Acute Decompensated Heart Failure (ADHF)- Inpatient Management Jennifer Kumar February 2014
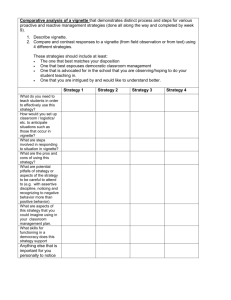
advertisement

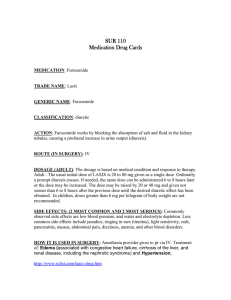
Acute Decompensated Heart Failure (ADHF)- Inpatient Management Jennifer Kumar February 2014 Objectives Learn to identify the signs and symptoms of ADHF Learn to interpret pertinent laboratory data and imaging Learn the inpatient management of ADHF Clinical Vignette Clinical Vignette 62 year old Caucasian male with PMH of ischemic cardiomyopathy (EF 25%), CAD, HTN presents with two week history of dyspnea Previously able to walk 2 miles, currently cannot walk more than 10 feet before developing DOE PND 3 times per night 4 pillow orthopnea Increasing lower extremity edema ROS: loss of energy, loss of appetite, 10# weight gain Clinical Vignette PMH: ischemic cardiomyopathy (EF 25%, based on echocardiogram 6 months prior), CAD (s/p MI with PCI in 2002), HTN Home medications: ASA 81mg daily, Lisinopril 5mg daily, Lasix 40mg daily Allergies: NKDA ROS: denies CP, denies dizziness, denies palpitations Clinical Vignette VS: Temp 36.5, HR 90, BP 108/72, RR 20, SpaO2 91% on RA Pertinent physical exam: ◦ General: appears uncomfortable, able to speak short sentences ◦ HEENT: Jugular venous distension at 10cm ◦ CVS: PMI displaced laterally to mid-axillary line in the 6th ICS, (-) heaves, thrills, RRR, (+) S3, (-)S4, (-) murmurs or rubs ◦ Chest: loss of tactile fremitus at the base with dullness to percussion, (+) rales throughout bottom half of lung fields bilaterally ◦ Abdomen: distended, (+) mild fluid wave, (+) hepatojugular reflux, ◦ Extremities: 2+ pitting edema up to knees bilaterally, cool to touch, 2+ DP and PT pulses Clinical Vignette Current presentation consistent with acute decompensated heart failure (ADHF) What labs should we order to help evaluate further? Laboratory Data CBC ◦ Anemia, infection can precipitate ADHF BMP ◦ Hyponatremia- poor prognostic sign ◦ Elevated creatinine- impaired renal perfusion LFT ◦ May be elevated due to congestive hepatopathy Troponin ◦ Ischemia can precipitate HF ◦ Troponin may be mildly elevated in HF as well from demand ischemia Laboratory Data BNP ◦ < 100 strongly suggestive against HF ◦ >400 suggestive of HF exacerbation However may be falsely elevated in: Renal disease, atrial fibrillation, pulmonary HTN May be falsely low in: Obese patients, HFPEF Toxicology screen ◦ In select patients, as drug abuse can trigger exacerbation TSH ◦ Untreated thyroid disease can precipitate exacerbation Clinical Vignette At this point, what imaging should be obtained to further assist with management? Imaging: EKG Important to look for underlying ◦ Ischemia ◦ Arrhythmias Imaging: Chest x-ray Enlarged cardiac silhouette Pulmonary edema Pulmonary congestion ◦ Cephalization ◦ Kerley B lines ◦ Peri-bronchial cuffing Pleural effusions, typically bilateral Clinical Vignette Should an echocardiogram be repeated? Imaging: Echo Typically repeated no sooner than annually Provides information regarding; ◦ ◦ ◦ ◦ ◦ ◦ Ejection fraction Diastolic dysfunction Wall motion abnormalities Chamber sizes Pulmonary HTN Ventricular dysynchrony Clinical Vignette How should we begin our inpatient management? Non-pharmacologic Management Daily weight Strict I’s and O’s Low sodium diet (<2g daily) Fluid restriction ◦ Typically only for patients with hyponatremia Clinical Vignette What should we use to improve our patient’s volume status? Treatment: Diuretics Recommend to give intravenously initially Typically at least twice a day Agents ◦ Furosemide Can give home dose as IV (2:1 po to IV