20 Vitamin D and Calcium T.S. Dharmarajan and Amit Sohagia Questions and Answers
advertisement
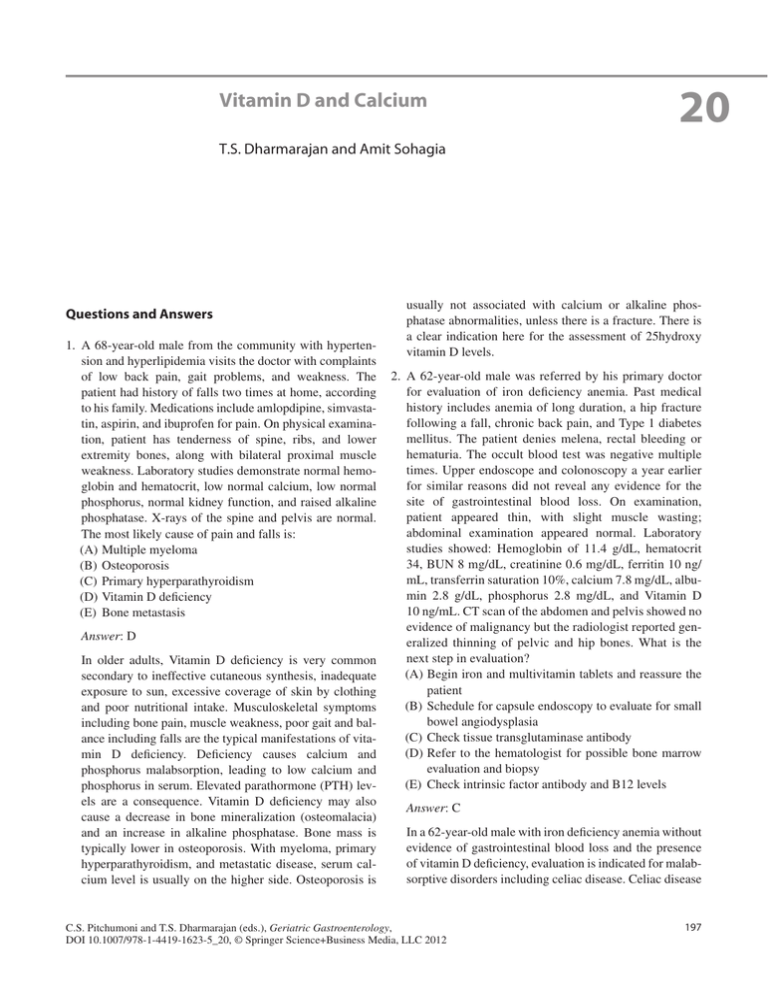
Vitamin D and Calcium 20 T.S. Dharmarajan and Amit Sohagia Questions and Answers 1. A 68-year-old male from the community with hypertension and hyperlipidemia visits the doctor with complaints of low back pain, gait problems, and weakness. The patient had history of falls two times at home, according to his family. Medications include amlopdipine, simvastatin, aspirin, and ibuprofen for pain. On physical examination, patient has tenderness of spine, ribs, and lower extremity bones, along with bilateral proximal muscle weakness. Laboratory studies demonstrate normal hemoglobin and hematocrit, low normal calcium, low normal phosphorus, normal kidney function, and raised alkaline phosphatase. X-rays of the spine and pelvis are normal. The most likely cause of pain and falls is: (A)Multiple myeloma (B) Osteoporosis (C) Primary hyperparathyroidism (D)Vitamin D deficiency (E) Bone metastasis Answer: D In older adults, Vitamin D deficiency is very common secondary to ineffective cutaneous synthesis, inadequate exposure to sun, excessive coverage of skin by clothing and poor nutritional intake. Musculoskeletal symptoms including bone pain, muscle weakness, poor gait and balance including falls are the typical manifestations of vitamin D deficiency. Deficiency causes calcium and phosphorus malabsorption, leading to low calcium and phosphorus in serum. Elevated parathormone (PTH) levels are a consequence. Vitamin D deficiency may also cause a decrease in bone mineralization (osteomalacia) and an increase in alkaline phosphatase. Bone mass is typically lower in osteoporosis. With myeloma, primary hyperparathyroidism, and metastatic disease, serum calcium level is usually on the higher side. Osteoporosis is usually not associated with calcium or alkaline phosphatase abnormalities, unless there is a fracture. There is a clear indication here for the assessment of 25hydroxy vitamin D levels. 2. A 62-year-old male was referred by his primary doctor for evaluation of iron deficiency anemia. Past medical history includes anemia of long duration, a hip fracture following a fall, chronic back pain, and Type 1 diabetes mellitus. The patient denies melena, rectal bleeding or hematuria. The occult blood test was negative multiple times. Upper endoscope and colonoscopy a year earlier for similar reasons did not reveal any evidence for the site of gastrointestinal blood loss. On examination, patient appeared thin, with slight muscle wasting; abdominal examination appeared normal. Laboratory studies showed: Hemoglobin of 11.4 g/dL, hematocrit 34, BUN 8 mg/dL, creatinine 0.6 mg/dL, ferritin 10 ng/ mL, transferrin saturation 10%, calcium 7.8 mg/dL, albumin 2.8 g/dL, phosphorus 2.8 mg/dL, and Vitamin D 10 ng/mL. CT scan of the abdomen and pelvis showed no evidence of malignancy but the radiologist reported generalized thinning of pelvic and hip bones. What is the next step in evaluation? (A)Begin iron and multivitamin tablets and reassure the patient (B) Schedule for capsule endoscopy to evaluate for small bowel angiodysplasia (C) Check tissue transglutaminase antibody (D)Refer to the hematologist for possible bone marrow evaluation and biopsy (E) Check intrinsic factor antibody and B12 levels