Developing Regulations to Protect Older Adults
advertisement

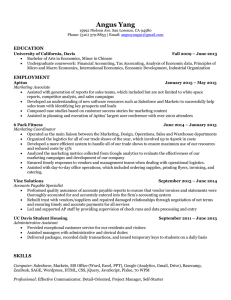
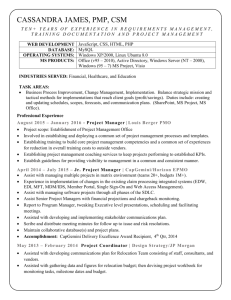
Developing Regulations to Protect Older Adults Office of Health Care Quality Student: Grace E. Mandel Preceptor: Amanda Thomas, MPH Health Policy Analyst for Regulatory Affairs Office of Health Care Quality Monitors the quality of care in Maryland’s health care facilities and community-based programs through regulation, surveying and education dhmh.maryland.gov/ohcq Regulatory Process Formal Informal Submit to Office of Policy and Regulations Develop Draft Approval Process New Regulation 1 • • • • Why revise a regulation? Adopt new requirements Amend requirement Repeal requirements Remove outdated information OR 1 Why revise a regulation? • • Respond to request from Governor Comply with: – – Regulation Review and Evaluation Act (RREA) New legislation 2 Paperwork to Office of Policy and Regulations (OPR) All Updates Require: • Notice of Regulation Development Form • Background Form • Proposed Action Form & If Mandatory under RREA: • Work Plan • Evaluation Form & If Incorporation by Reference: • Incorporation By Reference Form 3 Who Participates in Draft Development? Stakeholders & Community Members -Town Hall Meetings -One on One Meetings -Informal Comments & Program Coordinators and Managers -Incorporate feedback to develop a new draft Submit to Approval Process Approval Process 4 5 6 • Formal Comment Period • Administrative, Executive, and Legislative Review Committee (AELR) Reviews Proposed Updates • Governor Signs Regulation Assisted Living • Defining Characteristics – Autonomy, choice, and dignity – Less expensive than long term care – Designed for adults with limited needs assistance Stakeholder Involvement • Forums • One on One Meetings • Comment Periods • Goal: Education & improvement of the regulation Attendance at Forums Satisfaction at Forums Informal Comments Stakeholders OHCQ Surveyor* 11% Other 3% Providers 39% State or Local Government 19% Training Provider or Educator 13% Advocacy Organization/ Professional Association 15% Interest Areas 7% 3% 22% 9% Clinical Care and Services Training 5% Licensing Resident Protections & Rights 6% 14% Staffing Medication 10% Facility Standards Definitions 12% 12% Editing Other Manager Training (1) The assisted living manager shall at a minimum: (i) A 4-year, college-level degree; (ii) 2 years experience in a health care related field and 1 year of experience as an assisted living program manager or alternate assisted living manager; or (iii) 2 years experience in a health care related field and successful completion of the 80-hour assisted living manager training program; Manager Training Comments on Managers Requirement “I am unclear how a college degree will impact one's ability to effectively manage an assisted living facility. What seems more relative and appropriate is experience in the field as well as taking the 80 hour Manager's training Course through the Beacon Institute.” Staffing Ratio • “Clarify what “on site staff sufficient in number means”. This is impossible to prove.” • “Appropriate staffing is determined by the organization providing the services. This determination is made by careful evaluation of the resident's needs, type of staffing provided and possibility of requiring private duty care givers in situations where appropriate. Too many details go into making this determination and cannot be successfully determined by OHCQ by making a blanket statement for all facilities.” Public Health Impact • Protections for residents of Assisted Living facilities • Flexibility while also having enforceable standards • Easily Interpretable Regulations Special Thanks! • Amanda Thomas, MPH – Health Policy Analyst for Regulatory Affairs • Dr. John Parrish – Director of Quality Initiatives Unit • Dr. Beth Resnick and Paulani Mui, MPH – Johns Hopkins Bloomberg School of Public Health