Atopic Dermatitis
advertisement

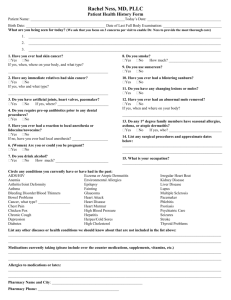
Atopic Dermatitis April 2015 Pediatric Continuity Clinic Curriculum Created by: Matthew Pertzborn, PGL-2 Objectives Describe the common clinical presentation and diagnosis of atopic dermatitis Understand the management of atopic dermatitis Discuss common co-morbidities and complications of atopic dermatitis Case #1 A 12 month old female presents with a 6 month history of intermittent erythema, dryness, and cracking of the skin on the face and on the extensor surfaces of the arms. She has been scratching at the affected areas. Question 1-1: What is the differential diagnosis of these symptoms? Question 1-2: What is the typical distribution of atopic dermatitis? Question 1-3: What are common triggers of atopic dermatitis? Discussion question 1-1? Differential includes: Contact dermatitis Psoriasis Impetigo Histiocytosis X (particularly if the distribution involves the diaper area in children wearing diapers) Wiskott-Aldrich syndrome Scabies Seborrheic dermatitis Drug reaction Lymphoma with cutaneous involvement Immune system disorder (e.g. hyper-IgE syndrome) Zinc deficiency Discussion question 1-2? It is important to be aware of the typical distribution: Infants (most common onset is between 3 and 6 months of age) Older Children Face Extensor sites Trunk Flexor sites Antecubital fossa Popliteal fossa Neck Trunk Typically spares the groin and axillary areas Stuffy-sounding nose is a common observation Discussion question 1-3? Common triggers/exacerbating factors in atopic dermatitis: Food/formula Mechanical Soaps Detergents Wool Weather (e.g. low levels of humidity) Diaphoresis Dust mites (Dermatophagoides pteronyssinus) Mold Pollen Pets Bacteria Stress Additional Information Image From: Pediatrics In Review (Reference #1) Additional Information Often follows a relapsing course The term “atopic dermatitis” and “atopic eczema” (often simply called “eczema”) are the same Itching is very characteristic IgE often elevated Case #2 A 3 year old male presents with a 2 year history of intermittent erythema, dryness, and cracking of the skin on the face and on the extensor surfaces of the arms. The symptoms were previously controlled adequately with application of Vaseline after baths. He has been having multiple flares of these symptoms despite the Vaseline management and the mother is wondering what else can be done. Question 2-1: What is the first-line management for eczema in general? 2-2: What is the best next treatment choice for the patient above? 2-3: Is there a non-corticosteroid alternative for severe disease? Discussion question 2-1? Initial Management of Eczema: Removal of potential triggers if possible Use mild, non-scented soap (e.g. Dove soap) only Minimize non-soap cleaners Should be neutral to low pH, fragrance-free, hypoallergenic if used Removal of certain detergents for washing clothes. Avoid dryer sheets (e.g. Bounce) and detergents with fragrances. Topical moisturizers/emollients (e.g. petrolatum jelly, Aquaphor ointment) Ointments more effective than creams Lotions should be avoided Application after bath (immediately after drying) Application throughout the day Exact frequency and amount not well delineated in the literature Discussion question 2-2? Management of acute flares if the initial management is not adequate: Some advocate burst of high-dose corticosteroids with tapering in potency once controlled, others advocate starting with lowestpotency corticosteroids and then titrating upward Potency ranges from lowest-potency (class VII (e.g. hydrocortisone 0.25-1%)) to high-potency corticosteroids (class I (e.g. diflorasone)) Caution should be used when applying higher-potency corticosteroids to the face, neck, or skin-folds as risk of significant systemic absorption is higher in these areas Avoid using higher-potency corticosteroids for more than 2 weeks at a time Typically dosed 2x per day Discussion question 2-2? Management of acute flares if the initial managements are not adequate: Wet-wrap therapy can be useful as adjunct Involves covering the area on which the topical moisturizer or topical corticosteroid is applied with a wet bandage and then placing a dry bandage on top of the wet bandage Wrap may be kept on for up to 24 hours at a time and this adjunct has been used for as much as 2 weeks in the literature Use of this adjunct with mid- to high-potency corticosteroids is controversial Discussion question 2-3? Topical calcineurin inhibitors May be used to avoid side/adverse effects of corticosteroids, particularly if high-potency corticosteroids are required, skin atrophy secondary to corticosteroid use occurs, or topical corticosteroids are required long-term Topical tacrolimus ointment (0.03-0.1%) or pimecrolimus cream (1%) Typically dosed 2x per day Additional Information Clinical pearl: Important to apply emollient/ointment after every bath (pad down with towel, don’t wipe after the bath prior to application) Case #3 A 3 year old male presents with a 2 year history of intermittent erythema, dryness, and cracking of the skin on the face and on the extensor surfaces of the arms. Starting 5 days ago, there has been some crusting on the face with a small amount of yellow oozing What other medical conditions (non-infectious) are associated with eczema? Are there increased risk of infectious co-morbidities in eczema? Is there anything that can be done to prevent secondary infection? Discussion question 3-1? Allergic rhinitis, asthma, and food allergies are associated with eczema. Extra careful screening for the above conditions should occur Discussion question 3-2? Secondary skin infections possible: Appropriate systemic antibiotic therapy if secondary infection occurs (depends on local resistance profiles) Staphylococcus aureus most common Clindamycin Bactrim If secondary infections frequent: Mupirocin to the nares if Staphylococcus aureus colonization suspected (BID x10 days) Bleach baths if signs of secondary infection present (may also do this prophylactically if eczema is extensive) Can reduce colonization dramatically 1/4-1/2 cup household bleach (6% sodium hypochlorite) in half-filled bath Stay in bath 20 minutes then rinse with fresh water after Typically weekly Lukewarm temperature Additional Information Clinical pearl: Remember to ask about family history of allergic rhinitis (seasonal allergies), hay fever, asthma, and eczema. 