Answer: C In a 62-year-old male with iron deficiency anemia without evidence of gastrointestinal blood loss and the presence of vitamin D deficiency, evaluation is indicated for malabsorptive disorders including celiac disease. Celiac disease C.S. Pitchumoni and T.S. Dharmarajan (eds.), Geriatric Gastroenterology, DOI 10.1007/978-1-4419-1623-5_20, © Springer Science+Business Media, LLC 2012 197 198 is a small bowel disorder characterized by mucosal inflammation, villous atrophy, and crypt hyperplasia, occurring upon exposure to dietary gluten; there is demonstrable improvement after withdrawal of gluten from the diet. The classic form is characterized by fully developed villous atrophy and features of intestinal malabsorption. The atypical form is characterized by villous atrophy in the setting of milder clinical features such as iron deficiency, osteoporosis, short stature, and/or infertility. Despite the historical title of “atypical,” this form is the most common. Option A is inappropriate as iron deficiency anemia always warrants evaluation for gastrointestinal blood loss and malignancy. Option B is not appropriate at this time as multiple stool specimens are negative for occult blood, although capsule endoscopy can pick up scalloping and villous atrophy of celiac disease. While bone marrow can provide an idea of iron stores, it would not provide an etiology for iron deficiency; B12 deficiency could be present in celiac disease but would not explain the laboratory abnormalities described. 3. All of following foods are natural sources of vitamin D except: (A)Sea foods, such as salmon, tuna fish, mackerel (B) Cod liver oil (C) Dry mushrooms (shiitake) (D)Egg yolk (E) Dairy products: milk, yogurt, cheese Answer: E Only few foods contain vitamin D. Fatty fishes (such as salmon, tuna, and mackerel) and cod liver oils are among the best sources. Small amounts of vitamin D are found in beef liver, cheese, and egg yolk. Vitamin D in these foods is primarily in the form of vitamin D3 and its metabolite 25(OH)D3. Some mushrooms provide vitamin D2, with shiitake mushrooms being a very good source. Dairy products such as milk, cheese, and yogurt contain calcium but do not contain vitamin D in the natural state, unless they are fortified. Fortified foods provide most of the vitamin D in the American diet. Fortification is not applied to every yogurt and cheese, and so labels have to be carefully scrutinized. Almost all of the US milk supply is fortified with 100 IU/8 oz, as also some brands of almond milk, soy milk, orange juice, and cereals. 4. Which of the following factors most interferes with calcium absorption in the small intestine? (A)Age (B) Calcium intake with meals (C) Sodium and protein intake (D)Components in food such as phytic acid and oxalic acid (E) Amount of calcium consumed T.S. Dharmarajan and A. Sohagia Answer: C High intakes of sodium, protein, and even caffeine increase calcium excretion but do not interfere with absorption of calcium in the gut. Factors which are responsible for calcium absorption in the gastrointestinal tract are: amount of calcium consumed (the efficiency of absorption decreases as calcium intake increases), age and life stage (absorption decreases to 15–20% in adulthood and continues to decrease as people age; compared with younger adults, recommended calcium intakes are