A. 1. 2.
advertisement

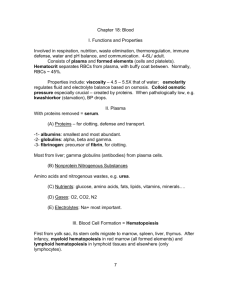
Physiology 31 Lecture Chapter 16 – Blood I. Overview A. Functions & Properties of Blood B. Plasma & Cellular Elements of Blood 1. Red Blood Cells 2. White Blood Cells 3. Platelets F. Blood Cell Production G. Blood Disorders H. Platelets & Coagulation II. Functions & Properties of Blood A. Transportation 1. Respiratory - RBCs pick up _______ from the lungs and take it to tissue cells for aerobic respiration. ______ from cellular respiration is carried in blood back to lungs for elimination. 2. Nutritive - blood carries digested _______ molecules through the liver to the body’s cells. 3. Excretion - metabolic _______, excess water & ions are filtered through kidney capillaries into tubules and excreted in urine. 4. Regulatory a. Blood carries _________ from endocrine glands to target tissues. b. Blood ____ is maintained via a buffering system in blood. c. Body ______________ is regulated via blood’s high water content. B. Protection 1. ___________ – platelet factors initiate clotting and minimize blood loss 2. ____________ – blood plays several roles 3. _____________ and other plasma proteins neutralize or destroy pathogens 4. ______________ – leukocytes (WBCs) destroy microorganisms and cancer cells III. Plasma & Cellular Elements of Blood A. ______________ is the study of blood, blood forming tissues, and their pathology. B. Total blood volume in the body is between ___-__ L C. Blood consists of: 1. _________ - the watery portion of blood (55% of whole blood) 2. Formed Elements (45% of blood) include erythrocytes (_____s), leukocytes (_____s), and platelets (thrombocytes) suspended in the plasma D. Normal blood parameters include 1. Blood is warm at 37C (_____F) 2. Blood has a pH range of ____-_____ 2 3. Salinity (mainly NaCl) is about ____% 4. Osmolarity (total molarity of dissolved particles) of blood is about _____ mOsm/L a. Osmolarity regulates the exchange of __________ and ______ across capillary walls to and from surrounding tissues b. If blood osmolarity is too high (______tonic), too much fluid enters the blood vessels, resulting in ______ BP c. If blood osmolarity is too low (______tonic), too much fluid remains in the tissues, resulting in edema and _____ BP 5. ______________ (resistance of flow due to cohesion between a fluid’s particles) of blood is 4.5-5.5 times the viscosity of water a. Viscosity of blood is due to RBCs and plasma ___________ b. RBC or protein ___________ causes blood to flow too rapidly c. __________ RBC or protein content causes slow blood flow d. Either problem can lead to serious ______________ problems e. Kwashiorkor syndrome is a condition in children who have severe dietary _____________ deficiencies; symptoms are thin arms and legs and a distended abdomen D. Blood ______ - watery portion of blood, composes 55% of blood; consists of about 90% ______ and 10% solutes. _______ include: 1. Plasma __________ - 7% of solutes; 3 major types produced by the ________ are: a. ___________ (60%) - small protein that makes blood viscous to maintain blood ___________, flow, and fluid balance b. ___________ (36%) proteins include globulin, globulin (transport lipids), and gamma globulin (build antibodies) c. _________ (4%) - a protein precursor for fibrin, essential for blood clotting. (________ is plasma without clotting factors) 2. _______________ (immunoglobulins) - proteins produced by plasma cells derived from B lymphocytes, function in immunity 3. Nonprotein nitrogenous substances, such as amino acids and nitrogenous wastes (e.g., urea), the breakdown products of __________ 4. Nutrients – _______, amino acids, lipids, vitamins and minerals 5. _________ – oxygen and CO2 6. Electrolytes – ions such as ____, Cl-, K+, H+, Ca2+ and HCO37. Other plasma solutes include enzymes and _____________. IV. ___________ (RBCs) compose __% of all formed elements in blood A. A mature RBC is a biconcave disc, 7-8 m wide, that lacks a __________ and most organelles (thus is not able to divide) B. Adults have about 5 _____________ RBCs per cc of blood C. RBCs regenerate from red bone _________ at rate of 2 mil./sec. D. Contain Hemoglobin (___) - composed of ______ protein, usually consisting of 2-alpha & 2-beta polypeptide chains, and 4 _____ (red pigment) groups, each of which contains an ______ ion 1. Hb can combine with oxygen (____hemoglobin) and transport it to cells via the blood stream, or with 3 2. CO2 (__________hemoglobin) for transport away from cells. 3. Glucose binds to hemoglobin, forming _______hemoglobin (HbA1C). An assay of HbA1C can determine a diabetic’s average blood _______ level over the past 2-3 months to assess treatment. E. RBCs also contain __________ anhydrase (CAH) enzyme that catalyzes the reaction: CO2 + H2O H2CO3 F. RBCs live about ____ days, then are recycled in the liver & spleen G. Worn out RBC components are ___________ by macrophages: 1. Amino acids from ________ are used to make new proteins 2. Iron from heme is transported in blood by ___________ protein 3. Iron attaches to ________ protein & is stored in liver & muscles 4. ______ is picked up by RBC precursors in red bone marrow. 