THE USE OF CARDIAC MONITORING FOR NON-ICU MEDICINE PATIENTS AT Jerry Yu
advertisement

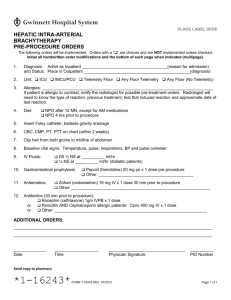
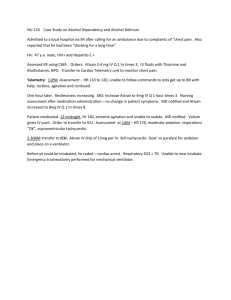
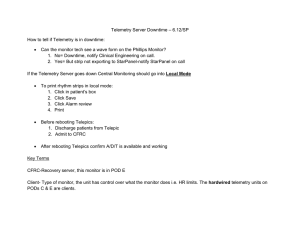
THE USE OF CARDIAC MONITORING FOR NON-ICU MEDICINE PATIENTS AT UCI: A FOLLOW UP Jerry Yu DSR2 Cardiac Monitoring • Introduced >40 years ago to the inpatient setting • Now include computerized arrhythmia detection, ST segment monitoring, noise reduction, multi-lead monitoring The drawbacks of telemetry • Deliberately set for high sensitivity at the expense of • • • • specificity (frequent arrhythmia alarms, ST segment alarms) Consequently telemetry can give false-positive alarms: misinterpretation of artifacts as arrhythmia Telemetry is expensive: 1998 study estimates cost at $683 per patient per day When and how telemetry should be used has been a matter of debate Known shortage of telemetry beds available at UCI can often impede transfer of patients from higher levels of care 2004 AHA Guidelines for Cardiac Monitoring • Separation of patients into 3 risk classes: • Class I: Telemetry indicated for nearly all patients • Class II: Telemetry MAY be indicated in some patients • Class III: Telemetry is NOT indicated • Guidelines are based on expert opinion consensus Class I Indications • • • • • • • • • • • • • • • Patients resuscitated from cardiac arrest Patients in early ACS Patients with ACS and newly diagnosed high-risk coronary lesions Adults who undergone cardiac surgery Child who undergone cardiac surgery Patients who undergone non-urgent PCI w/ complications Patients undergone DF or PM placement and are pacer dependent Patients with temporary pacemaker Patients with AV block (mobitz 2 or higher) Patients with arrhythmias complicating WPW with rapid conduction Patients with long QT syndrome and associated ventricular arrhythmia Patients receiving Intraaortic balloon counterpulsation Patients with Acute heart failure/pulmonary edema Patients with hemodynamically unstable arrhythmia Patients with indications for intensive care • • • • • • • Sepsis Acute Respiratory Failure Shock Acute PE Major non-cardiac surgery Renal failure with electrolyte abnormalities Drug overdose (esp with known arrhythmogenics) Class II Indications • Patients with postacute MI • Patients with chest pain syndromes • Patients undergone uncomplicated non urgent PCI • Patients with chronic atrial tachyarrhythmias receiving antiarrhythmic rx • Patients undergone PM who are not PM dependent • Patients who undergone uncomplicated ablation of arrhythmia • Patients who undergone routine coronary angiography • Patients with subacute heart failure • Patients who are being evaluated for syncope • Patients who are DNR with arrhythmias that causediscomfort Class III indications • Postoperative patients at low risk for arrhythmias • Obstetric patients unless heat disease is present • Patients with permanent rate controlled atrial fibrillation • Patients undergoing hemodialysis w/o Class I/II indications • Stable patients with chronic ventricular premature beats Some Background literature • Estrada CA, Young MJ. Role of Telemetry monitoring in the non-intensive care unit. Am J Cardiol. 1995 Nov 1;76(12):960-5 • Prospective Cohort study n=2240 • Telemetry lead to change in management of 7% of patients • Telemetry was useful but did not change management in 5.7% of patients • Estrada CA, Young MJ. Evaluation of Guidelines for the Use of Telemetry in the Non-Intensive-care setting. J Gen Intern Med. 2000 January; 15(1): 51– 55. • Subgroup analysis based on previous study • Telemetry detected arrhythmia resulting in ICU transfer for: • 0.4% of the Class I patients • 1.6% of the Class II patients • 0% of the Class III patients The Prior Project- 2012 • Conducted at UCI inpatient medicine service- 4 ward teams • Classified patients on telemetry into class I, II, or III based on 2004 AHA guidelines • Determined % of patients who received telemetry w/o class I or II indications Results of 2012 study • 54 patient charts were reviewed • 39% of patients were found to not have class I or II indications for telemetry • Most common reasons to be on telemetry: • Stable GI bleeding • Chest pain r/o • Respiratory compromise • Acute decompensated Heart failure Current UCIMC non-ICU telemetry capacity • T5: 28 beds • T3: 28 beds • DH 78: 15 beds • DH 66: 15 beds • DH 68: 15 beds • Non-telemetry beds: • T4: 25 • DH 32: 15 • “On any given day, all telemetry beds are full and we have patients waiting for telemetry beds” -SPPO This Project • Review of 6 ward Teams at UCI • Review of all patients on cardiac monitoring on a telemetry unit (T3, T5, DH78, NSDU, SDU) • Classify patients into Class I, II, or III indications for cardiac monitoring based on 2004 AHA guidelines • Compare current % of Class III patients to 2012 Results • Total 53 patient’s charts were reviewed • Most common indications for cardiac monitoring • 1. Syncope • 2. A fib/A flutter w/ RVR • 3. Sepsis with hypotension • 4. Acute Decompensated Heart Failure Results Team # of pts on tele unit # of patients w/ cardiac monitor # of Class I # of Class II # of class III % of patients on tele w/ class III A 8 7 3 2 1 14% B 6 4 1 2 1 25% C 5 5 2 2 1 20% D 13 12 6 1 5 42% E 8 7 2 2 3 42% G 13 10 9 1 0 0% Total 53 45 23 10 11 24.4% Results • 24.4% of patients on cardiac monitoring did not have indications • Most commonly observed: Hemodynamically stable patients with infections (UTI, CAP, infectious colitis) • Compared to 2012, observed a 14.6% reduction in non- indicated cardiac monitoring use Limitations • Small sample size • Bias (me) in applying AHA guidelines and categorization • No AHA category for “clinical judgement” Discussion • We observed a substantial improvement over telemetry use from 2 years prior of 14.6% • Yet, still have nearly 1/4th of all telemetry use not fulfilling AHA criteria • This is an understatement given that not ALL class II patients require telemetry use Areas for improvements at UCI • Continued daily examination of telemetry use during morning rounds with RN staff • Early cessation of cardiac monitoring when indications are no longer met • Continued need to educate house staff and attending alike regarding AHA recommendations