higher for females older than 50 years and for both males and females older than 70 years), vitamin D intake and status, and components in food (phytic acid and oxalic acid, found naturally in some plants, which bind to calcium and inhibit absorption). Vegetarians might absorb less calcium than omnivores because they consume more plant products containing oxalic and phytic acids. On the other hand, some vegetarian diets may contain less protein than typical omnivore diets, which may help reduce calcium excretion. While calcium carbonate is better absorbed in the presence of acid and with meals, calcium citrate has reasonable absorption even in the empty stomach or with lower gastric acidity.. 5. A 62-year-old patient with history of Crohn’s disease diagnosed in early adulthood complicated with strictures and fistulae underwent multiple small bowel surgical procedures and had resection of more than 100 cm of ileum. He now presents with right-sided flank pain and hematuria. Currently the patient is taking 6-mercaptopurine, with the Crohn’s disease in remission. The CT scan confirms obstructing right renal calculi. The patient underwent lithotripsy by urologist and now comes to you for dietary advice to prevent recurrent stones. Which of the following supplements will most likely lessen his chance of recurrent stone formation? (A)Zinc (B) Calcium (C) Magnesium (D)Potassium Answer: B Calcium oxalate stones are common in patients with Crohn’s disease who have had ileal resection. More than 100 cm ileal resection may lead to steatorrhea from bile salt malabsorption. Fat malabsorption tends to increase oxalate absorption in colon via two mechanisms. (1) Unabsorbed fatty acids bind calcium leading to a reduction in the formation of insoluble calcium oxalate, which leaves more oxalate free in the solution for absorption. (2) Fatty acids and bile salts increase colonic permeability to oxalate. A reduced fat diet and calcium supplementation are recommended to diminish oxalate absorption 20 Vitamin D and Calcium and prevent hyperoxaluria and nephrolithiasis. Calcium supplements will bind oxalate in the gut, reducing the amount of free oxalate available for absorption. 6. Which of the following statements is most accurate regarding vitamin D? (A)1,25 Dihydroxy vitamin D formed in the kidney is the physiologically active form and a reliable measure of status. (B) 25 Hydroxy vitamin D is the storage form, but a poor measure of the vitamin status. (C) Vitamin D provided in doses of 800 IU daily is safe and the current recommendation. (D)Vitamin D is best provided as 500,000 U annually or 50,000 U weekly for 3 months, as compliance improves with this form of administration. 199 Answer: C Vitamin D as the 25 hydroxy form is the storage form and the best index of status at the present. While the 1,25 form is physiologically active, it has a short half life and is labile, with levels poorly suggestive of the status. Current guidelines from the Institute of Medicine (IOM) recommend 800 IU daily for adults over age 70 and state that the upper safe limit is 4,000 U/day. Canadian guidelines recommend a range from 800 to 2,000 U daily. Large intermittent doses of 500,000 U have been shown to be associated with falls and fractures. It is likely that large intermittent doses are metabolized differently from smaller frequent doses.