COPD Ambulatory Rotation - Block 4 Ryan Burris Brian Dang
advertisement

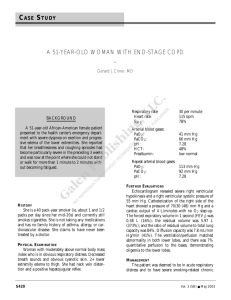
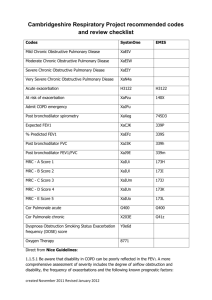
COPD Ambulatory Rotation - Block 4 Ryan Burris Brian Dang Minh-Phuong (Michelle) Le Jennifer Mah Ben Yip COPD Definition • The Global Initiative for Chronic Obstructive Lung Disease (GOLD) and World of Health Organization (WHO) Definition: "Chronic obstructive pulmonary disease (COPD), a common preventable and treatable disease, is characterized by airflow limitation that is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases. Exacerbations and comorbidities contribute to the overall severity in individual patients.” COPD Diagnosis • Symptoms of COPD – – – – – Dyspnea on exertion or rest Cough Cachexia, cyanosis Wheezing Limitation of activities • Smoking history – Obtain a pack year history; the higher the PY, the greater the risk of developing COPD. • Environmental history • Occupational history COPD Diagnosis • Pulmonary function tests – FEV1/FVC < 70% – FEV1 < 80% • CXR – Hyperinflation – Flattened diaphragms – Long narrow heart – Interstitial markings and bullae COPD Diagnosis COPD Diagnosis • Other clues but not necessary for diagnosis – ABG with hypercapnia and hypoxemia – Decreased DLCO – Negative BNP – Spirometry shows • Dec IC and VC • Increased TLC, FRC, and RV due to hyperinflation COPD Diagnosis • Rule out other DDX of symptoms and obstructive disease – Can rule out asthma with • Bronchodilator challenge: Positive if improvement of FEV1 ≥ 12% after albuterol • Methacholine challenge: Positive if decrease in FEV1 ≤ 20% with methacholine – – – – – Alpha 1 anti-trypsin deficiency Congestive heart failure Bronchiectasis Bronchitis Tuberculosis COPD Severity TREATMENT OPTIONS? Non-Pharmacologic Therapy • • • • Smoking cessation Reduce environmental exposures Physical activity Vaccinations – Influenza, pneumococcal • Supplemental O2 • Pulmonary rehabilitation • CPAP Pharmacologic Therapy Bronchodilators • Beta2 agonists • Anticholinergics • Theophylline (methylxanthine) Inhaled Corticosteroids • For FEV1 < 60% • Don’t use as monotherapy! Many different combinations… Class Generic Brand SA beta2-agonists Albuterol ProAir, Proventil LA beta2-agonists Formoterol Salmeterol SA anticholinergics Ipratropium bromide Atrovent LA anticholinergics Tiotropium Spiriva Combo SA beta agonist + anticholinergic Albuterol/Ipratropium Combivent ICS Beclomethasone Budesonide Fluticasone Combo LA beta agonist + corticosteroid Formoterol/Budesonide Salmeterol/Fluticasone Symbicort Advair Practically speaking, what do I use? Patient Group First Choice Generic Brand Names A SA anticholinergic prn Ipratropium Atrovent or SA beta agonist prn or Albuterol or ProAir LA anticholinergic Tiotropium Spiriva or LA beta agonist or Formeterol or Salmeterol or Formeterol or Salmeterol ICS + LA beta agonist Formoterol/Budesonide Salmeterol/Fluticasone Symbicort or Advair or Tiotropium or Spiriva Formoterol/Budesonide Salmeterol/Fluticasone and/or Tiotropium Symbicort or Advair and/or Spiriva B C or LA anticholinergic D ICS + LA beta agonist and/or LA anticholinergic Patient Group First Choice Alternative Other Options A SA anticholinergic prn LA bronchodilator Theophylline or SA beta agonist prn or SA beta agonist + SA anticholinergic LA anticholinergic LA anticholinergic and LA beta agonist B or LA beta agonist SA beta agonist and/or SA anticholinergic Theophylline C ICS + LA beta agonist or LA anticholinergic LA anticholinergic and LA beta agonist or LA anticholinergic + PDE-4 inhibitor SA beta agonist and/or SA anticholinergic Theophylline or LA beta agonist and PDE-4 inhibitor D ICS + LA beta agonist and/or LA anticholinergic ICS + LA beta agonist and LA anticholinergic or ICS + LA beta agonist and PDE-4 inhibitor or LA anticholinergic and LA beta agonist or LA anticholinergic and PDE-4 inhibitor Carbocysteine SA beta agonist and/or SA anticholinergic Theophylline ACUTE EXACERBATIONS Exacerbation - Definition • An acute event characterized by a worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication – Changes in dyspnea, cough, and/or sputum production • Precipitants: most common causes are viral upper respiratory tract infections and infection of tracheobronchial tree; air pollutants • Clinical diagnosis based on presentation of the patient Its significance? • Negatively affect a patient’s quality of life • Have effects on