26 Role of Functional Magnetic Neuroimaging in Diagnosis and Research
advertisement

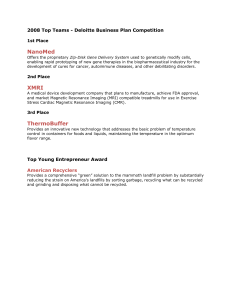
Functional MRI Techniques in Atypical Parkinsonism 451 26 Role of Functional Magnetic Neuroimaging in Diagnosis and Research Hartwig Roman Siebner and Günther Deuschl INTRODUCTION Recent advances in magnetic resonance imaging (MRI) have opened up new possibilities to map distinct aspects of human brain function in vivo. Functional magnetic resonance imaging (fMRI) is widely used to assess changes in regional neuronal activity at high spatial and temporal resolution (1,2). Magnetic resonance spectroscopy (MRS) provides a means to probe distinct aspects of brain metabolism at a regional level (3,4). Water diffusion magnetic resonance imaging (dMRI) can be used to study the integrity of white matter tracks in the brain (5). MRI has already been successfully applied to study the pathophysiology of movement disorders such as Parkinson’s disease (PD) (6,7). The aim of this chapter is to summarize how these innovative MRI methods may be useful for diagnosis and research of atypical parkinsonian disorders. FUNCTIONAL MAGNETIC RESONANCE IMAGING Neuroimaging techniques, such as single photon emission tomography (SPECT), positron emission tomography (PET), and fMRI, provide a means of mapping regional neuronal activity in vivo in the intact human brain. Blood oxygen level-dependent (BOLD) fMRI uses echo-planar imaging (EPI) to detect changes in the oxygenation state of the blood (8). Recent studies of the monkey brain combined BOLD-sensitive fMRI with electrophysiological measurements to demonstrate that the BOLD signal primarily measures the input and processing of neuronal information within a brain region (2). Since the BOLD signal is an intrinsic signal, BOLD-sensitive fMRI does not require the injection of a contrast agent. Compared to PET and SPECT, BOLD-sensitive fMRI does not involve exposure to radiation, is widely available, and offers a higher spatial and temporal resolution. Moreover, eventrelated fMRI protocols allow studies to investigate changes in the BOLD signal related to a single movement, whereas SPECT and PET can only map the averaged regional cerebral blood flow (rCBF) changes caused by multiple trials. Because of these methodological advantages, BOLD-sensitive fMRI has largely replaced PET and SPECT of rCBF as a tool to study the functional architecture of the human brain. In recent years, BOLD-sensitive fMRI has been extensively used as a research tool to study the functional consequences of nigrostriatal dopamine loss in idiopathic PD. So far, most studies have investigated changes in BOLD signal related to volitional hand movements (9–12). These studies have disclosed a movement-related dysfunction in basal ganglia-thalamocortical loops that are From: Current Clinical Neurology: Atypical Parkinsonian Disorders Edited by: I. Litvan © Humana Press Inc., Totowa, NJ 451 452 Siebner and Deuschl involved in manual motor control. However, the pattern of abnormal movement-related activity in frontal motor areas has been variable across studies (9–12). Since these studies used motor tasks that differed in terms of movement parameters and cognitive load, the implication is that, in PD, functional impairment of the various basal ganglia-thalamocortical motor loops is highly dependent on the motor context. In addition to motor activation studies, BOLD-sensitive fMRI has also successfully been employed to assess nonmotor functions such as attention to action and working memory in PD (12,13). Repeated fMRI measurements have also been used to image the acute effects of a therapeutic intervention. For instance, pharmacological fMRI studies have consistently demonstrated a partial normalization of movement-related activation in frontal motor areas after oral administration of levodopa (9–11). At present, there are no fMRI studies investigating atypical parkinsonian disorders. However, the experience with fMRI gathered in PD indicates that fMRI can successfully be applied in atypical parkinsonian disorders. The main potential of fMRI lies in its ability to assess the functional consequences of the underlying neurodegenerative process. Activation studies with fMRI can not only reveal regional abnormalities in task-related activity but also disclose abnomal functional integration among brain