Psychosocial Outcomes and Health-Related Quality of
advertisement

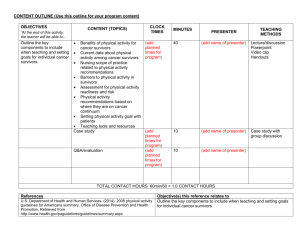
435 Psychosocial Outcomes and Health-Related Quality of Life in Adult Childhood Cancer Survivors: A Report from the Childhood Cancer Survivor Study Lonnie K. Zeltzer,1 Qian Lu,1 Wendy Leisenring,3 Jennie C.I. Tsao,1 Christopher Recklitis,4 Gregory Armstrong,2 Ann C. Mertens,5 Leslie L. Robison,2 and Kirsten K. Ness2 Department of Pediatrics and Division of Cancer Prevention and Control Research, David Geffen School of Medicine at University of California at Los Angeles and University of California at Los Angeles’s Jonsson Comprehensive Cancer Center, Los Angeles, California; 2Department of Epidemiology and Cancer Control, St. Jude Children’s Research Hospital, Memphis, Tennessee; 3Fred Hutchinson Cancer Research Center, Seattle, Washington; 4Dana-Farber Cancer Institute, Boston, Massachusetts; and 5Department of Pediatrics, Emory University, Atlanta, Georgia 1 Abstract Purpose: Psychological outcomes, health-related quality of life (HRQOL), and life satisfaction are compared between 7,147 adult childhood cancer survivors and 388 siblings from the Childhood Cancer Survivor Study, examining demographic and diagnosis/treatment outcome predictors. Methods: Psychological distress, HRQOL, and life satisfaction were measured by the Brief Symptom Inventory-18, the Medical Outcomes Survey Short Form-36, and Cantril Ladder of Life, respectively. A self-report questionnaire provided demographic/health information and medical record abstraction provided cancer/treatment data. Siblings’ and survivors’ scores were compared using generalized linear mixed models, and predictor effects of demographic and cancer/treatment variables were analyzed by multivariate logistic regression. Results: Although survivors report greater symptoms of global distress (mean, 49.17; SE, 0.12) than do siblings (mean, 46.64; SE, 0.51), scores remain below population norms, indicating that survivors and siblings remain psychologically healthy. Survivors scored worse than siblings on overall physical (51.30 F 0.10 versus 54.98 F 0.44; P < 0.001) but not emotional aspects of HRQOL, but effect sizes were small, other than in vitality. Most survivors reported present (mean, 7.3; SD, 0.02) and predicted future (mean, 8.6; SD, 0.02) life satisfaction. Risk factors for psychological distress and poor HRQOL were female gender, lower educational attainment, unmarried status, annual household income <$20,000, unemployment, lack of medical insurance, having a major medical condition, and treatment with cranial radiation. Conclusion: Compared with population norms, childhood cancer survivors and siblings report positive psychological health, good HRQOL, and life satisfaction. The findings identify targeted subgroups of survivors for intervention. (Cancer Epidemiol Biomarkers Prev 2008;17(2):435 – 46) Introduction Adulthood is now attainable for most children treated for cancer with 5-year survival rates at 80% (1). Increased survival may be accompanied by long-term burden for some individuals related to the unique characteristics of their cancer diagnoses and treatment and the effect of treatment on their educational, psychological, and social development. Identification of subgroups of childhood cancer survivors at risk for poor health-related quality of Received 9/8/07; revised 11/1/07; accepted 11/30/07. Grant support: National Cancer Institute grant U24-CA55727 (L.L. Robison, Principal Investigator), American Lebanese Syrian Associated Charities (St. Jude Children’s Research Hospital), Children’s Cancer Research Fund (University of Minnesota), University of California at Los Angeles’s Jonsson Comprehensive Cancer Center postdoctoral fellowship (Q. Lu), and Lance Armstrong Foundation grant G-00-12-076-02 (L. Zeltzer, Principal Investigator). The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact. Requests for reprints: Lonnie K. Zeltzer, Department of Pediatrics, David Geffen School of Medicine at University of California at Los Angeles, 22-464 MDCC, 10833 Le Conte Avenue, Los Angles, CA 90095-1752. Phone: 310-825-0731; Fax: 310-794-2104. E-mail: lzeltzer@mednet.ucla.edu Copyright D 2008 American Association for Cancer Research. doi:10.1158/1055-9965.EPI-07-2541 life (HRQOL) is important for development of intervention strategies. As treatments evolve, determination of treatments promoting long-term survival and reduced risk for poor HRQOL outcomes will be a goal. Findings in survivors are often derived from singleinstitution oncology programs or long-term follow-up clinics and suggest that psychosocial status and HRQOL are relatively good for most survivors, yet less favorable outcomes have been reported (2-6). Childhood Cancer Survivor Study (CCSS) reports have examined psychosocial outcomes and HRQOL within specific diagnostic groups (7-11). However, it is necessary to examine the entire cohort of childhood cancer survivors, compare them with siblings, and identify demographic and treatment risk factors so that risk-based treatments to enhance HRQOL of life can be developed. This report describes psychosocial status, HRQOL, and life satisfaction in the CCSS cohort, compares findings to sibling controls and population norms, and examines broad demographic and treatment factors associated with poor outcomes among survivors. We have used siblings as the major comparison group for survivors because the demographic match to the survivors is closer in the sibling group than in cohorts Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 436 Psychological Distress, HRQOL, and Life Satisfaction from which the population norms were derived (12). This article, by painting the big picture, will provide the background for future, more detailed, within-diagnosis analyses. Materials and Methods Participants. The CCSS cohort, a resource funded by the National Cancer Institute, represents the largest and most comprehensively characterized group of childhood cancer survivors in North America. Details of study design and cohort characteristics have been described elsewhere (13, 14). Subjects were recruited from persons treated for an initial diagnosis of leukemia, central nervous system (CNS) malignancy, Hodgkin’s disease, non – Hodgkin’s lymphoma (NHL), kidney cancer, neuroblastoma, soft tissue sarcoma, or malignant bone tumor at 1 of 26 institutions across the United States and Canada, survivors >5 years, and diagnosed between 1970 and 1986 when younger than 21 years of age. Among the 20,267 eligible individuals, 17,273 were located; 14,024 (81.2%) survivors and 3,846 siblings were enrolled. Comparison of participants, nonparticipants, and