symptoms and lung function that take weeks to recover • Accelerate the rate of decline of lung function • Associated with significant mortality, particularly in those requiring hospitalization • High socioeconomic costs Where to treat patient? Treatments • Ipratropium + albuterol (metered dose inhaler or nebulizer): 1st line • Corticosteroids: increase FEV1 but no mortality benefit (prednisolone x10-14d or methylprednisolone x72h) • +/- Antibiotics x5-10d: increase in dyspnea, sputum volume, sputum purulence – amox, bactrim, doxy, clarithro, cipro/levo – Haemophilus influenzae, Streptococcus pneumoniae, Moraxella catarrhalis – GOLD 3 & 4: Pseudomonas aeruginosa • Intravenous methylxanthines (theophylline or aminophylline): only in selected cases when response to short-acting bronchodilators is insufficient Oxygenation • Supplemental O2: goal SaO2 88-92%, PaO2 55-60 – Helps to prevent intubation, decrease in mortality – Not for AMS, cannot clear secretions, HD instability, UGIB • Intubation: acidosis, PaO2 <55-60, high PaCO2, worsening dyspnea, not NPPV candidate Treatment Goals • Minimize the impact of the current exacerbation • Prevent the development of subsequent exacerbations • Abx and steroid: shorten recovery time, improve lung function (FEV1) & arterial hypoxemia (PaO2), reduce the risk of early relapse, treatment failure, and length of hospital stay MKSAP QUESTIONS! MKSAP Question 1 • A 48 year old man is evaluated for a 1-year history of cough. He has not had dyspnea, abdominal pain, heartburn, or change in appetite or weight. He has a 30 pack year history of smoking. He does not have seasonal allergies. His medical history is significant for hypertension that is treated with losartan. • On physical examination, vital signs are normal. Pulmonary examination discloses normal breath sounds that are equal bilaterally with no wheezing. No nasal polyps are noted. Abdominal examination is unremarkable. There is no cyanosis, clubbing, or edema. Pulmonary function tests disclose an FEV1 of 75% of predicted and an FEV1/FVC ratio of 63%. Following administration of a bronchodilator, there is no significant change in the FEV1/FVC ratio, and the FEV1 is 83% of predicted. Chest radiography shows no masses and normal lung markings. MKSAP Question 1 • Which of the following is the most likely cause of this patient’s cough? – A) Asthma – B) COPD – C) Gastroesophageal reflux disease – D) Losartan MKSAP Question 1 • Which of the following is the most likely cause of this patient’s cough? – A) Asthma – B) COPD – C) Gastroesophageal reflux disease – D) Losartan MKSAP Answer 1 • The most likely cause of this patient’s cough is COPD. His post bronchodilator FEV1/FVC ratio less than 70% confirms airflow limitation and a diagnosis of obstructive lung disease’ his relatively preserved FEV1 suggests that his COPD is mild. COPD should be considered in any patient older than 40 years who has dyspnea, chronic cough or sputum production, and/or a history of risk factors (such as exposure to tobacco smoke, dust, chemicals, outdoor air pollution, or biomass smoke). Spirometry is the gold standard for diagnosing COPD and monitoring its progress; it should be done to confirm the diagnosis and to exclude other diseases. The American College of Physicians and Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines require an FEV1/FVC ratio of less than 70% of predicted to establish the diagnosis of COPD. The GOLD guidelines use the degree of airflow obstruction as measured by the FEV1 to further describe the level of disease. Level 1 (mild) COPD is characterized by an FEV1 of 80% of predicted or greater; Level 2 (moderate) COPD is characterized by an FEV1 of 50% to 79% of predicted; Level 3 (Severe) COPD is characterized by an FEV1 of 30% to 49% of predicted; and Level 4 (Very severe) COPD is characterized by an FEV1 less than 30% of predicted. MKSAP Answer 1 • Although asthma may present with cough, it is unlikely in this patient owing to the lack of atopy and history of respiratory symptoms as a child or any other clinical findings consistent with bronchospasm • Gastroesophageal reflux disease may cause cough; however, COPD is the more likely cause of cough in this patient who does not have heartburn symptoms, has a history of smoking, and demonstrates airflow obstruction on pulmonary function testing. • ACE inhibitors may be associated with cough, but angiotensin receptor blockers (such