ratio) Titrate up based on response (goal net negative 1.52L daily on average) ◦ Bumetanide Alternative to Furosemide in tolerant patients 40 mg IV Lasix = 1 mg IV Bumetanide = 1mg po Bumetanide Clinical Vignette The patient is now receiving 40mg Furosemide IV twice a day What could be done next if the patient did not respond to Furosemide? How often should his electrolytes be monitored? Treatment: Diuretics If not responding to initial diuretic dose: ◦ Can titrate dose up further ◦ Older patients, underlying renal dysfunction may require higher doses Can consider adding Metolazone for additional effect ◦ Thiazide diuretic Monitoring of electrolytes closely ◦ Check potassium and magnesium at least daily ◦ If aggressive diuresis, check at least twice daily Clinical Vignette The patient did not come in on a beta blocker, but this has been shown to improve long-term mortality in heart failure Should we begin a beta blocker at this time? Which beta blocker (if any) should we choose? Treatment: Beta blockers Typically not initiated during acute exacerbation Continue if already on ◦ Stopping can worsen RAAS activation ◦ If SYMPTOMATIC hypotension, can decrease the dose Options ◦ Carvedilol: lowest dose 3.125mg BID ◦ Metoprolol XL: lowest dose 25mg daily ◦ Titrate to goal HR of 60 bpm Or as much as BP can tolerate Caveat: Blood pressure Patients with heart failure frequently have a lower BP than the general population ◦ Due to reduced cardiac output Not unusual to see patient’s with reduced EF to have a SBP in the 80s-100s Use of medications which can lower BP is not contraindicated in these populations ◦ However, need to ensure patient does not have lightheadedness, orthostatic hypotension Clinical Vignette The patient has been having an appropriate diuresis Clinically, patient reports improvement in shortness of breath and now able to walk without DOE PE: resolution of rales, peripheral edema How should the diuretic dose be adjusted? What medications should be added to his regimen prior to discharge? Medication Adjustment Diuretic ◦ Patient should be transitioned to po regimen ◦ Can base the po on the dose of the IV dose E.g. Furosemide 40mg IV BID 40mg po BID ◦ Should monitor for at least 24 hours on po to ensure proper response Chronic medical management ACEI/ARB ◦ Shown to improve mortality ◦ Already on Lisinopril, can titrate up further as tolerated ◦ Consider decreasing dose or discontinuing if: SYMPTOMATIC hypotension, AKI, hyperkalemia Spironolactone ◦ Shown to improve mortality (RALES trial) ◦ Indications: EF <30% and NYHA Class II OR EF <35% and NYHA Class III/IV ◦ Benefits: enhances diuresis, minimizes K wasting ◦ Dosing: lowest: 12.5mg, titrate up as tolerated Digoxin ◦ Reduces rate of hospital admissions ◦ No significant effect on mortality no longer used as frequently now Clinical Vignette Which patients benefit from combination therapy with Isosorbide dinitrate/Hydralazine? Treatment: Isosorbide dinitrate/Hydralazine ◦ Added to standard therapy for heart failure ◦ Efficacious and increases survival among black patients with heart failure ◦ Dosing: Isosorbide dinitrate/Hydralazine 20mg/37.5mg TID Transition to Outpatient Our patient’s discharge meds Furosemide 40mg BID Lisinopril 5mg daily Carvedilol 3.125mg BID Spironolactone 12.5mg daily ASA 81mg daily Summary Identify clinical signs and symptoms of ADHF Pertinent labs ◦ Sodium, creatinine, troponin, BNP Relevant imaging ◦ EKG, CXR, echocardiography Treatment ◦ Diuresis, BB, ACEI/ARB, Spironolactone, Digoxin, Isosorbide dinitrate/Hydralazine Transition to outpatient ◦ Strict instructions, close-follow-up