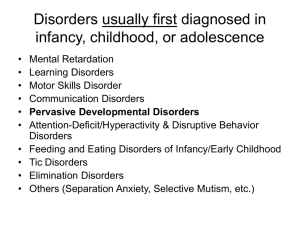
Psikologi Anak Pertemuan 11 Developmental disorders and Learning disorders

Psikologi Anak
Pertemuan 11
Developmental disorders and
Learning disorders
Mental Retardation
DSM-IV Diagnostic criteria
“The essential feature of Mental Retardation is significantly subaverage general intellectual functioning (criterion A) that is accompanied by significant limitation in at least two of the following skill areas: communication , self-care, home living, social/interpersonal skills, work, leisure, health and safety (criterion B). The onset must occur beforeage 18 years (criterion C).”
American Association on Mental Retardation (AAMR)criteria
• level of environmental support required by the individual
(intermittent, limited, extensive or pervasive)
• 4 different areas: intellectual functioning & adaptive skills, psychological/emotional functioning, physical/health, and environment
Continuum of Severity of MR
(from the DSM-IV)
• Mild mental retardation= IQ level 50-55 to 70
• Moderate retardation= IQ level 35-40 to 50-55
• Severe mental retardation= IQ level 20-25 to 35-40
• Profound mental retardation= IQ level < 20-25
• Also severity unspecified if individual is untestable
Characteristics of children with MR
• Children with mental retardation a heterogeneous and variable group
– some children with MR are placid, passive and dependent whereas others may be aggressive and impulsive.
• however, it is common for people with MR to show deficits in social skills
• lack of well developed communication skills may predispose children with MR to disruptive and aggressive behaviours
• no specific physical features associated with MR.
• children with MR are at increased risk of being exploited by others
(e.g., physical &/or sexual abuse)
• the incidence of mental disorders in individuals with MR is 3-4 times greater than it is in the general population.
• common comorbidities: ADHD, mood disorders, pervasive developmental disorders, stereotypic movement disorder.
Course of MR
• age & mode of onset depend on the aetiology and severity of the MR
– more severe retardation (esp. when associated with a specific syndrome e.g., Down’s syndrome) tends tobe identified early
• where the retardation results from an acquired cause, onset can be very abrupt
• MR not necessarily a life long disorder (mild
MR)
Aetiology of MR
General points
• Many risk factors for MR have been identified
• For 30-40% of MR cases aetiology is unclear in the past MR has been seen as being caused by either biological factors or psychosocial factors
• recent theories view MR as being the result of a combination of factors, although one factor may contribute more than others.
Genetic Risk Factors for MR
• Chromosomal abnormalities implicated in 10-20% of cases of MR in which there is a known cause
– Down’s Syndrome
– Fragile X Syndrome
• Genetic disorders
– PKU
Aetiology of MR
Prenatal Risk Factors for MR
• FAS & FAE
• Malnutrition
• Uncontrolled maternal diabetes
• viral & bacterial infections: HIV,
Toxoplasmosis which results in MR in 85% of offspring affected,
Rubella
Perinatal Risk Factors for MR
• Oxygen deprivation during delivery
• Prematurity
• LBW
Postnatal Risk Factors for MR
• extreme deprivation
• Disease: encephalitis, meningitis
• Lead poisoning
• other mental disorders (eg.
Autism, ADHD)
Psychosocial risk factors for MR
• Maternal age: teenage mothers and mothers over 35
• Low SES
• Sex
Placement and treatment options
Institutionalisation
• Approx. 4% of children with MR are institutionalized today
• Factors affecting decision to institutionalise: day to day stress, child’s level of functioning & potential for future learning, child’s behaviour, family attitude towards placement, medical or physical problems experienced by MR child, availability of respite care, professional advice, placement and treatment options
Therapy
• single most important psychological therapy used with MR children
& their families is behaviour therapy or behaviour modification
– aims to eliminate maladaptive behaviours (aggression,selfstimulation) & enhance adaptive skills (language, self-care etc)
Pervasive developmental disorders
• Pervasive developmental disorders such as
Autistic Disorder and Asperger’s Disorder are characterized by severe and pervasive impairments in several areas of development
– Reciprocal social interaction skills
– Communication skills
– Stereotyped behaviours, interests or activities
Reciprocal Social Interaction: Autism
• Nonuse or limited use of nonverbals
• Gesture, eye contact, nodding agreement
• Failure to develop peer relationships
• Lack of spontaneous seeking to share enjoyment or interests
• Lack of social or emotional reciprocity, give and take, showing interest
• Impaired awareness of others
Stereotyped Behaviour: Autism
• Preoccupation with one or more restricted patterns of interest
• Inflexible adherence to nonfunctional routines or rituals
• Stereotyped motor mannerisms
• Preoccupation with parts of objects
• Abnormal posture or gait
• Fascination with movement
• Attachment to an inanimate object
Communication: Autism
• Delay or lack of development of language
• Impaired ability to initiate or sustain a conversation
• Stereotyped or repetitive use of language
- Echolalia
- Idiosyncratic language
• Lack of spontaneous make believe play or social imitative play
• When speech does develop – abnormal pitch, intonation, rate, rhythm or stres, impairment in comprehension of language
Asperger’s Disorder
Social Behavior
• Not motivated to play with others – selffocused
• Tendency to dominate if engaged with others
• At lunch time tend to be alone - often in library or an isolated part of the playground
• No interest in team activities
• Often excluded by other children and often the victim of bullies
• Codes of conduct not understood
Language
• These children can be delayed in language but most talk fluently by age 5.