those who were lost to follow-up showed similar demographic, disease, and treatment characteristics (14, 15). Of eligible survivors and siblings 18 years of age or older at contact and available for the second follow-up survey, 9,307 (84%) survivors and 2,875 (80%) siblings participated. The psychosocial portion of this survey was sent to all survivors and a randomly selected subsample of 500 siblings, with 7,147 (77%) survivors and 388 (78%) siblings participating. The study was approved by Institutional Review Boards of all participating institutions with participants providing informed consent. Outcome Variables. Emotional health was evaluated by the 18-item Brief Symptom Inventory-18 (BSI-18), which includes symptoms over the previous 7 days. The BSI-18 has been validated in healthy volunteers (16), in cancer patients (17), and in an earlier administration with this cohort of cancer survivors (18). The BSI-18 has a summary scale (the global distress index) and three subscales (depression, anxiety, and somatization). Raw scores were converted to T-scores based on U.S. population norms and dichotomized using a cutpoint of 63. Those with T-scores z63 were classified as having poor emotional health (17, 18). The Medical Outcomes Short Form-36 (SF-36) was used to evaluate HRQOL. Participants answered 36 questions about general health, well-being, and quality of life over the previous 4 weeks. The SF-36 has two summary scales and eight individual subscales representing different aspects of well-being (19). Data are presented as T-scores, with a general population mean of 50 and SD of 10. Higher scores indicate ‘‘better’’ HRQOL (19). T-scores were dichotomized for the multiple variable models. Participants with T-scores at least 1 SD below the population mean (V40) were classified as reporting poor HRQOL. Life satisfaction was determined by having participants complete the Cantril Ladder of Life (LOL). The LOL assesses respondents’ life satisfaction with three self-report items that indicate life satisfaction in the past, present, and future. Ratings are made on a 10-point scale ranging from ‘‘best possible life’’ to ‘‘worst possible life’’ (20), providing a global rating of life satisfaction that has been used in both population studies and clinical survivor samples (21-23). Risk Factors. For these analyses, we considered sex, age at diagnosis and interview, length of followup, race/ethnicity, marital status, educational attainment, annual household income, and health insurance as independent variables in our multiple variable models. Major medical condition was included as a covariate in the models and was derived from information provided by participants about medical late effects. Participants who reported complete deafness, kidney dialysis, congestive heart failure, myocardial infarction, angioplasty, bypass surgery, stroke, liver cirrhosis, a heart, lung, or kidney transplant, amputation, joint replacement or second cancer, and/or current use of seizure medications, medications for heart problems or high blood pressure, chemotherapy, immune suppressants, or oxygen were classified as having a major medical condition (24). Diagnosis, treatment, and related information were obtained from medical records. Data Analysis. Descriptive statistics were calculated for demographic and treatment variables and compared between survivors and siblings with generalized estimating equations (25). To account for sibling-survivor pairs, mixed models were also used to calculate and compare age- and gender-adjusted mean scores between siblings and survivors overall and, by diagnosis, on subscales and summary scales for the BSI, the SF-36, and the LOL (26). Mean scores on the BSI-18 and SF-36 were compared among study participants and ageand gender-specific population norms with one-sample t tests. Frequencies and percents of dichotomized outcomes for the psychosocial, HRQOL, and life satisfaction scales were calculated and compared among survivors using both demographic and treatment characteristics as predictors in multiple variable logistic regression models. Statistical Analysis System version 9.1 was used for analysis. Bonferroni corrections (n = 17) were used to reduce errors related to multiple tests, with a levels set at 0.003. Results Characteristics of the Study Population. Participants were more likely than nonparticipants to be female, older than 24 years of age, white, college educated, married, and employed than were nonparticipants (data not shown). Survivor participants did not differ from nonparticipants by cancer diagnosis, survival time, or baseline BSI scores. As expected, based on their random selection for participation in the psychosocial portion of the questionnaire, sibling participants did not differ from nonparticipants by sex, age, race, educational attainment, employment, marital status, or scores on the BSI at baseline. Demographic characteristics of participating survivors and siblings are shown in Table 1. Survivors had a median age of 32 (18-54) years and siblings had a median age of 33 (18-58) years. Among survivors, median age at diagnosis was 7 (0-20) years and median survival time Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 Cancer Epidemiology, Biomarkers & Prevention Table 1. Characteristics of the study population Gender Male Female Age at second follow-up (y) 18-24 25-34 35+ Race/ethnicity White Black Hispanic Other Unknown Educational attainment <High school High school graduate College graduate Unanswered Marital status Single Married/living as married Divorced/separated Unanswered Employment Employed or caring for home Student Looking for work/ unable to work Unanswered Annual household income $20,000+ <$20,000 Health insurance Yes No Major medical condition Yes No Diagnosis Acute lymphoblastic leukemia Acute myeloid leukemia Other or unspecified leukemia Astrocytomas Medulloblastoma, PNET Other CNS tumors Hodgkin’s disease NHL Wilm’s tumor Neuroblastoma Soft tissue sarcoma Ewing’s sarcoma Osteosarcoma Other bone Age at diagnosis (y) 0-3 4-9 10-14 15-20 Survival time (y) <20 20-24 25-29 30+ Surgery Yes No Survivors, n (%) Siblings, n (%) 3,481 (48.7) 3,666 (51.3) 186 (47.9) 202 (52.1) Table 1. Characteristics of the study population (Cont’d) P* 0.77 0.001 1,482 (20.7) 3,169 (44.3) 2,496 (34.9) 61 (15.7) 157 (40.5) 170 (43.8) 6,500 179 261 182 25 (90.9) (2.5) (3.7) (2.5) (0.3) 347 9 9 5 18 (89.4) (2.3) (2.3) (1.3) (4.6) 278 3,549 3,254 66 (3.9) (49.7) (45.5) (0.9) 9 183 194 2 (2.3) (47.2) (50.0) (0.5) 3,136 3,432 506 73 (43.9) (48.0) (7.1) (1.0) 111 226 47 4 (28.6) (58.2) (12.1) (1.0) <0.001 Survivors, n (%) Medical record unavailable Chemotherapy Yes No Medical record unavailable Radiation Cranial Other than cranial None Medical record unavailable Siblings, n (%) P* 410 (5.7) 5,326 (74.5) 1,411 (19.7) 410 (5.7) 2,057 2,415 2,265 410 (28.8) (33.8) (31.7) (5.7) Abbreviation: PNET, primitive neuroectodermal tumor. *From generalized estimating equations to allow for intrafamily correlations. 