5. Heme is converted to ___________, which is secreted in _____ by the liver and kidneys; gives color to urine and feces. a. A high level of bilirubin in the blood causes _____________ (yellowish skin and sclera), which indicates liver disease or bile duct blockage b. Newborns sometimes exhibit jaundice due to increased _________ during the rapid conversion of fetal Hb to adult Hb V. _____________ (WBCs) compose about __% of the formed elements A. WBCs are ____________, do not contain hemoglobin, live from hours to years, and function in ____________ B. Normal blood contains about 5-10 ___________ WBCs/cc of blood C. WBCs are __________ according to their stained appearance 1. _________phils - have visible granules in their cytoplasm a. _____________ (60%) - have pale lilac granules, 3-5 lobed nucleus; are _____________, destroy bacteria with lysozyme & defensins. Sometimes called polymorphonuclear leukocytes (PMNs) due to variably shaped nuclei b. _________phils (1%) - stain dark blue, has S-shaped nucleus; similar to ______ cells that release ___________ (a vasodilator) and ___________ (an anticoagulant) in allergic & parasitic reactions, intensifies inflammatory response. c. ________phils (3%) - stain pink; 2 nuclear lobes; destroy ___________, and counteract effects of histamine 2. _________________ - have no visible cytoplasmic granules. a. ______________ (30%) - nucleus takes up most of cell; mediate immune responses in blood and lymphoid tissues. Types are: 1) ___ cells – responsible for __________ immunity: develop into memory cells and plasma cells that secrete __________ against foreign antigens (esp. bacterial) 2) ___ cells – responsible for _____-mediated immunity: attack fungi, transplanted cells, and cancer cells 3) Cytotoxic (_________) T cells destroy tumor cells & virus infected cells b. ___________ (6%) - largest WBC; nucleus is kidney-horseshoe shaped; migrate out of capillaries and become _____________ that phagocytize pathogens, then present their antigens for lymphocyte response (Remember quantities by: Never Let Monkeys Eat Bananas) 4 VI. __________ (thrombocytes) - megakaryocyte fragments that contain many granules but no nuclei. Functions: A. Initiate blood _________ B. Secrete ___________, which stimulates blood vessel constriction C. Life span is 5-9 ______ VII. ___________________ - Formation of Blood Cells A. Blood cells are first produced in the yolk sac of the _______, then in the bone marrow, liver, spleen, and thymus in the ________ B. From infancy onward, most formed elements are produced in the red bone ______; lymphocytes are also formed in lymphoid tissues C. Blood cells are formed from hemopoietic _______ cells (hemocytoblasts), which give rise to 5 different -blast cells (nucleated precursor cells): 1. Proerythroblasts - become mature _________cytes (RBCs). 2. Myeloblasts - become mature neutrophils, eosinophils, and basophils (__________ WBCs). 3. Monoblasts - become mature _____cytes (agranular WBCs), which become phagocytic _______phages. 4. Lymphoblasts - become mature ________cytes (agranular WBC B & T lymphocytes, cytotoxic killer cells). 5. Megakaryoblasts – fragment to become mature _________ (thrombocytes). D. Hematopoeitic _________ factors stimulate differentiation & proliferation of the different blood cells. 1. Erythropoietin (____) - hormone produced by _________ in response to hypoxia (low O2), increases pro__________blasts. 2. ___________ - small glycoproteins produced by bone marrow cells, lymphocytes, macrophages, and fibroblasts; include ________ Stimulating Factor & Inter________ that stimulate WBC formation. 3. Thrombopoeitin – a hormone produced by the _________ and stimulates formation of ___________. E. Red Bone ___________ (myeloid tissue) - produces RBCs, leukocytes, and platelets. F. Lymphoid tissue – also produce ______________ leukocytes. VIII. Blood Types A. The _____ Group includes blood types A, B, AB, and O, and is determined by the presence or absence of A and B __________ on RBCs (the antigens are glycoproteins and glycolipids) 1. Type A has the ___ antigen on the RBC 2. Type B has the ___ antigen on the RBC 3. Type AB has both ___ and ___ antigens 4. Type O has neither ___ nor ___ antigens 5 B. People must receive transfusions of similar blood type because they have ____________ (gamma globulins) against certain RBC antigens, which will cause ____________ (clumping of the blood) 1. Type A blood has antibodies (anti-__) against type B antigen 2. Type B blood has antibodies (anti-__) against type A antigen 3. Type AB blood does not have __ or __ antibodies 4. Type O has both ___ and ___ antibodies (anti-A & anti-B) 5. Knowing the above facts, which blood type would be the “universal donor” type? _______ Which would be the “universal recipient?” ______ C. ____ Group is determined by the presence or absence of Rh ___________ (D) on the RBC of different blood types 1. ____ has the D antigen and no anti-D antibodies 2. ____ does not have the D antigen, but can develop anti-D antibodies if exposed to ____ blood 3. If an ____ mother carries a second ____ fetus, her antibodies can cross the placenta and agglutinate the fetal blood, causing erythroblastosis _______. ________ is given to prevent this IX. Blood Disorders A. ______ disorders 1. ____________ - skin is pale due to a deficiency of RBCs or hemoglobin; causes include a. Inadequate erythropoiesis or hemoglobin synthesis, due to deficient _____, vit. _____, or intrinsic factor needed to absorb B12 b. Hemmorrhagic anemia due to blood ______ c. ____________ anemia due to excess destruction of RBCs 2. _____________ - excess RBCs in the blood; may be caused by cancer of bone marrow; treated by removing some blood 3. _________ cell disease - inherited condition in which abnormal hemoglobin crystalizes, causing RBCs to become __________ shaped and agglutinate; new treatments allow patients to survive B. ____________ - cancer of leukocyte forming cells in bone marrow causes high WBC count, cancer cells crowd out normal ____ cells in marrow; leukemia patients suffer from anemia, infections, & internal hemorrhaging; treatment includes bone _______ transplant C. Thrombocytopenia - low number of __________ in blood; results in diminished ______ formation & increased internal bleeding D. Blood cell ________ are used to determine the percentage of formed elements in the blood and disease 1. Hematocrit (___) is measurement of RBC% in whole blood; 37-52% is normal; less = _______, greater = ____________ 2. A ___________ WBC Count counts the number of each WBC type to diagnose disease 6 a. 3. _______phils - normal is 50-60%; higher indicates _______ infection, burns, stress, or inflammation. b. _______phils - normal is 1-4%; higher indicates allergic reactions, ___________ infections, autoimmune disease, or adrenal insufficiency. c. _______phils – normal is <1%; higher indicates _________ reactions, leukemia, cancers, or hypothyroidism. d. __________cytes – normal is 20-30%; higher indicates viral infection, immune disease, or ____________. e. _______cytes – normal is 2-8%; higher indicates ________ (e.g.: Epstein-Barr virus) or fungal infection, tuberculosis, leukemia or some chronic disease. f. Bone _________ Transplant is used to treat several types of anemia, leukemia, and other blood disorders. Complete Blood Count (____) used to determine RBC count, hemoglobin, hematocrit, WBC count, differential WBC count, and platelet count. X. Platelets and Coagulation A. _________ are small fragments of megakaryocytes that contribute to __________ (the cessation of bleeding). Their functions include 1. Secretion of procoagulants (_________ factors) and vaso___________ 2. Formation of platelet _______ to stop bleeding 3. Dissolution of old blood _______ 4. ________________ of bacteria 5. Chemical secretion to attract neutrophils and ____________ to areas of inflammation 6. Growth factor secretion to stimulate mitosis in _____blasts and smooth _________ to maintain linings of blood vessels B. Platelets play a role in all 3 ___________ mechanisms – vascular spasm, platelet plug formation, and blood clotting (coagulation) 1. Vascular spasm – ___________ released by platelets constricts smooth muscle of broken blood vessels, which reduces bleeding 2. Platelet _______ formation – platelets adhere to exposed __________ fibers in the torn blood vessel wall, which temporarily seals the break 3. ____________ and blood vessel repair occurs as a mass of sticky _________ proteins forms via a cascade of protein factors (I-XII) and other enzymes produced mainly in the _______, as well as platelet factors (PF1-4) produced by __________ a. ______________ mechanisms begin outside the blood stream. Damaged blood vessel cells release tissue thrombo________ (factor III), which leads to activation of factor ___ (a procoagulant) b. ____________ mechanisms employ factors in the blood plasma and platelets; exposed collagen activates factor ____ (Hageman factor), which also leads to activation of factor __. _________ is required in both pathways. c. Activation of factor X leads to the formation of ___________, from prothrombin. d. Thrombin cuts plasma fibrinogen into __________, which polymerizes to form the clot 7 e. Platelet-derived _______ factor (PDGF) stimulates fibroblasts and smooth muscle cells to _______ damaged blood vessel and surrounding connective tissues f. Tissue repair is followed by fibrinolysis, in which the blood clot is dissolved by ________, an enzyme created from plasminogen by thrombin and tissue plasminogen activator (____) 1) t-PA is used clinically to dissolve blood _____ formed during strokes and heart attacks C. Inappropriate _____________ is prevented by 1. Platelet repulsion by ____________ on blood vessel endothelium 2. Dilution of small amounts of _________ that form spontaneously 3. Anticoagulants, such as _________ secreted by basophils and mast cells D. Coagulation disorders 1. ____________ – inherited inability of blood to clot due to lack of factor VIII (hemophilia __), factor IX (hemophilia __), or factor XII (hemophilia __). Suffers are treated with _________ factors 2. __________ – abnormal clotting of blood in an unbroken vessel. a. A ____________ (clot) may block a blood vessel, or break off and travel through the blood stream as an b. ______________, which can block blood flow to a vital organ (e.g., pulmonary embolism)