regions that form a functional network (12). The pathology of atypical parkinsonian disorders affects brain regions that are not subject to neurodegeneration in PD (14). Therefore, fMRI studies may be particularly revealing if the behavioral paradigm activates a functional system that is specifically affected by the suspected atypical parkinsonian syndrome. For instance, in patients with progressive supranuclear palsy (PSP), fMRI studies that explore distinct aspects of voluntary control of eye movements such as smooth pursuit and saccade generation may reveal specific functional abnormalities in regions involved in ocular motor control. Therefore, fMRI may provide a better understanding of the pathophysiology and help to establish a specific profile of abnormal brain activation for the various atypical parkinsonian disorders. In contrast to PET activation studies, fMRI activation studies allow to acquire many hundreds of brain volumes during a single session. Therefore, single-subject fMRI provides sufficient statistical power to analyze individual activation patterns. This is of relevance in atypical parkinsonian disorders since it may be difficult to recruit a sufficient number of well-characterized patients to ensure sufficient statistical power for between-group comparisons. Pharmacological fMRI provides a means to objectively measure the functional effects of therapeutic agents on neuronal activity. Serial fMRI measurements of the functional response to levodopa can be used to address the question why a subgroup of patients with multiple system atrophy (MSA) shows a sustained levodopa response during the course of the disease. In conjunction with structural MRI, long-term fMRI studies might be of value to monitor disease progression in patients with atypical parkinsonian disorders. MAGNETIC RESONANCE SPECTROSCOPY MRS provides chemical information on tissue metabolites (3,4). The molecules that can be studied by MRS in human brain tissue are hydrogen 1 (1H) and phosphorus 31 (31P). Magnetic resonance sensitivity is far greater for protons than it is for phosphorus (3). Therefore, most commercial MR scanners are capable of only proton MRS. Spectra are usually obtained from localized brain regions. The brain region is defined on a single slice by placing a small voxel, on the order of 1 or 2 cm2, in the area of interest. The compounds that can be observed in proton spectra are primarily identified by their frequency (i.e., their position in the spectrum), expressed as the shift in frequency in pars per million (ppm) relative to a standard. A normal spectrum shows peaks from N-acetyl groups, especially N-acetylaspartate (NAA) at 2.0 ppm, creatine (Cr), and phosphocreatine at 3.0 ppm, and choline-containing phospholipids (Ch) at 3.2 ppm (3). An additional peak at 1.3 ppm arises from the methyl resonance of lactate and is normally barely visible above the baseline noise (3). Pathologic conditions that involve regional neuronal loss lead to region-specific decreases in the relative NAA Functional MRI Techniques in Atypical Parkinsonism 453 concentrations (3,4). Since NAA is a marker of neuronal integrity, proton MRS provides a noninvasive means of quantifying neuronal loss or damage in vivo. Ch and other lipids are markers of altered neuronal membrane synthesis. Cr is a possible marker of defective energy metabolism. Typically, individual metabolic ratios obtained from peak areas of the spectrum are used as input to the statistical analysis. Because total Cr concentration is relatively resistant to change, Cr is often used as an internal standard to which the concentrations of other metabolites are normalized. Proton MRS has been used by several groups to study brain metabolism in nondemented PD yielding conflicting results (15–27). In general, the majority of these studies have failed to detect consistent abnormalities for NAA, Ch, or Cr in the basal ganglia (15–19,21,24,25; but see refs. 20,26,27) or the cerebral cortex (19,21,25; but see refs. 22,23). A multicenter study that included 151 patients with PD and 97 age-matched controls found no overall differences in the striatal proton spectra between groups (16). However, there was a decrease in the NAA/Cho ratio in a subgroup of elderly patients (aged 51–70 yr) and patients that were not treated with levodopa (16). These findings suggest that proton MRS may