Evidence-Based Imaging I. Title Imaging evaluation of sinusitis: Impact on Health Outcome
advertisement
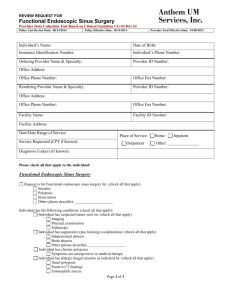
Back to Contents Page Evidence-Based Imaging I. Title Imaging evaluation of sinusitis: Impact on Health Outcome II. Authors Yoshimi Anzai, MD Department of Radiology University of Washington Williams Neighbor, MD Department of Family Medicine University of Washington KEY POINTS Issues 1. Acute sinusitis A: How can we identify patients with acute sinusitis who will benefit from antibiotic treatment? B: How accurate are imaging studies for diagnosis of acute bacterial sinusitis? Special case: Pediatric acute sinusitis Special case: Cost-Effectiveness Analysis in acute sinusitis 2. Chronic sinusitis A: How can we diagnose chronic sinusitis? IV. Key Points - Acute bacterial sinusitis is over-diagnosed clinically and antibiotics are overprescribed, leading to antibiotics resistant infections. We need to differentiate patients with acute bacterial sinusitis who may benefit from antibiotic treatment from those with an uncomplicated upper respiratory viral infection (STRONG EVIDENCE). - Although a CT scan is frequently performed to assist diagnosis of sinusitis, no adequate data exists on the sensitivity and specificity of sinus CT for diagnosis of acute bacterial sinusitis. (LIMITED EVIDENCE). - The diagnosis of chronic sinusitis is based on clinical grounds. No gold standard exists to confirm clinical diagnosis. CT findings for chronic sinusitis often do not correlate with patients' clinical symptoms. (LIMITED EVIDENCE). - CT influences surgeons' decision regarding which patients will undergo sinus surgery, in addition to providing anatomic information to guide endoscopic sinus surgery (LIMITED EVIDENCE). X. Discussion of Issues Acute Sinusitis Issue 1: How can we identify patients with acute sinusitis who benefit from antibiotic treatment? Summary How to determine which sinusitis patients should receive antibiotic treatment and how to distinguish those patients from ones with uncomplicated upper respiratory tract infection are questions that have been studied in detail in the clinical literature. The majority of the literature supports using clinical guidelines to select patients with acute bacterial sinusitis and recommends the first-line antibiotic treatment (amoxicillin) for patients with severe symptoms and illness longer than 7 days. Imaging studies are not routinely recommended for initial diagnosis of acute sinusitis (Limited Evidence). Evidence of imaging accuracy for diagnosis of acute sinusitis is extremely limited. Issue 2: How accurate are imaging studies for the diagnosis of acute bacterial sinusitis? Summary There is no single report from the U.S. concerning testing sensitivity or specificity of CT compared with a sinus puncture and culture of aspirate, which is the gold standard of acute bacterial sinusitis. Only one report measured PPV compared with the gold standard of sinus aspiration. Sinus radiography has been reported to have moderate sensitivity. Sinus CT is reported to be more sensitive than sinus radiography, but little is known about its specificity (Insufficient Evidence). Special Cases: Pediatric Sinusitis Imaging diagnosis of acute sinusitis in children is challenging. The paranasal sinuses are in the process of development and mucosal thickening or fluid collection is physiologically seen in such developing sinuses. Once sinuses are well developed and pneumatized, then diagnosis with sinus CT or radiography is similar to what is observed in an adult population. A clinical practice guideline regarding the diagnosis, evaluation, and treatment of children with acute bacterial sinusitis recommends that the diagnosis of acute bacterial sinusitis be based on clinical criteria in children six years or younger who present with upper respiratory symptoms that are either persistent or severe. Although controversial, imaging studies may be necessary to confirm a diagnosis of acute bacterial sinusitis in children older than six years. CT scans of the paranasal sinuses should be reserved for children who present with complications of acute bacterial sinusitis or who have very persistent or recurrent infections and are not responsive to medical management (Moderate Evidence). There are only 5 