as losartan) have a significantly lower rate of cough as a side effect and would not be a likely cause of this patient’s cough given his other clinical parameters. MKSAP Question 2 • A 66 year old man is evaluated in the intensive care unit for possible extubation. He was admitted for a severe COPD exacerbation 3 days ago. His carbon dioxide remained markedly elevated despite a trial of noninvasive ventilation, and he was therefore intubated and placed on invasive mechanical ventilation. He has improved with treatment of his COPD. His medications are methylprednisolone, albuterol, ipratropium, propofol, and levofloxacin. • On physical examination, he is awake and responsive. Temperature is 37.0 °C (98.6 °F), blood pressure is 138/82 mm Hg, pulse rate is 96/min, and respiration rate is 20/min. Pulmonary examination reveals decreased breath sounds bilaterally with no wheezing. Accessory muscle use is noted. A small amount of thin secretions is noted with endotracheal suctioning. • Arterial blood gas levels have returned to baseline, with a pH of 7.36, a PCO2 of 55 mm Hg (7.3 kPa), and a PO2 of 70 mm Hg (9.3 kPa) on an FIO2 of 0.35. He tolerates a weaning trial well and the decision is made to extubate. MKSAP Question 2 • Which of the following interventions will decrease this patient's risk for reintubation? – A) Incentive spirometry every 2 hours – B) Inhaled helium-oxygen mixture – C) Nebulized N-acetylcysteine – D) Noninvasive positive pressure ventilation MKSAP Question 2 • Which of the following interventions will decrease this patient's risk for reintubation? – A) Incentive spirometry every 2 hours – B) Inhaled helium-oxygen mixture – C) Nebulized N-acetylcysteine – D) Noninvasive positive pressure ventilation MKSAP Answer 2 • • • • The most appropriate intervention at the time of extubation is noninvasive positive pressure ventilation (NPPV). Application of NPPV shortly after extubation for a 24-hour period reduced the need for reintubation in previous trials of intubated patients with chronic lung disease and hypercapnia after a successful weaning trial. This population also appears to benefit from NPPV even if it is not applied until after the patient has developed respiratory failure following extubation. However, studies enrolling unselected patients with postextubation respiratory failure indicate that the use of NPPV may actually increase mortality. The use of incentive spirometry reduces the risk of postoperative pulmonary complications but does not have a role in the routine management of nonsurgical patients following extubation. The reduced gas density of helium-oxygen mixtures (heliox) reduces resistance to airflow, and thereby the work of breathing, in patients with obstructive lung disease. However, there is insufficient evidence to support the routine use of heliox in the management of COPD exacerbations. N-acetylcysteine is a mucolytic agent that has been used to thin secretions in patients with excess mucus production. However, N-acetylcysteine is less likely to benefit this patient because he had minimal secretions prior to extubation. Furthermore, nebulized N-acetylcysteine may trigger bronchospasm. MKSAP Question 3 • A 70-year-old woman is evaluated during a routine examination. She has severe COPD with recurrent exacerbations and decreasing exercise capacity. She does not have cough or fever, but she has dyspnea with activities of daily living. She stopped smoking 1 year ago and is adherent to her medication regimen. Her inhaler technique is good. Her medications are fluticasone/salmeterol, tiotropium, and an albuterol inhaler as needed. • On physical examination, pulse rate is 80/min and respiration rate is 22/min; BMI is 22. Pulmonary examination reveals diminished breath sounds that are equal bilaterally. No wheezing or crackles are noted. FEV1 is 45% of predicted. Oxygen saturation is 92% at rest and 90% after exertion breathing ambient air. Chest radiograph shows no infiltrate or mass. MKSAP Question 3 • Which of the following is the most appropriate management? – A) Morphine – B) Oxygen therapy – C) Prednisone – D) Pulmonary rehabilitation MKSAP Question 3 • Which of the following is the most appropriate management? – A) Morphine – B) Oxygen therapy – C) Prednisone – D) Pulmonary rehabilitation MKSAP Answer 3 • • • • Pulmonary rehabilitation is the most appropriate management for this patient. Current guidelines recommend pulmonary