reveal subtle metabolic abnormalities in patients with PD depending on age and medication. Therefore, heterogeneities of clinical features across patient groups may at least in part account for discrepancies across studies (15–27). Three out of four proton MRS studies have reported abnormal proton spectra in patients with atypical parkinsonian disorders (15,18,19; but see ref. 26). Davie et al. (15) performed proton MRS of the lentiform nucleus in seven patients with MSA-P (predominantly striatonigral variant) and five patients with MSA-C (olivocerebellar variant). Compared with healthy controls, the NAA/Cr ratio was significantly decreased in patients with MSA (15). Tedeschi et al. (19) found a reduced NAA/Cre ratio in the brainstem, centrum semiovale, and frontal and precentral cortex, and a reduced NAA/Ch ratio in the lentiform nucleus in 12 patients with PSP compared with healthy controls (Fig. 1). The same study also included nine patients with corticobasal degeneration (CBD). CBD patients also showed an abnormal metabolic pattern with a reduced NAA/Cre ratio in the centrum semiovale and a reduced NAA/Ch ratio in the lentiform nucleus and the parietal cortex contralateral to the most affected side (Fig. 1). A reduction in NAA/Ch and NAA/Cr ratios in the lentiform nucleus was also observed by Federico et al. (18) in seven patients with MSA and seven patients with PSP. All three studies additionally examined the proton spectra in a group of PD patients and found no abnormalities in the selected region of interest (15,18,19). It should be noted, however, that Clarke et al. failed to find any abnormality for NAA, Ch, and Cr in six patients with probable MSA (26). In summary, the published data suggest that proton MRS may be of potential diagnostic value in atypical parkinsonian disorders. However, the demonstration of significant group differences in patients with well-defined clinical features does not imply that proton MRS can reliably discriminate between PD and atypical parkinsonian disorders in individual patients. A recent study by Alexon et al. used pattern recognition techniques (i.e., neural network and related data analyses) to analyze proton spectra in 15 patients with probable PD, 11 patients with possible PD, 5 patients with atypical PD, and 14 healthy age-matched controls (27). In contrast to conventional analyses, all information within the proton spectrum can be entered in the statistical analysis simultaneously. The neuronal networks approach allowed them to distinguish between the four groups with considerable accuracy; approximately 88% of the predictions were correct. By contrast, conventional analysis revealed no significant differences in metabolite ratios among groups. Proton MRS of the basal ganglia in conjunction with statistical analyses that take into account the pattern of the entire proton spectrum may help to distinguish PD from atypical parkinsonian disorders at initial presentation. Discriminative power may be further increased by using a multimodal imaging approach that combines MRS with other imaging techniques such as structural MRI or 18F-6-fluorodopa PET. 454 Siebner and Deuschl Fig 1. H-MRS findings in control subjects and patients with parkinsonian disorders.PSP, progressive supranuclear palsy; PD, Parkinson’s disease; CBD, corticobasal degeneration. Columns and error bars present means ± SD. Asterisks indicate significant differences between controls and PSP patients and between controls and CBD (*p = 0.05, **p < 0.01, ***p < 0.001). The data were taken from Table 2 published in ref. 19. Phosphorus MRS provides information on levels of cerebral phospholipids and high-energy phosphates. The cerebral phosphorus spectra contains at least seven resonances that can be attributed to phosphomonoesters (PME), inorganic phosphate (Pi), phosphodiesters (PDE), phosphocreatine (PCr), and adenosine triphosphate (ATP). So far, only one group has used MRS to investigate the phosphorus spectra in 13 patients with PD and 15 patients with MSA (28). Assuming a constant cytosolic concentration of ATP, Barbiroli et al. measured PCr and Pi and calculated cytosolic pH and free Mg2+ (28). Compared with an age-matched control group, patients with PD showed a significant increase in Pi and a decrease in cytosolic free Mg2+, whereas PCr was reduced and Pi was increased in patients with MSA. In the