0.16 5,822 (81.5) <0.001 was 23 siblings and not medical <0.001 Survivors (and by Diagnostic Subgroup) versus Siblings. Age- and gender-adjusted means and SEs from generalized linear mixed models on each of the BSI, SF-36, and LOL scales are shown in Table 2A to C. 356 (91.8) 372 (5.2) 803 (11.2) 15 (3.9) 15 (3.9) 150 (2.1) 2 (0.5) 6,367 (89.1) 780 (10.9) 363 (93.6) 25 (6.4) 6,362 (89.0) 785 (11.0) 360 (92.8) 28 (7.2) 1,251 (17.5) 5,896 (82.5) 18 (4.6) 370 (95.4) 0.01 <0.02 <0.001 2,090 (29.2) 170 (2.4) 146 (2.0) 548 195 143 955 533 671 448 631 194 395 28 (7.7) (2.7) (2.0) (13.4) (7.5) (9.4) (6.3) (8.8) (2.7) (5.5) (0.4) 2,211 2,137 1,497 1,302 (30.9) (29.9) (20.9) (18.2) 1,985 2,432 1,829 801 (27.8) (34.0) (25.6) (11.2) 5,403 (75.6) 1,334 (18.7) (15-34) years. Cases were more likely than to be younger, white, single, not employed, insured; have lower income; and have a major condition. Emotional Health (BSI-18). Compared with siblings, survivors reported more symptoms of global distress, depression, anxiety, and somatization, although scores are lower (better) than population norms for both groups. Survivors of acute lymphoblastic leukemia, astrocytomas, CNS tumors other than medulloblastoma, Hodgkin’s disease, NHL, Wilm’s tumor, soft tissue sarcoma, Ewing’s sarcoma, and osteosarcoma reported higher levels of global distress. Survivors of astrocytoma, NHL, Ewing’s sarcoma, and osteosarcoma reported significantly higher depressive symptoms, anxiety, and somatization. Generally, survivors and siblings had fewer symptoms than the general population, with survivors of astrocytoma reporting more depression and survivors of Hodgkin’s disease reporting more somatization than population norms. HRQOL (SF-36). Whereas survivors and siblings scored higher than norms in mental health, survivors scored lower than population norms on all other aspects of HRQOL, except for pain and the mental component summary, and lower than siblings on the physical component summary of the SF-36; however, sibling and survivor means did not differ significantly on the mental component summary, a pattern persisting for survivors across diagnostic groups, except for survivors of other or unspecified leukemia and bone cancer other than Ewing’s sarcoma or osteosarcoma. General health subscale means were also lower for survivors than siblings. Survivors of CNS tumors, lymphoma, soft tissue, or bone malignancies reported more problems in physical function, role physical, general health, and social function domains than did siblings. Bone cancer survivors also reported significant bodily pain. In addition, survivors of osteosarcoma had lower mean scores than siblings on the role emotional and mental health subscales. Survivors of astrocytoma also scored lower on the mental health subscale, and survivors of NHL scored lower on the vitality subscale when compared with siblings. Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 437 438 Psychological Distress, HRQOL, and Life Satisfaction Table 2. Means and SEs on BSI, SF-36, and LOL for survivors and siblings, overall and by diagnosis A. Means and SEs on the BSI for survivors and siblings, overall and by diagnosis U.S. population Siblings Survivors Leukemia Acute lymphoblastic leukemia Acute myeloid leukemia Other or unspecified leukemia CNS malignancies Astrocytomas Medulloblastoma, PNET Other CNS tumors Hodgkin’s disease NHL Wilm’s tumor Neuroblastoma Soft tissue sarcoma Bone tumors Ewing’s sarcoma Osteosarcoma Other bone Depression Anxiety Somatization Global status index Mean (95% CI) Mean (95% CI) Mean (95% CI) Mean (95% CI) 50.00 (49.44-50.56) 47.46* (46.50-48.42) 49.33c (49.11-49.55) 50.00 (49.44-50.56) 46.36* (45.46-47.26) 47.87*,c (47.65-48.09) 50.00 (49.44-50.56) 47.80* (46.92-48.68) 49.03* (50.19-50.59) 50.00 (49.44-50.56) 46.64* (45.64-47.64) 49.17c (48.93-49.41) 47.62* (47.23-48.01) 50.12 (49.73-50.51) 48.84*,c (48.39-49.29) 49.05 (47.60-50.50) 47.73* (46.36-49.10) 50.52 (49.19-51.85) 48.97 (47.44-50.50) 49.33* (47.76-50.90) 47.80 (46.31-49.29) 49.23 (47.80-50.66) 49.00 (47.35-50.65) 51.61*,c (50.81-52.41) 50.53* (49.18-51.88) 47.88*,c (47.12-48.64) 45.77* (44.48-47.06) 50.79c (50.06-51.52) 50.48c (49.25-51.71) 50.31c (49.47-51.15) 48.77 (47.36-50.18) 50.91* (49.34-52.48) 47.67* (46.18-49.16) 50.30c (48.87-51.73) 49.87c (48.22-51.52) 49.08* (48.43-49.73) 48.49*,c (47.86-49.12) 51.43*,c (50.84-52.02) 49.86c (49.17-50.55) 49.49* (48.67-50.31) 48.15* (47.41-48.89) 48.45 (47.55-49.35) 49.18 (48.44-49.92) 48.02*,c (47.24-48.80) 47.84* (47.13-48.55) 47.21* (46.35-48.07) 48.13*,c (47.42-48.84) 50.39c 49.78 50.06 50.48c (49.65-51.13) (49.09-50.47) (49.22-50.90) (49.79-51.17) 49.18c (48.32-50.04) 48.43*,c (47.65-49.21) 48.34 (47.38-49.30) 49.26c (48.48-50.04) 49.88* (48.53-51.23) 50.22* (49.26-51.18) 47.07 (43.52-50.62) 48.10*,c (46.81-49.39) 48.93* (48.01-49.85) 47.97* (44.58-51.36) 49.52c (48.29-50.75) 50.74c (49.86-51.62) 49.37 (46.12-52.62) 49.31c (47.90-50.72) 49.85c (48.83-50.87) 47.85 (44.13-51.57) (48.62-49.44) B. Means and SEs on the SF-36 for survivors and siblings, overall and by diagnosis U.S. population Siblings Survivors Leukemia Acute lymphoblastic leukemia Acute myeloid leukemia Other or unspecified leukemia CNS malignancies Astrocytomas Medulloblastoma, PNET Other CNS tumors Hodgkin’s disease NHL Wilm’s tumor Neuroblastoma Soft tissue sarcoma Bone tumors Ewing’s sarcoma Osteosarcoma Other bone Physical function Role physical Bodily pain General health Vitality Mean (95% CI) Mean (95% CI) Mean (95% CI) Mean (95% CI) Mean (95% CI) 53.26 (52.75-53.76) 52.50 (51.93-53.08) 54.98* (54.12-55.84) 52.27 (50.98-53.56) ,c 51.30* (51.10-51.50) 49.87*,c (49.58-50.16) 52.38* (52.01-52.75) 50.96* (50.39-51.53) 51.95 (50.68-53.22) 49.30*,c (47.36-51.24) 51.67 (51.03-52.32) 50.99 (50.32-51.66) 52.76 (51.78-53.74) 53.02* (51.94-54.10) 51.62 (51.38-51.86) 49.16*,c (48.91-49.41) 49.32 (48.63-50.01) 45.43* (44.23-46.63) 44.43* (44.16-44.70) 50.05c (49.58-50.52) 45.02* (44.49-45.55) 51.47 (50.00-52.94) 48.74*,c (47.11-50.37) 46.10* (44.30-47.90) 51.87 (51.44-52.30) 49.61c (47.87-51.35) 44.89* (42.95-46.83) 49.35*,c (48.64-50.06) 48.14*,c (47.06-49.22) 48.16*,c (46.96-49.36) 46.76*,c (44.96-48.56) 51.69 (50.87-52.51) 49.26*,c (48.36-50.16) 52.21 (50.84-53.58) 48.62*,c (47.11-50.13) 43.53* (42.53-44.53) 