Not Wanting to Miss a Beat – Is it Costing Us?
advertisement

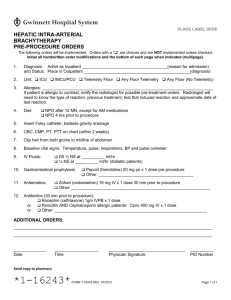
Not Wanting to Miss a Beat – Is it Costing Us? Analysis of Appropriate Use of Cardiac Monitoring for ICU transfers Kimberly Truong | Feb 2016, Doctoring Skill Rotation 2 Acknowledgements: Michelle Le, Jerry Yu, Asad Qasim Cardiac Monitoring • Introduced >40 years ago to the inpatient setting • Allows remote monitoring of cardiac rhythm and pulse ox • Logistically, determines which floor pt can be transferred to and nursing ratio 2 The drawbacks • Telemetry is expensive: 1998 study estimates cost at $683 per patient per day (bill of $9,108 /day in 2012 at UCI • Deliberately set for high sensitivity at the expense of specificity • Consequently telemetry can give false-positive alarms: misinterpretation of artifacts as arrhythmia • When and how telemetry should be used has been a matter of debate. Some physicians not aware of indications. • Known shortage of telemetry beds available at UCI can often impede transfer of patients 3 Guidelines 4 2004 AHA Guidelines for Cardiac Monitoring Class I: Telemetry indicated for nearly all patients Class II: Telemetry MAY be indicated in some patients Class III: Telemetry is NOT indicated 5 6 7 8 Current UCIMC non-ICU telemetry capacity T5: 28 beds T3: 28 beds DH 78: 15 beds DH 66: 15 beds DH 68: 15 beds Total = 101 telemetry beds Non-telemetry beds: T4: 25 9 Most Recent Project – Analyzed Medicine Admissions 6 UCI ward teams 42 patient’s charts were reviewed 27% of patients were found to not have class I or II indications for telemetry (similar to year before) Improvement from 2012, when 39% of patients were found to not have class I or II indications for telemetry Most common indications for cardiac monitoring 1. Sepsis with risk for hypotension 2. Syncope 3. ACS rule out 4. EtOH withdrawal 10 This Project -- Methods • Looked at ICU transfers • Medicine residents have more control • Chart reviewed ICU transfers for 7 days • Level of care documented – Med Surg vs Telemetry • Indication for telemetry documented, then classified as Class I, II or III indications based on AHA Guidelines • Class I is definitely indicated • Class II means may be indicated • Class III means definitely NOT indicated • Summary statistical analysis used 11 Results – Summary Table Overall Diagnosis COPD/asthma exacerbation Upper GI Bleed Pneumonia DKA Chronic afib, rate controlled New onset afib Recent severe sepsis or septic shock First degree AV block History of CAD Tracheal stenosis Obstructive sleep apnea Prostate cancer Decompensated congestive heart failure Acute ischemic cardiac disease Total 12 N % 6 4 3 3 3 2 2 1 1 1 1 1 1 1 30 20.0% 13.3% 10.0% 10.0% 10.0% 6.7% 6.7% 3.3% 3.3% 3.3% 3.3% 3.3% 3.3% 3.3% 100% Results – Summary Table Overall Transfers N % Med Surg 7 23.3% Telemetry 23 76.7% Total 30 13 Department Name | Month X, 201X Med Surg Transfers: Summary Table N % DKA 3 42.9% Upper GI Bleed 1 14.3% Chronic atrial fibrillation 1 14.3% Pneumonia 1 14.3% Prostate cancer 1 14.3% Total 7 14 Department Name | Month X, 201X Telemetry Transfers: Summary Table N 15 Indication Class % COPD/Asthma exacerbation Upper GI Bleed Pneumonia New onset afib 6 3 2 2 26.1% 13.0% 8.7% 8.7% 2 3 2 2 Chronic afib, rate controlled Severe sepsis, septic shock 2 8.7% 8.7% 3 Tracheal stenosis 2 1 4.3% 2 2 Sleep apnea first degree AV block 1 1 4.3% 4.3% 3 3 Acute decompensated heart failure 1 4.3% 1 1 1 23 4.3% 4.3% 1 3 Acute ischemic heart disease History of CAD Total Telemetry Transfers, by Indication Class Indication Class N % 1 2 8.7% 2 13 56.5% 3 8 34.8% 23 16 Department Name | Month X, 201X Cost Analysis Estimated excess cost to hospital for telemetry use and nursing: • • • $53/day1 With our 8 patients that had non-indicated monitoring excess of $424 for 7 days If we continue this for a year $22,048 per year Estimated cost to patient for telemetry bed (2012): • General Med/Surg Bed: $5,359 /day • Monitored (Tele) Bed: $9,108 /day – Excess Cost per day: $3,750 / day – With our 8 patients that had non-indicated cardiac monitoring excess of $30,000 in 7 day – If we continue this for 365 days $1.6 million in 1 year 17 Department Name | Month X, 201X Limitations Small sample size. Only a 7-day cross-section look at teams’ census. May be resident and attending dependent Subjective assessment (classification bias) in applying AHA guidelines and categorization of indications or lack of indication 18 Department Name | Month X, 201X Conclusion • First study to look at telemetry orders where internal medicine residents have responsibility over • Rate of inappropriate telemetry use may be higher than medicine admission telemetry use (35% vs 27%) • There is room for housestaff education and possible technology integration (ie: pop-up or order expiration) in Quest 19 Department Name | Month X, 201X References 1) Benjamin EM, Klugman RA, Luckmann R, Fairchild DG, Abookire SA. Impact of Cardiac Telemetry on Patient Safety and Cost. AJMC 2013;19(6):e225-32 20 Department Name | Month X, 201X