MSA group, there was no difference in the phosphorus spectra between the MSA-P and the MSA-C variants of MSA. A discriminant analysis that considered only the concentrations of PCr and Mg2+ provided a correct classification of MSA and PD patients in 93% of the cases. These preliminary data suggest that, in addition to proton MRS, phosphorus MRS may be useful to probe cerebral phosphate metabolism and ion contents in patients with atypical parkinsonian disorders. DIFFUSION-WEIGHTED MAGNETIC RESONANCE IMAGING Water diffusion-weighted MRI produces quantitative maps of microscopic displacement of water molecules that occur as part of the physical diffusion process. This is achieved by sensitizing the magnetic resonance signal to the random motion of water molecules by using strong magnetic field gradients. By varying the magnetic field gradient, one can obtain different degrees of diffusionweighted images and calculate an apparent diffusion coefficient (ADC) for each voxel (5). Since diffusion of water molecules is highly sensitive to microstructural changes in the cerebral tissue, diffusion-weighted MRI has become a firmly established method to probe the functional integrity of brain tissue, especially in acute cerebral ischemia (29). Diffusion-weighted MRI has a high sensitivity to detect structural abnormalities. However, it is important to bear in mind that diffusionweighted MRI has a low specificity in terms of underlying pathophysiology since various mechanisms (e.g., edema, neurotoxicity, Wallerian degeneration) can affect the diffusion process in the cerebral tissue. Functional MRI Techniques in Atypical Parkinsonism 455 Three studies have characterized water diffusion in patients with atypical parkinsonian disorders. Patients with PSP showed an increase in ADCs in the prefrontal and precentral white matter (30) and the basal ganglia (31,32). An increase in ADCs was also found in patients with the MSA-P variant of MSA (32), but not in patients with PD (31,32). These data indicate that diffusion-weighted imaging may help to distinguish between PD and atypical parkinsonian disorders, but fails to discriminate between PSP and MSA. The microstructure of the brain tissue imposes directional constraints to the diffusion of water molecules in the brain (referred to as anisotropy). Diffusion is particularly anisotropic in white matter tracts because water preferentially diffuses along the direction of white matter fibres. Anisotropic diffusion is more adequately characterized by a diffusion tensor. A diffusion tensor is an array of nine coefficients that fully characterizes the directional properties of water diffusion in space. Diffusion tensor-encoded MRI (DT-MRI) uses different gradient orientations to characterize the diffusion tensor in each voxel of the brain (5). The diffusion tensor is often displayed as an elipsoid (5). The average size of the ellipsoid represents the overall displacement of the water molecules in a given voxel (mean diffusivity). The eccentricity of the ellipsoid characterizes the degree of anisotropy. A sphere indicates isotropic diffusion whereas an elongated (cigar-shaped) or flat (pancakeshaped) ellipsoid indicates anisotropic diffusion. The main axis of the ellipsoid corresponds to the preferential direction of diffusion. In the white matter, the main axis of the diffusion tensor is thought to represent the prevailing orientation of white matter bundles in each voxel. DT-MRI allows one to track white matter fibers by connecting neighboring voxels on the basis of their main direction of the diffusion tensor (i.e., main fiber orientation) (33). Anisotropy measurements can be used to identify subtle abnormalities in the organization of white matter tracks that are not evident with plain, anatomical MRI (34). However, it is worth bearing in mind that currently available DT-MRI techniques can only visualize white matter bundles that consist of a large number of axons, limiting fiber tracking to the white matter. Furthermore, DT-MRI can not probe the directional and functional status of the information flow along the white matter tracts. DT-MRI also has a considerable potential for functional mapping of subcortical gray matter. A recent study employed DT-MRI to differentiate the nuclei in the thalamus and to map their connectivity (35). Because DT-MRI provides a unique approach to tracking