45.98* (44.29-47.67) 49.23*,c (47.84-50.62) 46.61*,c (44.51-48.71) 51.21 (49.60-52.82) 48.14*,c (46.38-49.90) 44.60* (42.64-46.56) 52.61 (51.24-53.98) ,c 51.94* ,c 51.57 (49.49-53.65) ,c (51.37-52.51) 49.13* (48.25-50.01) 52.30 (50.71-53.89) ,c 52.05 (51.38-52.72) 46.73* ,c (46.00-47.46) 43.96* (43.14-44.78) ,c 51.99* (51.26-52.72) 49.70* (48.60-50.80) 51.98 (51.14-52.82) 49.12* (48.20-50.04) 43.29*,c (42.27-44.31) 45.14* (44.20-46.08) 53.01 (52.34-53.68) 51.61 (50.61-52.61) 52.20 (51.44-52.96) 49.78c (48.94-50.62) 52.50 (51.70-53.30) 51.16 (49.94-52.38) 51.92 (51.00-52.84) 49.85* (48.83-50.87) 45.00* (43.86-46.14) ,c ,c ,c ,c 43.63* (42.69-44.57) 51.60* (50.93-52.27) 49.53* (48.53-50.53) 51.05* (50.29-51.81) 48.94* (48.10-49.78) 49.24*,c (48.04-50.44) 48.63*,c (46.81-50.45) 49.92*,c (48.53-51.31) 49.26*,c (47.73-50.79) ,c ,c ,c ,c 43.64* (42.78-44.50) 47.49* (46.20-48.78) 48.72* (47.74-49.70) 49.22* (48.14-50.30) 52.60 (49.44-55.76) 52.19 (47.43-56.95) 52.54 (48.91-56.17) 52.01 (48.01-56.01) (Continued on the following page) Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 43.37* (41.68-45.06) 43.52* (42.30-44.74) 45.15 (40.70-49.60) Cancer Epidemiology, Biomarkers & Prevention Table 2. Means and SEs on BSI, SF-36, and LOL for survivors and siblings, overall and by diagnosis (Cont’d) B. Means and SEs on the SF-36 for survivors and siblings, overall and by diagnosis Role emotional Social function Mental health Physical component summary Mental component summary Mean (95% CI) Mean (95% CI) Mean (95% CI) Mean (95% CI) Mean (95% CI) 50.41 (49.73-51.09) 51.41 (50.41-52.41) 49.42*,c (49.18-49.66) 48.86 (48.13-49.58) 56.11* (55.13-57.09) 55.20c (54.96-55.44) 52.56 (52.56-53.64) 53.27 (52.27-54.27) 50.04*,c (49.80-50.28) 48.79 (48.06-49.51) 50.02 (48.77-51.27) 49.43 (49.14-49.72) 49.71* (49.28-50.14) 55.34* (54.91-55.77) 51.08*,c (50.65-51.51) 49.48 (48.93-50.03) 49.82 (48.31-51.33) 56.22* (54.73-57.71) 49.49*,c (47.98-51.00) 51.02 (49.12-52.92) 49.87 (48.24-51.50) 55.71 (54.10-57.32) 51.59 (49.96-53.22) 48.93 (46.87-50.99) 47.92*,c (47.08-48.76) 47.85*,c (46.44-49.26) 54.18*,c (53.36-55.00) 55.37* (53.98-56.76) 48.94*,c (48.10-49.78) 47.77*,c (46.36-49.18) 48.80 (47.74-49.86) 50.32 (48.54-52.10) 48.50* (46.85-50.15) 54.99* (53.38-56.60) 48.10*,c (46.47-49.73) 49.13 (47.05-51.21) 49.47*,c (48.78-50.16) 49.58* (48.72-50.44) 50.63 (49.85-51.41) 50.00 (49.04-50.96) 49.19* (48.41-49.97) 55.49* 54.66* 55.47* 55.76* 55.21* 49.53*,c 50.53*,c 51.58*,c 50.89*,c 49.84*,c 49.35 48.62 49.58 50.12 49.10 48.04*,c (46.63-49.45) 55.21* (53.82-56.60) 48.21*,c (46.80-49.62) 49.55 (47.77-51.33) 48.51*,c (47.49-49.53) 52.36 (48.64-56.08) 54.12*,c (53.12-55.12) 56.56* (52.89-60.23) 45.72*,c (44.72-46.72) 51.49 (47.79-55.19) 49.75 (48.48-51.02) 51.73 (47.05-56.41) U.S. population 50.87 (50.21-51.53) Siblings 48.83 (47.26-50.40) Survivors 47.22* (46.85-47.59) Leukemia Acute 47.66* (46.97-48.35) lymphoblastic leukemia Acute myeloid 48.74* (46.39-51.09) leukemia Other or 46.32* (43.77-48.87) unspecified leukemia CNS malignancies Astrocytomas 46.84* (45.53-48.15) Medulloblastoma, 46.78* (44.58-48.98) PNET Other 45.10* (42.53-47.67) CNS tumors Hodgkin’s disease 47.07* (46.01-48.13) NHL 46.89* (45.56-48.22) Wilm’s tumor 47.70* (46.48-48.92) Neuroblastoma 48.63* (47.14-50.12) Soft tissue 46.95* (45.72-48.18) sarcoma Bone tumors Ewing’s 47.11* (44.90-49.32) sarcoma Osteosarcoma 44.86*,c (43.29-46.43) Other bone 50.46 (44.66-56.26) (54.82-56.16) (53.82-55.50) (54.71-56.23) (54.82-56.70) (54.45-55.97) (48.84-50.22) (49.67-51.39) (50.80-52.36) (49.95-51.83) (49.06-50.62) (48.49-50.21) (47.54-49.70) (48.60-50.56) (48.92-51.32) (48.12-50.08) C. Means and SEs on the Cantril LOL for survivors and siblings, overall and by diagnosis U.S. population Siblings Survivors Leukemia Acute lymphoblastic leukemia Acute myeloid leukemia Other or unspecified leukemia CNS malignancies Astrocytomas Medulloblastoma, PNET Other CNS tumors Hodgkin’s disease NHL Wilm’s tumor Neuroblastoma Soft tissue sarcoma Bone tumors Ewing’s sarcoma Osteosarcoma Other bone Current 5 y ago 5 y in future Mean (95% CI) Mean (95% CI) Mean (95% CI) 6.90 (6.73-7.07) 7.35* (7.17-7.53) 7.33c (7.29-7.37) 6.10 (6.95-6.25) 6.36 (6.14-6.58) 6.42c (6.38-6.46) 8.30 (8.09-8.51) 8.75c (8.59-8.91) 8.56c (8.52-8.60) 7.39c (7.31-7.47) 6.39c (6.29-6.49) 8.59c (8.51-8.67) 7.29 (7.02-7.56) 6.52 (6.21-6.83) 8.45 (8.21-8.69) 7.25 (6.96-7.54) 6.33 (6.00-6.66) 8.42 (8.17-8.67) 7.03c (6.87-7.19) 7.15 (6.90-7.40) 6.26 (6.08-6.44) 6.36 (6.07-6.65) 8.22* (8.08-8.36) 8.21* (7.97-8.45) 6.98 (6.69-7.27) 7.37c (7.25-7.49) 7.38c (7.22-7.54) 7.42c (7.28-7.56) 7.49c (7.31-7.67) 7.24c (7.10-7.38) 6.27 (5.92-6.62) 6.45c (6.31-6.59) 6.60c (6.42-6.78) 6.52c (6.36-6.68) 6.61c (6.41-6.81) 6.27* (6.11-6.43) 8.19* (7.94-8.44) 8.61c (8.51-8.71) 8.76c (8.62-8.90) 8.65c (8.53-8.77) 8.72c (8.56-8.88) 8.48 (8.36-8.60) 7.29c (7.04-7.54) 7.30c (7.12-7.48) 7.89c (7.24-8.54) 6.58c (6.29-6.87) 6.42c (6.20-6.64) 6.67 (5.91-7.43) 8.43 (8.21-8.65) 8.61 (8.45-8.77) 9.11 (8.52-9.70) NOTE: Scale 0 to 100: higher scores indicate more depression, anxiety, somatization, and overall emotional difficulties. Scale 0 to 100: lower scores indicate lower HRQOL. Adjusted for age, sex, and intrafamily correlation. Siblings were the reference group. Scale 0 to 10: lower scores indicate lower self-estimate of life satisfaction. *U.S. population reference group P < 0.003 adjusted for age and sex. cSiblings were the reference group P < 0.003 adjusted for age, sex, and intrafamily correlation. Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 439 440 Psychological Distress, HRQOL, and Life Satisfaction Table 3. Frequencies and percents of survivors with poor outcomes on BSI and SF-36 by socioeconomic variables A. Frequencies and percents of survivors with poor outcomes on the BSI (ORs and 95% CIs comparing poor outcomes by sociodemographic variables) Depression n (%) Gender Male 373 Female 495 Age at second follow-up (y) 18-24 200 25-34 361 35+ 307 Race/ethnicity White 775 Black 20 Hispanic 40 Other 33 Educational attainment <High school 52 High school 494 graduate College graduate 317 Marital status Single 488 Married/living 270 as married Divorced/separated 103 Employment Employed/caring 581 for home Student 44 Looking for work/ 229 unable to work Annual household income $20,000+ 672 <$20,000 196 Health insurance Yes 721 No 147 Major medical condition Yes 193 No 675 Anxiety Somatization Global status index OR (95% CI) n (%) OR (95% CI) n (%) OR (95% CI) n (%) OR (95% CI) (10.7) (13.5) Reference 1.3 (1.1-1.5) 220 (6.3) 369 (10.1) Reference 1.7 (1.4-2.0) 371 (10.7) 609 (16.6) Reference 1.7 (1.4-1.9) 298 (8.6) 454 (12.4) Reference 