controlled randomized trials and 8 case series on antibiotic therapy for acute bacterial sinusitis in children. A placebo-controlled randomized trial by Garbutt et al revealed that no significant difference in the clinical improvement of children treated with antibiotics compared with those with a placebo. However, children with complications or suspected complications of acute bacterial sinusitis should be treated promptly and aggressively with antibiotics and, when appropriate, drainage. Special Cases: Cost-effectiveness Analysis (CEA) in acute sinusitis A few studies have rigorously addressed the cost effectiveness of diagnosis and treatment for acute sinusitis. Balk et al reported on strategies for diagnosing and treating suspected acute bacterial sinusitis. They created a Markov model to examine four strategies for acute sinusitis: 1) no antibiotic treatment; 2) empirical antibiotic treatment; 3) clinical criteria-guided treatment; and 4) radiography-guided treatment. The model simulated a 14-day course of illness and included sinusitis prevalence and symptom severity. They concluded that the use of clinical criteria guided treatment was cost-effective in most cases. The empirical use of antibiotics was cost-effective with higher prevalence. Sinus radiography-guided treatment was never cost-effective for initial treatment. A meta analysis by the AHRQ also reported that treatment of uncomplicated sinusitis with amoxicillin or folate inhibitors based on clinical criteria is the most cost-effective strategy. Fagnan et al also stated that sinus radiography and CT generally were not cost effective in making an initial diagnosis. Most of the literature suggests that sinus radiography is not recommended for the diagnosis of routine cases. The role of sinus radiograph is limited based on the literatures, which is in part due to the limited sensitivity or specificity but also to the added cost for diagnosis of this highly prevalent disease. A practice guide based on consensus of Canadian and American experts in infectious diseases, microbiology, otolaryngology and family medicine states that radiography is not warranted when the likelihood of acute sinusitis is high or low but is useful when the diagnosis is in doubt (Limited Evidence). The limitations of these CEAs are the unrealistic assumption that patients receive the first line antibiotic, amoxicillin, which is inexpensive. Increasing numbers of physicians, however, prescribe more expensive broad-spectrum antibiotics, in part due to prevalent amoxicillin resistant infections in the community. Moreover, the model used in the CEA by Balk did not account for downstream societal cost of increasing antibiotic resistant infection. If a diagnosis of acute sinusitis is made by a definitive test, such as CT, it may potentially reduce necessity of antibiotic treatment. Chronic Sinusitis Issue 1: How Can We Diagnose Chronic Sinusitis? Summary A diagnosis of chronic sinusitis is usually based on clinical history and physical examination. It is not a pathological diagnosis and, thus, patients' symptoms drive medical care. Sinus CT may show mucosal thickening in various degrees, from minimal mucosal thickening to severe opacification of the paranasal sinuses. Mucosal thickening on CT is non-specific and could be subtle, since many patients have been treated with antibiotics or anti-inflammatory medication prior to CT. Occasionally, bone thickening or sclerosis of the affected sinus is seen, suggestive of chronic periosteal inflammation. Issue 2: What is the role of imaging in chronic sinusitis? Does imaging change treatment decision-making? Summary The roles of sinus CT for chronic sinusitis patients are to support clinical diagnosis, to evaluate the extent of disease, and to provide detailed anatomy to assist treatment planning. The literature suggests that sinus CT findings do not always correlate with patients' clinical symptoms. Whether patients with a normal CT but with persistent clinical symptoms should undergo surgery remains controversial. There is not enough evidence that sinus CT predicts clinical outcomes or whether sinus CT affects treatment decisions. Evidence for the cost effectiveness analysis of diagnosis and treatment of chronic sinusitis is lacking (Insufficient Evidence). Back to Contents Page