70% of patients with eczema have atopic disease in other members of the family PREP Question PREP 2014 Item 141: The mother of a 7-month-old infant is frustrated that the infant’s atopic dermatitis is not getting better. He is awake “all night” scratching and is irritable and fussy. She has been giving him diphenhydramine every 8 hours and applying hypoallergenic moisturizer and a topical corticosteroid cream twice a day. The infant was breastfed until 3 months ago and then switched to a cow milk-based formula. On physical examination, you notice that he has dry, erythematous papules and patches, with excoriation marks on his face, neck, antecubital fossae, popliteal fossae, and back. He has normal growth parameters. Of the following, the MOST appropriate next step in this infant’s management is to recommend: A. discontinuing diphenhydramine and switching him to daily loratadine B. eliminating cow milk, egg, soy, and wheat from his diet C. Introducing cow milk on a trial basis to see if the rash worsens D. switching to hypoallergenic formula and a diet of only rice and chicken E. testing for pertinent, potential food allergen triggers PREP Question PREP 2014 Item 141: The mother of a 7-month-old infant is frustrated that the infant’s atopic dermatitis is not getting better. He is awake “all night” scratching and is irritable and fussy. She has been giving him diphenhydramine every 8 hours and applying hypoallergenic moisturizer and a topical corticosteroid cream twice a day. The infant was breastfed until 3 months ago and then switched to a cow milk-based formula. On physical examination, you notice that he has dry, erythematous papules and patches, with excoriation marks on his face, neck, antecubital fossae, popliteal fossae, and back. He has normal growth parameters. Of the following, the MOST appropriate next step in this infant’s management is to recommend: A. discontinuing diphenhydramine and switching him to daily loratadine B. eliminating cow milk, egg, soy, and wheat from his diet C. Introducing cow milk on a trial basis to see if the rash worsens D. switching to hypoallergenic formula and a diet of only rice and chicken E. testing for pertinent, potential food allergen triggers (see PREP 2014 for explanation) PREP Question PREP 2014 Item 106: The parents of a 3 year old boy would like him to be tested for allergies. The parents report that the boy has had worsening symptoms of itchy eyes, sneezing fits, and nasal congestion since the family got a new dog 1 year ago. The parents would like the boy tested to determine if they need to give the dog away. They are reluctant to stop the boy’s daily antihistamine and are disappointed to learn that skin testing cannot be performed while taking this medication.You decide to obtain bloodspecific IgE testing. However, the parents have read on the internet that the “scratch test” is a better test. Of the following, you are MOST likely to advise the parents that in this situation, blood-specific IgE testing is: A. Comparable to skin testing B. Less expensive and better tolerated by children than skin testing C. More accurate than skin testing D. The only testing that can be done because he is too young for skin testing E. A preliminary test and you will obtain skin testing to confirm the results PREP Question PREP 2014 Item 106: The parents of a 3 year old boy would like him to be tested for allergies. The parents report that the boy has had worsening symptoms of itchy eyes, sneezing fits, and nasal congestion since the family got a new dog 1 year ago. The parents would like the boy tested to determine if they need to give the dog away. They are reluctant to stop the boy’s daily antihistamine and are disappointed to learn that skin testing cannot be performed while taking this medication. You decide to obtain blood-specific IgE testing. However, the parents have read on the internet that the “scratch test” is a better test. Of the following, you are MOST likely to advise the parents that in this situation, blood-specific IgE testing is: A. Comparable to skin testing (see PREP 2014 for explanation) B. Less expensive and better tolerated by children than skin testing C. More accurate than skin testing D. The only testing that can be done because he is too young for skin testing E. A preliminary test and you will obtain skin testing to confirm the results References and Future Reading Eichenfield, Lawrence F., Wynnis L. Tom, Sarah L. Chamlin, Steven R. Feldman, Jon M. Hanifin, Eric L. Simpson, Timothy G. Berger, James N. Bergman, David E. Cohen, Kevin D. Cooper, Kelly M. Cordoro, Dawn M. Davis, Alfons Krol, David J. Margolis, Amy S. Paller, Kathryn Schwarzenberger, Robert A. Silverman, Hywel C. Williams, Craig A. Elmets, Julie Block, Christopher G. Harrod, Wendy Smith Begolka, and Robert Sidbury. "Guidelines of Care for the Management Of atopic dermatitis." Journal of the American Academy of Dermatology 70.2 (2014): 338-51. Web. Cipriani, Francesca, Arianna Dondi, and Giampaolo Ricci. "Recent Advances in Epidemiology and Prevention of Atopic Eczema." Pediatric Allergy and Immunology. 10 Dec. 2014. Web. 28 Dec. 2014. References and Future Reading Knoell, K. A., and K. E. Greer. "Atopic Dermatitis." Pediatrics in Review 20.2 (1999): 46-52. Web. Krakowski, A. C., L. F. Eichenfield, and M. A. Dohil. "Management of Atopic Dermatitis in the Pediatric Population." Pediatrics 122.4 (2008): 812-24. Web.