• Pragmatic difficulties (repairing a conversation,coping with uncertainty, irrelevant comments, interrupting)
• Semantic difficulties (literal interpretations)
• Problems with prosody (lack of variation, accent, formal language, pedantic, idiosyncratic words, vocalizing thoughts)
Asperger’s Disorder
Interests and routines, Motor Clumsiness, Cognition
• May begin with collecting objects
• Interest in a special topic
• Romantic interest in a real person
• Need for routine, sameness
• Limited ability to kick and catch ball, tie
• shoelaces, odd gait, poor handwriting
• Theory of mind - difficulty in conceptualizing the fact that others have thoughts and feelings
• Mind-reading
Course of Disorder
Autism
• Onset prior to age 3
• Developmental gains during school age
• Some deteriorate at adolescence others improve
• language skills and IQ best predictors of prognosis
• Small percentage live and workindependently
Asperger’s
• Often not diagnosed until school age
• Heterogeneous presentation
• Many go on to succeed in work and to live independently- best predictors are ability to learn social skills, support etc
• Prognosis may be better than for Autism
• Different presentation in females
Aetiology
Genetic predisposition
• Concordance rates in identical twins ~50%
• Runs in families (siblings of children with ASD 50x more likely to be diagnosed than baseline)
• Sex-linked?
• Unfavourable obstetric events
– Some mums report difficult or complicated births in children later diagnosed ASD
Neuropsychological Abnormalities
• Cerebellar abnormalities (reduction in size)
• Left hemisphere abnormalities (unusual MRIs)
• High comorbidity with seizures
• Autopsy studies show heavy brains
• Rate of growth of brain (Courchesne)
Diet
• Some suggestion that diet can affect symptoms
• Food additives, wheat (gluten), milk (lactose)
MMR (measles, mumps, rubella)
• Latest study (British Medical Journal, 2001) found no evidence of vaccineautism link suggestion that MMR vaccine could exacerbate already present autism symptoms
Treatment approaches
• Applied Behaviour Analysis (ABA)
• Increase communication (PECS)
• Relationship Development Intervention
• Floortime
• Sensory Integration
• Social Skills Training
• Pharmacotherapy and diet
• TEACCH
Learning Disorders
LD diagnosed when achievement on individually administered, standardized tests in reading, mathematics or written expression is substantially below that expected for age, schooling and level of intelligence
(discrepancy method)
• significant interference caused
Learning Disorders: Subtypes
• Reading Disorder – Dyslexia
• Mathematics Disorder – Dyscalculia
• Disorder of Written Expression - Dysgraphia
• Learning Disorder Not Otherwise Specified
Characteristic features of children with LDs
• LD child differs from normal learner by characteristics of the LD, rather than by its presence
• IQ score usually in average or above average range but performance on tests very variable
• at increased risk for psychological problems
• poor self-esteem; high rate of high school drop out
Non-Verbal Learning Disorder
• Not in DSM-IV
• Characteristics
– Motor coordination difficulties
– General lack of coordination
– Both gross and fine motor problems (pencil grip)
– Balance problems
– Academic difficulties
– Deficits in maths, writing and reading comprehension
– Problems with organisation, reasoning and problem-solving (executive functioning)
– Strong verbal and attentional memory
– Good spelling and reading (errors are phonemically correct)
Non-Verbal Learning Disorder
Characteristics
• Visuo-spatial deficits
– Poor visual organisation and recall (Rey)
– Faulty spatial perception and spatial relations
• Emotional
– Tantrums (difficult to soothe)
– Easily overwhelmed (esp. by change in routine)
– Vulnerable to depression, anxiety and low self esteem
• Social difficulties
– Lack of ability to comprehend non-verbal communication
– Deficits in social judgement and social interaction
• Problems with peer relationships