Changing Practitioner Behavior
advertisement
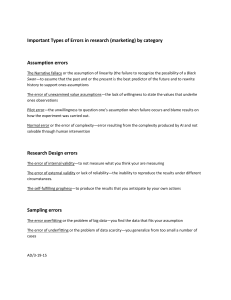
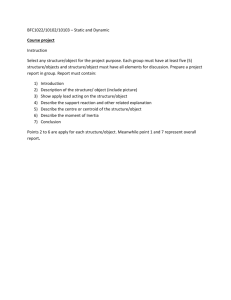
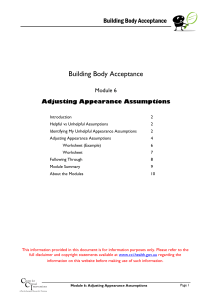
Changing Practitioner Behavior Gail D’Onofrio MD, MS Professor and Chief Section of Emergency Medicine Yale University School of Medicine Principles of Motivational Interventions Create cognitive dissonance Lessen ambivalence by reflection on conflicting motivations Negotiate strategies for change Steps: Brief Intervention Raise the subject Provide Feedback Enhance Motivation Negotiate & Advise NIDA: Principles of Drug Addiction Treatment #10 Treatment does not need to be voluntary to be effective Strong motivation can facilitate the treatment process. Sanctions or enticements in the family, employment setting, or criminal justice system can increase treatment entry, retention rates and success of interventions Approaches to Quality Improvement and Their Assumptions on Improving Medical Care Grol, R. Improving the quality of medical care: Building bridges among professional pride, payer profit and patient satisfaction JAMA. 2001:28:2578-86 Approach Evidence-based Medicine Clinical guidelines Decision Aids Assumption Provision of best evidence and convincing information leads to optimal decision making and optimal care Approach Professional education and development Self-regulation Recertification Assumption Bottom up learning based on experiences in practice and individual learning needs leads to performance change Approach Assessment and accountability Feedback Accreditation Public reporting Assumption Providing feedback on performance relative to peers, and public reporting of performance data, motivate change in practice routines Approach Patient-centered care Patient involvement Shared decision making Assumption Patient autonomy and control over disease and care processes lead to better care and outcomes Approach Total quality improvement Restructuring processes Quality systems Assumption Improving care comes from changing the system, not from changes in individuals Effects of Different Strategies to Improve Patient Care Strategy Educational Materials Continuing education Interactive education meetings Educational outreach visits Use of opinion leaders Feedback on performance Conclusions Limited Limited Few studies, mostly effective Affects prescribing and prevention Mixed effects Mixed effects, effect on test ordering Strategy Reminders Substitution or delegation of tasks Use of computer Total quality management and CQI Patient-oriented interventions Combined and multifaceted interventions Conclusions Mostly effective Pharmacist: effect on prescribing; Nurse: No Mostly effective Limited effects, weak study design Mixed effects, reminding pts good for prevention Very effective Clinical Inertia “Recognition of the problem, but failure to act.” Phillips LS, et al. Clinical inertia. Ann Intern Med. 2001;135:825-834 Clinical Inertia Problem of the provider and system It is not related to patient adherence to treatment regimens Result of: – – – Overestimation of care Use of “soft” reasons to avoid changes Lack of training and practice structure needed to attain goals Strategies to approach practitioner behavioral change Provide skills-based educational sessions Elicit opinion leaders Institute systems changes (forced computer entry, reminders, multiple screeners etc.) Provide ongoing feedback to practitioners Provide incentives (positive or negative) Be creative