anatomical connectivity in vivo, DT-MRI can provide important new insights into the neuroanatomical basis of atypical parkinsonian disorders linking clinical symptoms with impaired anatomical connectivity. Though no DT-MRI study has been published on atypical parkinsonian disorders at this stage, it is safe to state that DT-MRI provides a promising tool to pinpoint characteristic patterns of abnormal connectivity, especially in CBD and MSA. This may be used to separate atypical parkinsonian disorders from PD. MRI-BASED MORPHOMETRY MRI-based volumetry of structural MR images can reveal the pattern of atrophic changes in patients with atypical parkinsonian syndromes. Using a region-of-interest (ROI) analysis, it has been shown that the patterns of atrophy in predefined regions of interest allow the separation PD from MSA and PSP (36) as well as PSP from CBD (37). For instance, a recent study by Gröschel and colleagues demonstrated that the volumes of midbrain, parietal white matter, temporal gray matter, brainstem, frontal white matter, and pons separate best between patients with PSP or CBD (37). A stepwise linear discriminant analysis resulted in two canonical discriminant functions, which allowed for the correct prediction of the diagnosis in 95% of healthy control subjects as well as in 76% of all PSP and 83% of all CBD patients (37). The discriminant functions revealed similar results in patients with definite PSP/CBD and in patients with possible and probable PSP/CBD (37). Prospective studies are now needed to show whether MRI-based volumetry will have clinical applicability. 456 Siebner and Deuschl In recent years, voxel-based morphometry (VBM) of structural MRI data has been introduced as a simple and objective approach for characterizing small-scale differences in white and gray matter (36). VBM refers to a voxel-wise statistical comparison of the local concentration of gray (or white) matter between two groups of subjects. The procedure involves spatial normalization of high-resolution MR images into the same stereotactic space followed by segmentation of the gray (or white) matter. The smoothed gray matter segments are then compared using parametric statistical tests and the theory of Gaussian random fields (38). Other voxel-based morphometric approaches, such as deformation-based or tensor-based morphometry, allow the study of regional differences in brain shapes between groups of subjects (38). In contrast to conventional ROI analyses, VBM and related approaches provide whole-brain coverage and are highly sensitive to subtle structural changes within a single brain region. Since VBM is an automated procedure, the analysis is highly observer independent. Finally, VBM is not affected by partial volume effects. VBM cannot only be applied to highresolution structural MRI, but VBM can also be used to investigate between-group differences of ADC maps or fractional anisotropy maps. This allows to screen for regional changes in neuronal integrity (i.e., VBM of ADC maps) or regional changes in fiber orientation (i.e., VBM of DT-weighted MRI). FUTURE DIRECTIONS Apart from proton MRS, none of the MRI approaches described in this chapter have yet been used to study the pathophysiology of atypical parkinsonian disorders. Therefore, the potential of these techniques for the diagnosis and research of atypical parkinsonian disorders remains to be defined. Based on the MRI experience gathered with other neuropsychiatric disorders, we anticipate that fMRI, MRS, and water diffusion MRI will significantly contribute to early diagnosis and advance our understanding of pathophysiological evolution of the different atypical parkinsonian disorders. Future advances in MR technology and new MR techniques (e.g., magnetization transfer technique) will further increase the diagnostic and research potential of MRI in parkinsonian disorders (39). It is important to bear in mind that these MRI techniques can readily be combined with each other and with high-resolution structural MRI. Indeed, multimodal MRI studies that combine structural and functional MR techniques represent the most promising approach to exploit MRI as a research tool. Since VBM of structural MRI images maps the pattern of structural abnormalities, VBM provides complementary anatomic information for the interpretation of altered neuronal activity as revealed by