1.5 (1.3-1.8) (13.5) (11.4) (12.3) Reference 1.0 (0.8-1.2) 1.3 (1.0-1.6) 146 (9.9) 248 (7.8) 195 (7.8) Reference 0.8 (0.6-1.0) 0.9 (0.6-1.1) 182 (12.3) 427 (13.5) 371 (14.9) Reference 1.1 (0.9-1.3) 1.2 (0.9-1.5) 173 (11.7) 311 (9.8) 268 (10.7) Reference 0.9 (0.7-1.1) 1.1 (0.9-1.5) (11.9) (11.2) (15.3) (15.9) Reference 0.7 (0.4-1.1) 1.2 (0.8-1.7) 1.1 (0.7-1.7) 524 18 30 17 (8.1) (10.1) (11.5) (8.2) Reference 1.0 (0.6-1.6) 1.3 (0.9-2.0) 0.8 (0.4-1.4) 874 31 54 21 (13.4) (17.3) (20.7) (10.1) Reference 1.1 (0.7-1.7) 1.5 (1.1-2.1) 0.6 (0.4-1.1) 665 25 40 22 (10.2) (14.0) (15.3) (10.6) Reference 1.0 (0.7-1.6) 1.4 (1.0-2.0) 0.8 (0.5-1.4) (18.7) (13.9) 1.2 (0.9-1.8) 1.2 (1.0-1.4) 43 (15.5) 331 (9.3) 1.6 (1.1-2.3) 1.2 (1.0-1.4) 63 (22.7) 562 (15.8) 1.6 (1.2-2.3) 1.4 (1.2-1.6) 54 (19.4) 433 (12.2) 1.6 (1.1-2.2) 1.3 (1.1-1.5) (9.7) Reference 210 (6.5) Reference 342 (10.5) Reference 258 (7.9) Reference (15.6) (7.9) 1.9 (1.6-2.3) Reference 289 (9.2) 226 (6.6) 1.1 (0.9-1.4) Reference 414 (13.2) 445 (13.0) 0.8 (0.7-1.0) Reference 387 (12.3) 268 (7.8) 1.3 (1.1-1.6) Reference (20.4) 2.2 (1.7-2.9) 1.6 (1.1-2.1) 107 (21.1) 1.2 (0.9-1.6) 86 (17.0) 1.7 (1.2-2.2) (10.0) Reference 394 (6.8) Reference 648 (11.1) Reference 478 (8.2) Reference (11.8) (28.5) 1.0 (0.7-1.4) 2.5 (2.0-3.0) 30 (8.1) 157 (19.6) 1.0 (0.6-1.5) 2.5 (2.0-3.1) 36 (9.7) 273 (34.0) 0.9 (0.6-1.3) 3.4 (2.8-4.1) 37 (9.9) 223 (27.8) 1.0 (0.7-1.5) 3.1 (2.5-3.7) (10.6) (25.1) Reference 1.8 (1.5-2.2) 463 (7.3) 126 (16.2) Reference 1.6 (1.3-2.0) 777 (12.2) 203 (26.0) Reference 1.7 (1.4-2.1) 575 (9.0) 177 (22.7) Reference 1.8 (1.5-2.3) (11.3) (18.7) Reference 1.3 (1.0-1.7) 490 (7.7) 99 (12.6) Reference 1.3 (1.0-1.7) 830 (13.0) 150 (19.1) Reference 1.3 (1.0-1.4) 618 (9.7) 134 (17.1) Reference 1.3 (1.1-1.7) (15.4) (11.4) 1.2 (1.0-1.4) Reference 133 (10.6) 456 (7.7) 1.2 (1.0-1.6) Reference 235 (18.8) 745 (12.6) 1.3 (1.1-1.6) Reference 170 (13.6) 582 (9.9) 1.2 (1.0-1.4) Reference 67 (13.2) B. Frequencies and percents of survivors with poor outcomes on the SF-36 (ORs and 95% CIs comparing poor outcomes by sociodemographic variables) Physical function n (%) Role physical OR (95% CI) n (%) OR (95% CI) Bodily pain n (%) OR (95% CI) General health n (%) OR (95% CI) Vitality n (%) OR (95% CI) Gender Male 311 (8.9) Reference 586 (16.8) Reference 377 (10.8) Reference 547 (15.7) Reference 1,115 (32.0) Reference Female 483 (13.2) 1.7 (1.4-2.0) 837 (22.8) 1.5 (1.3-1.7) 573 (15.6) 1.6 (1.3-1.8) 845 (23.0) 1.7 1.5-1.9 1,735 (47.3) 1.9 (1.7-2.1) Age at second follow-up (y) 18-24 115 (7.8) Reference 223 (15.0) Reference 139 (9.4) Reference 223 (15.0) Reference 546 (36.8) Reference 25-34 292 (9.2) 1.3 (1.0-1.7) 576 (18.2) 1.4 (1.1-1.7) 379 (12.0) 1.4 (1.1-1.7) 575 (18.1) 1.3 (1.1-1.6) 1,264 (39.9) 1.2 (1.0-1.3) 35+ 387 (15.5) 2.4 (1.8-2.3) 624 (25.0) 2.2 (1.7-2.7) 432 (17.3) 2.1 (1.7-2.8) 594 (23.8) 1.8 (1.5-2.3) 1,040 (41.7) 1.2 (1.0-1.4) Race/ethnicity White 701 (10.8) Reference 1,262 (19.4) Reference 843 (13.0) Reference 1,244 (19.1) Reference 2,594 (39.9) Reference Black 32 (17.9) 1.1 (0.7-1.8) 52 (29.1) 1.2 (0.8-1.8) 33 (18.4) 1.2 (0.8-1.8) 45 (25.1) 1.0 (0.7-1.5) 73 (40.8) 0.9 (0.6-1.2) Hispanic 41 (15.7) 1.4 (0.9-2.0) 67 (25.7) 1.3 (1.0-1.8) 47 (18.0) 1.3 (0.9-1.8) 61 (23.4) 1.2 (0.9-1.6) 110 (42.1) 1.0 (0.8-1.3) Other 20 (9.7) (0.7 0.4-1.2) 42 (20.3) 1.0 (0.6-1.5) 27 (13.0) 1.0 (0.6-1.6) 42 (20.3) 1.0 (0.6-1.4) 73 (35.3) 0.8 (0.6-1.1) Educational attainment <High 73 (26.3) 2.5 (1.7-3.5) 93 (33.5) 1.6 (1.2-2.2) 67 (24.1) 1.9 (1.4-2.7) 90 (32.4) 1.9 (1.4-2.5) 122 (43.9) 1.0 (0.8-1.3) school (Continued on the following page) Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 Cancer Epidemiology, Biomarkers & Prevention Table 3. Frequencies and percents of survivors with poor outcomes on BSI and SF-36 by socioeconomic variables (Cont’d) B. Frequencies and percents of survivors with poor outcomes on the SF-36 (ORs and 95% CIs comparing poor outcomes by sociodemographic variables) Physical function n (%) High school graduate College graduate Marital status Single Married/ living as married Divorced/ separated Employment Employed/ caring for home Student Looking for work/ unable to work Annual household income $20,000+ <$20,000 Health insurance Yes No Major medical condition Yes No Role physical n (%) OR (95% CI) OR (95% CI) Bodily pain n (%) OR (95% CI) General health n (%) OR (95% CI) Vitality n (%) OR (95% CI) 446 (12.6) 1.4 (1.2-1.7) 773 (21.8) 1.3 (1.1-1.4) 542 (15.3) 1.4 (1.2-1.7) 768 (21.6) 1.4 (1.2-1.6) 1,461 (41.2) 1.1 (1.0-1.2) 256 (7.9) 523 (16.1) Reference 544 (16.7) Reference 332 (10.2) Reference Reference 1,238 (38.0) Reference 358 (11.4) 0.9 (0.7-1.1) 338 (9.8) Reference 632 (20.2) 1.0 (0.9-1.2) 391 (12.5) 0.8 (0.7-1.0) 630 (18.4) Reference 443 (12.9) Reference 584 (18.6) 0.9 (0.8-1.0) 1,227 (39.1) 0.9 (0.8-1.0) 648 (18.9) Reference 1,351 (39.4) Reference 92 (18.2) 1.3 (0.9-1.7) 149 (29.4) 1.2 (1.0-1.6) 108 (21.3) 1.2 (0.9-1.5) 149 (29.4) 1.2 (1.0-1.6) 899 (15.4) Reference 591 (10.2) Reference 940 (16.1) Reference 2,171 (37.3) Reference 67 (18.0) 1.5 (1.1-2.0) 44 (11.8) 1.5 (1.1-2.2) 426 (53.1) 5.1 (4.3-6.1) 293 (36.5) 4.1 (3.4-5.0) 56 (15.1) 1.1 (0.8-1.5) 365 (45.5) 1.3 (1.1-1.4) 410 (7.0) Reference 43 (11.6) 2.3 (1.6-3.4) 318 (39.6) 6.5 (5.3-7.9) 247 (48.8) 1.2 (1.0-1.4) 136 (36.6) 1.0 (0.8-1.3) 481 (59.9) 2.2 (1.9-2.6) 608 (9.5) Reference 1,152 (18.1) Reference 759 (11.9) Reference 1,127 (17.7) Reference 2,415 (37.9) Reference 186 (23.8) 1.8 (1.5-2.3) 271 (34.7) 1.6 (1.3-2.0) 191 (24.5) 1.6 (1.3-1.9) 265 (34.0) 1.7 (1.4-2.1) 435 (55.8) 1.7 (1.5-2.1) 701 (11.0) Reference 1,250 (19.6) Reference 818 (12.9) Reference 1,221 (19.2) Reference 2,518 (39.6) Reference 93 (11.8) 1.3 (1.0-1.8) 173 (22.0) 1.3 (1.0-1.6) 132 (16.8) 1.0 (0.8-1.2) 171 (21.8) 1.1 (0.9-1.4) 332 (42.3) 1.0 (0.9-1.2) 362 (28.9) 3.9 (3.2-4.6) 410 (32.8) 1.7 (1.5-2.3) 270 (21.6) 1.6 (1.3-1.9) 368 (29.4) 1.5 (1.3-1.8) 594 (47.5) 1.3 (1.1-1.5) 432 (7.3) Reference 1012 (17.2) Reference 680 (11.5) Reference 1023 (17.4) Reference 2,255 (38.2) Reference Role emotional n (%) OR (95% CI) Social function n (%) Gender Male 540 (15.5) Reference 439 Female 802 (21.9) 1.5 (1.3-1.7) 634 Age at second follow-up (y) 18-24 296 (20.0) Reference 228 25-34 570 (18.0) 0.9 (0.8-1.1) 446 35+ 476 (19.1) 1.1 (0.9-1.3) 399 Race/ ethnicity White 1,192 (18.3) Reference 949 Black 37 (20.7) 0.9 (0.6-1.3) 31 Hispanic 60 (23.0) 1.2 (0.9-1.6) 54 Other 53 (25.6) 1.5 (1.0-2.1) 39 Educational attainment <High 75 (27.0) 1.2 (0.9-1.6) 71 school High 713 (20.1) 1.1 (0.9-1.2) 623 school graduate OR (95% CI) Mental health n (%) OR (95% CI) Physical component summary n (%) OR (95% CI) Mental component summary n (%) OR (95% CI) (12.6) Reference 266 (7.6) Reference 456 (13.1) Reference (17.3) 1.5 (1.3-1.7) 381 (10.4) 1.4 (1.2-11.7) 681 (18.6) 1.6 (1.4-1.8) 595 (17.1) Reference 844 (23.0) 1.4 (1.3-1.6) (15.4) Reference 153 (10.3) Reference (14.1) 1.0 (0.8-1.2) 277 (8.7) 0.8 (0.7-1.1) (16.0) 1.3 (1.0-1.6) 217 (8.7) 0.9 (0.7-1.1) 321 (21.7) Reference 636 (20.1) 1.0 (0.8-1.1) 482 (19.3) 1.0 (0.8-1.2) (14.6) Reference (17.3) 0.8 (0.5-1.3) (20.7) 1.4 (1.0-1.9) (18.8) 1.3 (0.9-1.9) 576 (8.9) 21 (11.7) 29 (11.1) 21 (10.1) 141 (9.5) Reference 442 (13.9) 1.6 (1.3-2.0) 554 (22.2) 2.8 (2.2-3.6) Reference 1,016 (15.6) Reference 1,278 (19.7) Reference 1.1 (0.6-1.7) 37 (20.7) 1.0 (0.6-1.5) 40 (22.3) 0.9 (0.6-1.4) 1.1 (0.8-1.7) 53 (20.3) 1.2 (0.9-1.8) 64 (24.5) 1.2 (0.9-1.6) 1.1 (0.7-1.8) 31 (15.0) 0.9 (0.6-1.4) 57 (27.5) 1.5 (1.1-2.1) (25.5) 1.6 (1.1-2.2) 49 (17.6) 1.5 (1.1-2.2) 80 (28.8) 2.0 (1.4-2.7) 76 (27.3) 1.1 (0.8-1.5) (17.6) 1.4 (1.2-1.6) 355 (10.0) 1.1 (0.9-1.3) 633 (17.8) 1.5 (1.2-1.7) 761 (21.4) 1.0 (0.9-1.2) (Continued on the following page) Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 441 442 Psychological Distress, HRQOL, and Life Satisfaction Table 3. Frequencies and percents of survivors with poor outcomes on BSI and SF-36 by socioeconomic variables (Cont’d) Role emotional n (%) College 542 (16.7) graduate Marital status Single 639 (20.4) Married/ 553 (16.1) living as married Divorced/ 135 (26.7) separated Employment Employed/ 933 (16.0) caring for home Student 81 (21.8) Looking for 299 (37.2) work/unable to work Annual household income $20,000+ 1,090 (17.1) <$20,000 252 (32.3) Health insurance Yes 1,147 (18.0) No 195 (24.8) Major medical condition Yes 283 (22.6) No 1,058 (17.9) OR (95% CI) Social function n (%) OR (95% CI) Mental health n (%) OR (95% CI) Reference 365 (11.2) Reference 238 (7.3) Physical component summary n (%) OR (95% CI) Mental component summary n (%) OR (95% CI) 410 (12.6) Reference 589 (18.1) Reference 1.1 (1.0-1.3) 525 (16.7) 1.1 (1.0-1.3) 314 (10.0) 1.1 (0.9-1.3) Reference 420 (12.2) Reference 250 (7.3) Reference 447 (14.3) 0.7 (0.6-0.9) 559 (16.3) Reference 699 (22.3) 1.2 (1.0-1.4) 582 (17.0) Reference 1.4 (1.1-1.8) 114 (22.5) 1.4 (1.1-1.8) 75 (14.8) 1.5 (1.1-2.0) 124 (24.5) 1.1 (0.8-1.4) 142 (28.1) 1.4 (1.2-1.8) Reference 668 (11.5) Reference 424 (7.3) Reference 674 (11.6) Reference 1,027 (17.6) Reference 1.4 (1.0-1.8) 63 (16.9) 1.4 (1.1-2.0) 31 (8.3) 0.9 (0.6-1.4) 2.5 (2.1-3.0) 317 (39.5) 3.7 (3.1-4.5) 181 (22.5) 2.8 (2.2-3.4) 51 (13.7) 2.0 (1.4-2.8) 385 (47.9) 6.3 (5.2-7.6) 76 (20.4) 1.1 (0.8-1.4) 305 (38.0) 2.3 (1.9-2.8) Reference 835 (13.1) Reference 501 (7.9) Reference 1.7 (1.4-2.0) 238 (30.5) 1.9 (1.6-2.3) 146 (18.7) 1.7 (1.4-2.2) 916 (14.4) Reference 1,169 (18.4) Reference 221 (28.3) 1.6 (1.3-1.9) 270 (34.6) 1.7 (1.4-2.0) Reference 915 (14.4) Reference 521 (8.2) Reference 1,007 (15.8) Reference 1,223 (19.2) Reference 1.2 (1.0-1.4) 158 (20.1) 1.0 (0.8-1.2) 126 (16.1) 1.5 (1.2-1.9) 130 (16.6) 1.3 (1.0-1.7) 216 (27.5) 1.3 (1.0-1.5) 1.1 (1.0-1.3) 264 (21.1) 1.3 (1.1-1.5) 140 (11.2) 1.2 (0.9-1.4) Reference 808 (13.7) Reference 507 (8.6) Reference 383 (30.6) 2.2 (1.8-2.5) 284 (22.7) 1.0 (0.9-1.2) 754 (12.8) Reference 1,154 (19.6) Reference NOTE: Models adjusted for all variables in left column of the table. Compared with age-relevant U.S. population norms, survivors had poorer outcomes on physical function, role physical, general health, vitality, role emotional, and social function domains as well as physical component but had better outcomes on the mental health subscale. This pattern persisted for survivors across diagnostic groups, except for those with leukemia, Wilm’s tumor, neuroblastoma, and bone cancer other than Ewing’s sarcoma or osteosarcoma. Compared with norms, siblings had better outcomes on physical function, general health, and mental health domains and poorer outcomes on the vitality domain. Life Satisfaction (LOL). Overall, survivors and siblings reported high levels of current and predicted life satisfaction, except for CNS tumor survivors who predicted lower levels of satisfaction 5 years into the future than did siblings. Both survivors and siblings reported better current and future life satisfaction than did the general population. Demographic and Social Factors. Frequencies and percents of having poor psychosocial or quality of life among survivors by sociodemographic characteristics are shown in Table 3A and B with odds ratios (OR) and 95% confidence intervals (95% CI). Emotional Health (BSI-18). In adjusted models, female gender, lower educational attainment, unemployment, annual household income <$20,000, lack of health insurance, being African-American, and having a major medical condition were associated with increased risk for reporting symptoms of depression, anxiety, somatization, and global distress. Current age over 35 years was also associated with higher risk of reporting depressive symptoms. Compared with those who were married/ living as married, unmarried survivors were more likely to report depressive symptoms and global distress. Divorced or separated individuals also reported more symptoms of anxiety when compared with those who were married/living as married. Hispanics were more likely than Whites to report symptoms of somatization and global distress. HRQOL (SF-36). Female gender, unemployment, annual household income <$20,000, and lack of health insurance were associated with poor HRQOL across all summaries and subscales of the SF-36. Participants with a major medical condition were more likely than those without to report poor HRQOL across most domains, with the exception of mental health subscale and mental component summary scale. Older age and lower educational attainment were associated with increased risk of reporting poor physical HRQOL (physical component summary, general health, physical function, role physical, and bodily pain subscales), less vitality, and poor social function. Compared with Whites, Hispanics were at increased risk of reporting poor outcomes on role physical and social function subscales. Other ethnic minorities (nonBlack and non-Hispanic) were at increased risk of reporting poor HRQOL in role emotional and mental health domains. Compared with those who were married/living as married, unmarried survivors were at increased risk of reporting poor outcomes on role emotional, social function, and mental health subscales. When compared with those who were married/living as Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 Cancer Epidemiology, Biomarkers & Prevention Table 4. Frequencies and percents of survivors with poor outcomes on BSI and SF-36 by treatment variables A. Frequencies