rehabilitation for symptomatic patients with an FEV1 less than 50% of predicted. Pulmonary rehabilitation may be considered for symptomatic or exerciselimited patients with an FEV1 greater than or equal to 50% of predicted, but this is a weaker recommendation based upon moderate-quality evidence. Exercise training improves skeletal muscle function and reduces dynamic hyperinflation. Benefits of pulmonary rehabilitation include improvement in exercise capacity, reduction in the perceived intensity of breathlessness, improvement in health-related quality of life, and reduction in anxiety and depression associated with COPD. It is not recommended for patients who cannot walk or who have unstable angina or recent myocardial infarction. Morphine can be used in palliation for patients with severe dyspnea, especially at rest. However, this patient's dyspnea is not severe, so morphine is not appropriate at this time. This patient's oxygenation is adequate, and supplemental oxygen is not required. Oxygen therapy is indicated for patients who have hypoxemia, arterial PO2 of 55 mm Hg (7.3 kPa) or lower, or oxygen saturation of 88% or lower. This patient has no indication for a short-term course of a systemic corticosteroid because she does not have evidence of an acute exacerbation. An exacerbation of COPD is defined as an acute event characterized by a change in baseline dyspnea, cough, and/or sputum production beyond normal daily variation. The main symptoms include increased dyspnea often accompanied by wheezing and chest tightness, increased cough and sputum production, change in the color and/or tenacity of sputum, and fever. Various nonspecific signs and symptoms such as fatigue, insomnia, depression, and confusion may accompany these findings. MKSAP Question 4 • A 56-year-old man is evaluated in follow-up for COPD, which was diagnosed last week with spirometry; his FEV1 is 58% of predicted. He has a morning cough productive of sputum and dyspnea with moderate exertion. He quit smoking at the time of diagnosis. His only medication is a nicotine patch. He is started on a short-acting bronchodilator and is given appropriate vaccinations. • On physical examination, vital signs are normal. The lungs are clear to auscultation, but prolonged expiration is noted. The remainder of the physical examination is normal. MKSAP Question 4 • Which of the following is the most appropriate management? – A) Budesonide inhaler – B) Oral montelukast – C) Oral prednisone – D) Tiotropium inhaler MKSAP Question 4 • Which of the following is the most appropriate management? – A) Budesonide inhaler – B) Oral montelukast – C) Oral prednisone – D) Tiotropium inhaler MKSAP Answer 4 • • • • The most appropriate management is to begin a long-acting bronchodilator such as tiotropium. The 2011 American College of Physicians, American Thoracic Society, and European Respiratory Society guideline on the diagnosis and management of stable COPD recommends that for stable patients with symptomatic COPD and an FEV1 of less than 60% of predicted, the treatment is an inhaled bronchodilator (strong recommendation, moderate-quality evidence). Further, the guideline recommends that clinicians prescribe monotherapy using either long-acting inhaled anticholinergics or long-acting inhaled β2-agonists for symptomatic patients with COPD and FEV1 less than 60% of predicted (strong recommendation, moderate-quality evidence). There is no evidence that one is superior to the other. Clinicians should base the choice of specific monotherapy on physician or patient preference, cost, and adverse effect profile. For patients with stable COPD with respiratory symptoms and FEV1between 60% and 80% of predicted, the guideline suggests that treatment with inhaled bronchodilators may be used (weak recommendation, low-quality evidence). The guideline suggests that clinicians may administer combination inhaled therapies (long-acting inhaled anticholinergics, long-acting inhaled β2-agonists, or inhaled corticosteroids) for symptomatic patients with stable COPD and FEV1 of less than 60% of predicted (weak recommendation, moderate-quality evidence). An inhaled corticosteroid such as budesonide as monotherapy is not recommended owing to its lack of clinical benefit compared with an inhaled bronchodilator. Leukotriene modifiers such as montelukast have not been adequately tested in patients with COPD and are not recommended. A short course