fMRI. The same applies for DT-MRI which, in combination with fMRI, might provide important clues to altered functional connectivity in patients with atypical parkinsonism. On an individual basis, interfacing fMRI with structural MRI and DT-MRI may considerably enhance diagnostic accuracy of MRI in the differential diagnosis of the atypical parkinsonian disorders. ROLE OF FUNCTIONAL MAGNETIC RESONANCE IMAGING IN DIAGNOSIS AND RESEARCH OF ATYPICAL PARKINSONIAN SYNDROMES A. Functional magnetic resonance imaging (fMRI) Mapping the functional consequences of neurodegeneration Assessing the effect of therapeutic interventions Monitoring disease progression B. Magnetic resonance spectroscopy (MRS) Noninvasive characterization of regional abnormalities in tissue metabolism Discrimination between PD and atypical parkinsonian syndromes C. Diffusion-weighted magnetic resonance imaging (dMRI) Probing for microstructural changes in the cerebral tissue (ADC-maps) Mapping abnormalities in the organization of white matter tracts (DT-imaging) PD, Parkinson’s disease; ADC, apparent diffusion coefficient; DT, diffusion tensor. Functional MRI Techniques in Atypical Parkinsonism 457 REFERENCES 1. Turner R, Howseman A, Rees GE, Josephs O, Friston K. Functional magnetic resonance imaging of the human brain: data acquisition and analysis. Exp Brain Res 1998;123:5–12. 2. Logothetis NK. The neural basis of the blood-oxygen-level-dependent functional magnetic resonance imaging signal. Phil Trans R Soc Lond B 2002;357:1003–1037. 3. Rudkin TM, Arnold DL. Proton magnetic resonance spectroscopy for the diagnosos and management of cerebral disorders. Arch Neurol 1999;56:919–926. 4. Ross B, Bluml S. Magnetic resonance spectroscopy of the human brain. Anat Rec 2001;265:54–84. 5. Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nature Rev Neurosci 2003;4: 469–480. 6. Brooks DJ. Morphological and functional imaging studies on the diagnosis and progression of Parkinson´s disease. J Neurol 2000;247(Suppl 2):11–18. 7. Ceballos-Baumann AO. Functional imaging in Parkinson´s disease: activation studies with PET, fMRI and SPECT. J Neurol 2003;250(Suppl 1):15–23. 8. Ogawa S, Lee TM, Nayak As, Glynn P. Oxygenation-sensitive contrast in magnetic reonance image of rodent brain at high magnetic fields. Magn Resonance Med 1990;14:68–78. 9. Sabatini U, Boulanouar K, Fabre N, Martin F, Carel C, Colonnese C, et al. Cortical motor reorganization in akinetic patients with Parkinson’s disease: a functional MRI study. Brain 2000;123:394–403. 10. Haslinger B, Erhard P, Kampfe N, Boecker H, Rummeny E, Schwaiger M, et al. Event-related functional magnetic resonance imaging in Parkinson’s disease before and after levodopa. Brain 2001;124:558–570. 11. Buhmann C, Glauche V, Sturenburg HJ, Oechsner M, Weiller C, Buchel C. Pharmacologically modulated fMRI: cortical responsiveness to levodopa in drug-naive hemiparkinsonian patients. Brain 2003;126:451–461. 12. Rowe J, Stephan KE, Friston K, Frackowiak R, Lees A, Passingham R. Attention to action in Parkinson’s disease: impaired effective connectivity among frontal cortical regions. Brain 2002;125:276–289. 13. Mattay VS, Tessitore A, Callicott JH, Bertolino A, Goldberg TE, Chase TN, et al. Dopaminergic modulation of cortical function in patients with Parkinson’s disease. Ann Neurol 2002;51:156–164. 14. Brooks D. Diagnosis and management of atypical parkinsonian syndromes. J Neurol Neurosurg Psychiatry 2002;72(Suppl.1):i10–i16. 15. Davie CA, Wenning GK, Barker GJ, Tofts PS, Kendall BE, Quinn N, et al. Differentiation of multiple system atrophy from idiopathic Parkinson’s disease using proton magnetic resonance spectroscopy. Ann Neurol 1995;37:204–210. 16. Holshouser BA, Komu M, Moller HE, Zijlmans J, Kolem H, Hinshaw DB Jr, et al. Localized proton NMR spectroscopy in the striatum of patients with idiopathic Parkinson’s disease: a multicenter pilot study. Magn Reson Med. 1995;33:589–594. 17. Clarke CE, Lowry M, Horsamn A. Unchanged basal ganglia N-acetylaspartate and glutamate in idiopathic Parkinson´s disease as measured by proton magnetic resonance spectroscopy. Mov Dis 1997;12:297–301. 18. Federico F, Simone IL, Lucivero V, De Mari M, Giannini P, Iliceto G, et al. Proton magnetic resonance spectroscopy in Parkinson’s disease and progressive supranuclear palsy. J Neurol Neurosurg Psychiatry. 1997;62:239–242. 