and percents of survivors with poor outcomes on the BSI (ORs and 95% CIs comparing poor outcomes by treatment variables) Depression Gender Male Female Age at diagnosis (y) 0-3 4-9 10-14 15-20 Survival time (y) <20 20-24 25-29 30+ Surgery Yes No Chemotherapy Yes No Radiation Cranial Other than cranial None Anxiety Somatization Global status index n (%) OR (95% CI) n (%) OR (95% CI) n (%) OR (95% CI) n (%) OR (95% CI) 351 (10.8) 472 (13.6) Reference 1.3 (1.1-1.5) 206 (6.3) 347 (10.0) Reference 1.7 (1.4-2.0) 343 (10.5) 575 (16.6) Reference 1.7 (1.5-2.0) 278 (8.5) 427 (12.3) Reference 1.53 (1.3-1.8) 261 251 160 151 (12.5) (12.6) (11.3) (12.2) 1.0 (0.8-1.2) 1.0 (0.8-1.2) 0.9 (0.7-1.1) Reference 184 170 103 96 (8.8) (8.5) (7.3) (7.7) 1.1 (0.8-1.4) 1.1 (0.8-1.5) 0.9 (0.7-1.2) Reference 248 277 204 189 (11.9) (13.9) (14.5) (15.2) 0.8 (0.6-0.9) 0.9 (0.7-1.1) 1.0 (0.8-1.2) Reference 222 219 141 123 (10.6) (11.0) (10.0) (9.9) 1.1 (0.8-1.4) 1.1 (0.9-1.4) 1.0 (0.8-1.3) Reference 243 (12.9) 280 (11.8) 207 (12.1) 93 (12.3) 1.0 (0.8-1.3) 0.9 (0.7-1.2) 1.0 (0.7-1.2) Reference 171 195 129 58 (9.1) (8.2) (7.5) (7.7) 1.1 (0.8-1.6) 1.0 (0.8-1.4) 1.0 (0.7-1.3) Reference 249 311 239 119 (13.2) (13.1) (13.9) (15.8) 0.8 (0.7-1.1) 0.8 (0.6-1.0) 0.9 (0.7-1.1) Reference 207 (11.0) 222 (9.3) 185 (10.8) 91 (12.1) 0.9 (0.7-1.2) 0.7 (0.6-1.0) 0.9 (0.7-1.1) Reference 652 (12.1) 171 (12.8) 1.1 (0.9-1.4) Reference 435 (8.1) 118 (8.8) 1.1 (0.8-1.4) Reference 733 (13.6) 185 (13.9) 1.0 (0.8-1.2) Reference 566 (10.5) 139 (10.4) 1.2 (0.9-1.5) Reference 646 (12.1) 177 (12.5) 1.0 (0.8-1.2) Reference 450 (8.4) 103 (7.3) 1.2 (0.9-1.5) Reference 736 (13.8) 182 (12.9) 1.1 (0.9-1.4) Reference 565 (10.6) 140 (9.9) 1.1 (0.9-1.4) Reference 287 (14.0) 264 (10.9) 272 (12.0) 1.2 (1.0-1.5) 0.9 (0.7-1.1) Reference 159 (7.7) 189 (7.8) 205 (9.1) 0.9 (0.7-1.1) 0.9 (0.7-1.1) Reference 275 (13.4) 372 (15.4) 271 (12.0) 1.1 (1.0-1.4) 1.3 (1.1-1.5) Reference 214 (10.4) 251 (10.4) 240 (10.6) 1.0 (0.8-1.2) 1.0 (0.8-1.2) Reference B. Frequencies and percents of survivors with poor outcomes on the SF-36 (ORs and 95% CIs comparing poor outcomes by treatment variables) Physical function n (%) Gender Male 292 (8.9) Female 457 (13.2) Age at diagnosis (y) 0-3 171 (8.2) 4-9 189 (9.5) 10-14 188 (13.3) 15-20 201 (16.2) Survival time (y) <20 164 (8.7) 20-24 247 (10.4) 25-29 223 (13.0) 30+ 115 (15.2) Surgery Yes 653 (12.1) No 96 (7.2) Chemotherapy Yes 565 (10.6) No 184 (13.0) Radiation Cranial 239 (11.6) Other 281 (11.6) than cranial None 229 (10.1) OR (95% CI) n (%) OR (95% CI) Bodily pain n (%) General health n (%) OR (95% CI) OR (95% CI) Vitality n (%) OR (95% CI) Reference 1.7 (1.4-2.0) 549 (16.8) Reference 346 (10.6) Reference 791 (22.8) 1.5 (1.3-1.7) 539 (15.5) 1.6 (1.4-1.8) 511 (15.7) Reference 1,031 (31.6) Reference 794 (22.9) 1.6 (1.4-1.9) 1,653 (47.6) 2.0 (1.8-2.2) 0.5 (0.4-0.6) 0.5 (0.4-0.7) 0.8 (0.6-1.0) Reference 323 374 330 313 (15.5) 0.5 (0.4-0.7) 217 (10.4) 0.5 (0.4-0.7) (18.7) 0.7 (0.6-0.8) 232 (11.6) 0.6 (0.5-0.8) (23.4) 0.9 (0.7-1.1) 221 (15.7) 0.9 (0.7-1.0) (25.2) Reference 215 (17.3) Reference 346 362 292 305 (16.6) 0.6 (0.5-0.8) (18.1) 0.7 (0.6-0.9) (20.7) 0.8 (0.7-1.0) (24.6) Reference 790 785 607 502 (37.8) 0.9 (0.8-1.0) (39.3) 1.0 (0.8-1.1) (43.0) 1.1 (1.0-1.3) (40.5) Reference 0.5 (0.4-0.7) 0.6 (0.5-0.8) 0.8 (0.6-1.0) Reference 340 456 364 180 (18.0) 0.7 (0.6-0.9) 225 (11.9) 0.7 (0.5-0.9) (19.1) 0.8 (0.6-0.9) 290 (12.2) 0.7 (0.5-0.9) (21.2) 0.8 (0.7-1.0) 243 (14.2) 0.8 (0.6-1.0) (23.8) Reference 127 (16.8) Reference 322 448 338 197 (17.1) 0.6 (0.5-0.8) (18.8) 0.7 (0.6-0.8) (19.7) 0.7 (0.6-0.8) (26.1) Reference 723 937 717 307 (38.3) 0.9 (0.8-1.1) (39.3) 1.0 (0.8-1.1) (41.8) 1.0 (0.9-1.3) (40.7) Reference 1.9 (1.5-2.5) 1,106 (20.5) 1.2 (1.0-1.5) 726 (13.4) 1.2 (1.0-1.4) 1,063 (19.7) 1.1 (0.9-1.3) 2,149 (39.8) 1.1 (1.0-1.3) Reference 234 (17.5) Reference 159 (11.9) Reference 242 (18.1) Reference 535 (40.1) Reference 1.0 (0.9-1.2) 1,033 (19.4) 1.0 (0.8-1.1) 696 (13.1) 1.1 (0.9-1.4) 1,036 (19.5) 1.1 (1.0-1.6) 2,093 (39.3) 0.9 (0.8-1.1) Reference 307 (21.8) Reference 189 (13.4) Reference 269 (19.1) Reference 591 (41.9) Reference 1.3 (1.1-1.6) 0.9 (0.7-1.1) Reference Role emotional n (%) Role physical OR (95% CI) Gender Male 505 (15.5) Reference Female 763 (22.0) 1.6 (1.4-1.8) 434 (21.1) 1.4 (1.2-1.6) 263 (12.8) 1.1 (0.9-1.3) 523 (21.7) 1.2 (1.0-1.4) 345 (14.3) 1.0 (0.9-1.2) 387 (18.8) 1.3 (1.1-1.6) 572 (23.7) 1.6 (1.3-1.8) 872 (42.4) 1.1 (1.0-1.3) 981 (40.6) 1.1 (0.9-1.2) 383 (16.9) 346 (15.3) 831 (36.7) Reference Social function n (%) 408 (12.5) 600 (17.3) OR (95% CI) 277 (12.2) Reference Mental health n (%) Reference Physical component summary Mental component summary n (%) OR (95% CI) n (%) OR (95% CI) 422 (12.9) 646 (18.6) Reference 1.6 (1.4-1.9) 556 (17.0) 802 (23.1) Reference 1.5 (1.3-1.7) OR (95% CI) Reference 244 (7.5) Reference 1.5 (1.3-1.7) 352 (10.1) 1.4 (1.2-1.7) Reference (Continued on the following page) Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 443 444 Psychological Distress, HRQOL, and Life Satisfaction Table 4. Frequencies and percents of survivors with poor outcomes on BSI and SF-36 by treatment variables (Cont’d) B. Frequencies and percents of survivors with poor outcomes on the SF-36 (ORs and 95% CIs comparing poor outcomes by treatment variables) Role emotional n (%) Age at diagnosis (y) 0-3 397 4-9 378 10-14 266 15-20 227 Survival time (y) <20 356 20-24 437 25-29 325 30+ 150 Surgery Yes 1,024 No 244 Chemotherapy Yes 1,001 No 267 Radiation Cranial 381 Other 447 than cranial None 440 OR (95% CI) Social function n (%) Mental health OR (95% CI) n (%) OR (95% CI) Physical component summary n (%) OR (95% CI) Mental component summary n (%) OR (95% CI) (19.0) (18.9) (18.9) (18.3) 1.0 (0.9-1.3) 1.1 (0.9-1.3) 1.0 (0.9-1.3) Reference 320 289 213 186 (15.3) (14.5) (15.1) (15.0) 1.0 (0.8-1.3) 201 (9.6) 1.2 (0.9-1.6) 1.0 (0.8-1.2) 182 (9.1) 1.2 (0.9-1.5) 1.0 (0.8-1.2) 118 (8.4) 1.1 (0.8-1.4) Reference 95 (7.7) Reference 239 272 266 291 (11.4) (13.6) (18.9) (23.5) 0.4 (0.3-0.5) 0.5 (0.4-0.6) 0.7 (0.7-0.9) Reference 436 415 283 224 (20.9) (20.8) (20.1) (18.1) 1.2 (1.0-1.5) 1.2 (1.0-1.5) 1.2 (1.0-1.4) Reference (18.9) (18.3) (19.0) (19.9) 0.9 (0.7-1.2) 0.9 (0.7-1.1) 0.9 (0.8-1.2) Reference 277 331 272 128 (14.7) (13.9) (15.9) (17.0) 0.9 (0.7-1.1) 173 (9.2) 0.9 (0.7-1.2) 0.8 (0.6-1.0) 192 (8.1) 0.8 (0.6-1.1) 0.9 (0.7-1.2) 159 (9.3) 1.0 (0.7-1.3) Reference 72 (9.5) Reference 235 356 306 171 (12.5) (14.9) (17.9) (22.6) 0.5 (0.4-0.6) 0.7 (0.6-0.9) 0.7 (0.6-0.9) Reference 379 478 355 146 (20.1) (20.1) (20.7) (19.3) 1.2 (1.0-1.5) 1.2 (1.0-1.5) 1.2 (1.0-1.4) Reference (19.0) 1.2 (1.0-1.4) 821 (15.2) 1.2 (1.0-1.5) 472 (8.7) 