of systemic corticosteroids is used in patients with an acute COPD exacerbation, but long-term use of systemic corticosteroids is not recommended owing to adverse effects. MKSAP Question 5 • • • A 62-year-old man is evaluated during a routine examination. He has very severe COPD and has had multiple recent exacerbations and several hospitalizations over the past 2 years. During his last two hospitalizations he had acute hypercapnia requiring intubation. He has completed pulmonary rehabilitation twice, most recently 3 months ago, and his exercise capacity remains poor. He is adherent to his medication regimen. He used to smoke two packs per day but now only smokes two or three cigarettes per day. He is on 2 L of oxygen. His current medications are a fluticasone inhaler, salmeterol, tiotropium, roflumilast, and albuterol as needed. On physical examination, temperature is 37.1 °C (98.8 °F), blood pressure is 130/85 mm Hg, pulse rate is 88/min and regular, and respiration rate is 22/min. Pulmonary examination discloses distant breath sounds without wheezing. Oxygen saturation is 92% on 2 L of oxygen. Pulmonary function testing discloses an FEV1 of 18% of predicted, an FEV1/FVC ratio of 38%, and a DLCO of 15% of predicted. Chest radiograph shows a flattened diaphragm and decreased lung markings. MKSAP Question 5 • Which of the following is the most appropriate next step in management? – A) Increase oxygen – B) Lung transplantation evaluation – C) Lung volume reduction surgery evaluation – D) Repeat pulmonary rehabilitation – E) Smoking cessation MKSAP Question 5 • Which of the following is the most appropriate next step in management? – A) Increase oxygen – B) Lung transplantation evaluation – C) Lung volume reduction surgery evaluation – D) Repeat pulmonary rehabilitation – E) Smoking cessation MKSAP Answer 5 • • • • The most appropriate next step in management is to advise this patient to quit smoking. He meets criteria for possible lung transplantation based on the severity of his COPD. However, substance addiction (alcohol, tobacco, or narcotics) that is current or active within the last 6 months is an absolute contraindication to lung transplantation. This patient is still smoking and therefore should be advised to quit. Transplantation in patients with COPD should be considered if deterioration continues despite appropriate, maximal medical therapy in patients without clear contraindications to the procedure. The BODE (BMI, Obstruction, Dyspnea, Exercise) index is a method for assessing severity of COPD and is based on health care quality-of-life measures and independent predictors of disease-related mortality. A BODE score of greater than 5 is an indication for referral for evaluation for lung transplantation. Transplantation is indicated in patients with a BODE index of 7 to 10 and at least one of the following: history of hospitalization for exacerbation associated with hypercapnia; pulmonary hypertension, cor pulmonale, or both despite oxygen therapy; FEV1 of less than 20% of predicted and either DLCO of less than 20% of predicted or homogeneous distribution of emphysema. Referral for lung transplantation would be appropriate for this patient only if he stops smoking. This patient's oxygenation is adequate; therefore, increasing the oxygen is not appropriate, especially in a patient with a history of acute hypercapnia. Oxygen therapy is indicated for patients who have hypoxemia, arterial PO2 less than 55 mm Hg (7.3 kPa), or arterial oxygen saturation of 88% or lower. Patients with an FEV1 of less than 20% of predicted and either a DLCO of less than 20% of predicted or homogeneously distributed emphysema are considered high risk for lung volume reduction surgery (LVRS). Because this patient's FEV1 and DLCO are less than 20% of predicted, this patient is not an ideal candidate for LVRS. Pulmonary rehabilitation is very effective in patients with advanced COPD, and repeated courses or continuous pulmonary rehabilitation has value. However, it is not a definitive treatment for patients with severe disease who would otherwise be eligible for lung transplantation. References • Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: Revised 2015. Global Initiative for Chronic Obstructive Lung Disease (GOLD). www.goldcopd.org (Accessed on September 21, 2015). • Qaseem A, Snow V, Shekelle P, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2007; 147:633 • UpToDate