19. Tedeschi G, Litvan I, Bonavita S, Bertolino A, Lundbom N, Patronas N J, et al. Proton magnetic resonance spectroscopic imaging in progressive supranuclear palsy, Parkinson’s disease and corticobasal degeneration. Brain 1997;120:1541–1552. 20. Choe BY, Park JW, Lee KS, Son BC, Kim MC, Kim BS, et al. Neuronal laterality in Parkinson’s disease with unilateral symptom by in vivo 1H magnetic resonance spectroscopy. Invest Radiol. 1998;33:450–455. 21. Hoang TQ, Bluml S, Dubowitz DJ, Moats R, Kopyov O, Jacques D, et al. Quantitative proton-decoupled 31P MRS and 1H MRS in the evaluation of Huntington’s and Parkinson’s diseases. Neurology 1998;50:1033–1040. 22. Hu MT, Taylor-Robinson SD, Chaudhuri KR, Bell JD, Morris RG, Clough C, et al. Evidence for cortical dysfunction in clinically non-demented patients with Parkinson’s disease: a proton MR spectroscopy study. J Neurol Neurosurg Psychiatry 1999;67:20–26. 23. Lucetti C, Del Dotto P, Gambaccini G, Bernardini S, Bianchi MC, Tosetti M, et al. Proton magnetic resonance spectroscopy (1H-MRS) of motor cortex and basal ganglia in de novo Parkinson’s disease patients. Neurol Sci 2001;22:69–70. 24. O’Neill J, Schuff N, Marks WJ Jr, Feiwell R, Aminoff MJ, Weiner MW. Quantitative 1H magnetic resonance spectroscopy and MRI of Parkinson’s disease. Mov Disord 2002;17:917–927. 25. Summerfield C, Gomez-Anson B, Tolosa E, Mercader JM, Marti MJ, Pastor P, et al. Dementia in Parkinson disease: a proton magnetic resonance spectroscopy study. Arch Neurol. 2002;59:1415–1420. 26. Clarke CE, Lowry M. Basal ganglia metabolite concentrations in idiopathic Parkinson’s disease and multiple system atrophy measured by proton magnetic resonance spectroscopy. Eur J Neurol 2000;7:661–665. 27. Axelson D, Bakken IJ, Susann Gribbestad I, Ehrnholm B, Nilsen G, Aasly J. Applications of neural network analyses to in vivo 1H magnetic resonance spectroscopy of Parkinson disease patients. J Magn Reson Imaging. 2002;16:13–20. 28. Barbiroli B, Martinelli P, Patuelli A, Lodi R, Iotti S, Cortelli P, et al. Phosphorus magnetic resonance spectroscopy in multiple system atrophy and Parkinson’s disease. Mov Disord 1999;14:430–435. 458 Siebner and Deuschl 29. Moseley ME, Kucharczyk J, Mintorovitch J, Cohen Y, Kurhanewicz J, Derugin N, et al. Diffusion-weighted MRimaging of acute stroke.: correlation with T2-weighted an magnetic susceptibility-enhanced imaging in cats. Am L Neuroradiol 1990;11;423–429. 30. Oshiata T, Oka M, Imon Y, Yamaguchi S, Mimori Y, Nakamura S. Apparent diffusion coefficient measurements in progressive nuclear palsy. Neuroradiology 2000;42:643–647. 31. Schocke MF, Seppi K, Esterhammer R, Kremser C, Jaschke W, Poewe W, et al. Diffusion-weighted MRI differentiates the Parkinson variant of multiple system atrophy from PD. Neurology 2002;58:575–580. 32. Seppi K, Schocke MF, Esterhammer R, Kremser C, Brenneis C, Mueller J, et al. Diffusion-weighted imaging discriminates progressive supranuclear palsy from PD, but not from the parkinson variant of multiple system atrophy. Neurology 2003;60:922–927. 33. Conturo TE, Lori NF, Cull TS, Akbudak E, Snyder AZ, Shimony JS, et al. Tracking neuronal fibre pathways in the living human brain. Proc Natl Acad Sci USA 1999;96:10422–10427. 34. Sommer M, Koch MA, Paulus W, Weiller C, Buechel C. Disconnection of speech-relevant brain areas in persistent developmental stuttering. Lancet 2002;360:380–383. 35. Behrens TE, Johansen-berg H, Woolrich MW, Smith SM, Wheeler-Kingshott CA, Boulby PA, et al. Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat Neurosci 2003;6:750–757. 36. Schulz JB, Skalej M, Wedekind D, Luft AR, Abele M, Voigt K, et al. Magnetic resonance imaging-based volumetry differentiates idiopathic Parkinson´s syndrome from multiple system atrophy and progressive supranuclear palsy. Ann Neurol 1999;45:65–74. 37. Gröschel K, Hauser TK, Luft A, Patronas N, Dichgans J, Litvan I, et al. Magnetic resonance imaging-based volumetry differentiates progressive supranuclear palsy from corticobasal degeneration. Neuroimage 2004;21:714–724. 38. Ashburner J, Friston K. Voxel-based morphometry—the methods. Neuroimage 2000;11:805–821. 39. Hanyu H, Asano T, Sakurai H, takasaki M, Shindo H, Abe K. Magnetisation transfer measurements of the subcortical grey and white matter in Parkinson´s disease with and without dementia in progressive nuclear palsy. Neuroradiology 2001;43:542–546.