. Baumannii Mechanical Ave Age Sex Ventilation (years) (%M) Site of Infection Infecting Organism Other Nephrotoxic Agents Mortality 59% 76% lung, 22% urinary 31% A. Baumannii 46% P. Aeruginosa N/A 61% 62 60% 38% lung, 20% intra-abd 100% P. Aeruginosa N/A 67% 69 53% 34% lung, 16% urinary 23% A. Baumannii 55% K. Pneumoniae 15% aminoglycosides 62% lung 26% A. Baumannii 33% P. Aeruginosa 45% aminoglyc., 71% vanc., 5% amphotericin 11% aminoglycoside, 55% vancomycin, 7% amphotericin 47% Author (year) Comorbidities Elias et al. (2010) 48% cardiac, 32% pulm, 30.4% neuro 67% 59 Kvitko et al. (2011) cardiac 33%, neuro 31%, DM 26% 62% Esaian et al. (2012) DM 36%, COPD 24% 41% Kubin et al. (2012) Lung 38%, DM 33%, cardiac 30% 56% 58 55% 34% N/A Toun et al. (2013) Charlson Score 0 N/A 47 61% 40% lung 32% A. Baumannii 16% P. Aeruginosa Nandha et al. (2013) APACHE II 13 N/A 49 53% 38% BSI, 28% intra-abd 82% A. Baumannii None given 28% Akajagbor et al. (2013) Cardiac 34%, DM 33% N/A 53 44% 50% lung, 13% mixed sites 77% A. Baumannii 23% P. Aeruginosa 22% aminoglycoside 57% vancomycin N/A Author (year) Number of Subjects Institution PMB Dosing Recommendations Daily Poly B Doses (mg/day) Weight (kg) Nephrotoxicity Definition Nephrotoxicity Incidence Ouderkirk et al. (2003) 50 1.5-2.5 mg/kg/day Mean 110 N/A 2 fold ↑ in SCr to > 2 mg/dL 14% N/A 1.5 fold ↑ in SCr, ↑ in SCr of > 0.5 mg/dL , or 50% reduction in CLCr 22.5% 18.5% Holloway et al. (2006) 31 N/A Median 130 Teng et al. (2007) 27 N/A Mean 62.9 N/A 1.5 fold ↑ in SCr, increase in SCr of > 0.5 mg/dL , or 50% reduction in CLCr Pastweski et al. (2008) 11 1.5-2, 1.25 if CLCr 30-80, 0.5 if CLCr <30 Mean 84 N/A ↑ in SCr of > 0.5 mg/dL , or 50% reduction in CLCr 54.5% Ramasubban et al. (2008) 45 1.5-2 mg/kg/day Mean 120 N/A ↑ in SCr by 0.5 mg/dL 8.89% 21.9% Mendes et al. (2009) 114 N/A Mean 96.7 N/A If baseline SCr <1.5, when SCr ↑ to > 1.8. If baseline SCr >1.5, 1.5 fold ↑in SCr Oliveira et al. (2009) 30 N/A Median 100 N/A 2 fold ↑ in SCr or ↑ in SCr of >1 if initial SCr > 1.4 mg/dL 27% N/A Mild: 50-100% ↑ SCr, Mod: >/=100% ↑ SCr but no dialysis, Severe: dialysis Mild: 13.6%, Mod: 26.4%, Severe: 21.9% Elias et al. (2010) 235 N/A Median 150 Author (year) Number of Subjects Institution PMB Dosing Recommendations Daily Poly B Weight Doses (mg/day) (kg) Nephrotoxicity Definition Nephrotoxicity Incidence Kvitko et al. (2011) 45 N/A Mean 141 N/A Stage 1: 1.5-2 fold ↑ in SCr Stage 2: > 2 fold ↑ in SCr Stage1: 11% Stage 2: 24% Esaian et al. (2012) 115 1.5-2.5 mg/kg/day, adjust for renal dysfunction Median 100 Median 69 Meeting any of the RIFLE Criteria Risk 48%, Injury 31%, Failure 17% Kubin et al. (2012) 73 2.5-3, 1-1.5 if CLCr < 80mg/mL Median 180 Median 76.4 Meeting any of the RIFLE Criteria Risk 27.4%, Injury or Failure 20% Stage 1 11.5%, Stage 2 8.33%, Stage 3 1.04% Toun et al. (2013) 96 N/A Median 200 N/A Stage 1: 1.5 -2 fold ↑ SCr or SCr ↑ of 0.3. Stage 2: 2-3x ↑ in SCr. Stage 3: >3x ↑ in SCr or SCr > 4 w/acute rise > 0.5 Nandha et al. (2013) 32 1.5-2.5 Mean 111 N/A Meeting any of the RIFLE Criteria Risk 18.8%, Injury 15.6%, Failure 3.13% Akajagbor et al. (2013) 67 1.5-2 Median 123 Median 74 Meeting any of the RIFLE Criteria Risk 13.4%, Injury 19.4%, Failure 8.96% Kidney Risk Plots Kidney Injury Plots Kidney Failure Plots Population PK Model Details -24 subjects total -Doses ranged from 0.45-3.38 mg/kg/day administered as short term infusions (60-240 minutes) every 12 hours -8 blood samples per subjects - Pre-dose, 5 min, and 0.5, 1, 2, 4, 8, & 12 h after end of the infusion -Urine collected for 17 subjects -S-ADAPT platform, MCPEM algorithm used -AUC0-24h = 66.9 +/- 21.6 mg·h/L (range 16.4-117) -Fraction bound = 0.42 (range 0.26-0.64) -Median % excreted unchanged in urine: 4.04% (range 0.98-17.4%) Sandri et al., Clin. Infect. Dis., 57(4):524-531, 2013 Population PK Model Details Adaptive Feedback Control