1.1 (0.9-1.4) 906 (16.8) 1.5 (1.2-1.8) 1,097 (20.3) 1.2 (1.0-1.4) (18.3) Reference 187 (14.0) Reference 124 (9.3) Reference 162 (12.1) Reference 261 (19.6) Reference (18.8) 1.0 (0.9-1.2) 785 (14.7) 1.0 (0.8-1.1) 480 (9.0) 1.1 (0.9-1.4) 821 (15.4) 1.1 (0.9-1.3) 1,071 (20.1) 1.0 (0.9-1.2) (18.9) Reference 223 (15.8) Reference 116 (8.2) 247 (17.5) Reference 287 (20.3) Reference (18.5) 1.0 (0.8-1.1) 318 (15.5) 1.1 (1.0-1.4) 186 (9.0) 1.0 (0.8-1.2) 330 (16.0) 1.4 (1.2-1.6) (18.5) 0.9 (0.8-1.1) 364 (15.1) 1.0 (0.9-1.2) 200 (8.3) 0.9 (0.7-1.1) 438 (18.1) 1.1 (1.0-1.4) 400 (19.4) 0.9 (0.8-1.1) 481 (19.9) 0.9 (0.8-1.1) (19.4) Reference 326 (14.4) Reference 210 (9.3) Reference 300 (13.2) Reference 477 (21.1) Reference NOTE: Models adjusted for all variables in left column of the table. married, divorced or separated individuals also reported an increased prevalence of problems in role physical, general heath, and vitality domains. Treatment Factors. Frequencies and percents of having a poor psychosocial or quality of life outcome among survivors by treatment characteristics are shown in Table 4A and B with ORs and 95% CIs from unconditional logistic regression models. Emotional Health (BSI-18). In adjusted models, the only predictor of poor emotional health was previous treatment with cranial radiation, with only modest strength. Survivors treated with cranial radiation were at a slightly higher risk of reporting depressive symptoms compared with those without cranial radiation. HRQOL (SF-36). After adjusting for gender, age at diagnosis and survival time, and treatments with surgery, chemotherapy, and cranial radiation therapy, were each associated with higher risk of reporting poor HRQOL in physical function, role physical, and general health subscales and on the physical component summary. In multiple variable models, history of surgery was associated with elevated risk of poor HRQOL in physical function, role physical, bodily pain, vitality, role emotional, and social function subscales and in physical and mental components when compared with those without surgical history, although association magnitude was modest, except for physical function (OR, 1.9; 95% CI, 1.5-2.5). Survivors who received chemotherapy compared with those without reported poor HRQOL only in general health. Younger age at diagnosis was associated with decreased risk of poor HRQOL in physical function, role physical, bodily pain, and general health subscales and in the physical component sum- mary. Survivors >25 years reported better HRQOL in physical function, role physical, bodily pain, general health, and physical component summary compared with survivors >30 years. Discussion Whereas adult survivors of childhood cancer from the CCSS report more symptoms of psychological distress compared with siblings, both groups report better psychological adjustment than that of population norms. Survivors report poorer HRQOL in physical and social but not in mental health domains compared with siblings. Compared with U.S. population norms, survivors have increased risk of poor HRQOL in physical and social domains, with the largest effect size in vitality. Compared with population norms, siblings fare better in physical function and general health, and both survivors and siblings report better mental health than does the general population, as well as high levels of current life satisfaction. Except for CNS tumor survivors, both groups also expect high life satisfaction in 5 years. Our findings add to information from previous CCSS estimates of health status (24) and chronic disease (27). Despite their increased risk for poor health status, and the fact that >70% of childhood cancer survivors report a chronic health condition, survivors’ expectation of future life satisfaction is excellent. Survivors of CNS tumors, lymphoma, bone, and soft tissue sarcomas have the lowest mean HRQOL scores. Female gender, lower educational attainment, unmarried status, annual household income <$20,000, unemployment, lack of medical insurance, and having a major medical condition are all associated with a higher risk of Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 Cancer Epidemiology, Biomarkers & Prevention psychological distress and poor outcomes in some aspects of HRQOL. Previous treatment with cranial radiation and surgery are associated with poor HRQOL, particularly in physical domains. Participants diagnosed <10 years of age or treated in the past 25 years report better HRQOL than those diagnosed >10 years of age or treated >30 years ago. Our findings support the low mean psychological distress found in a study of 161 childhood cancer survivors (28, 29) on the SCL-90-R (30), the parent instrument of the BSI-18, and yet are consistent with another investigation (31) of 101 survivors where f32% screened positive for psychological distress on the SCL90-R, with a history of cranial radiation and poor physical health as predictors. Our results extend earlier CCSS findings of increased depression and somatization in survivors of leukemia and lymphoma (9), brain tumor (8), and solid tumors (10) compared with siblings. Our findings are also consistent with earlier reports of associations between poor HRQOL and female gender (32-35), older age (35), lower educational attainment (33), unemployment (33), and medical limitations (33). Others found being survivors >26 years (32) and treatment with cranial radiation or surgery (34, 35) as risks for poor physical HRQOL. Younger age at diagnosis and decreased risk of poor physical HRQOL in our study contradicts another study of 2,152 childhood cancer survivors (35) that used the Health Utilities Index Mark III, a discrepancy possibly explained by differences in the focus of the Health Utilities Index Mark III versus SF-36. Although our findings are based on a large sample, varied diagnoses, and participants from 26 children’s cancer centers throughout North America, they should not be considered without taking into account potential study limitations. First, we used only self-report data to characterize outcomes. Clinical interviews may have improved the precision of our estimates, particularly those related to psychological distress. Second, the SF-36 is a generic HRQOL measure. To investigate the physical and psychological functioning of these survivors more systematically, more specific measures may be needed. Change over time with longitudinal repeated measures assessments is needed to determine stability of our findings and the developmental trajectory of HRQOL in this population. In addition, the survivor participants in our study were more likely than nonparticipants to be female, white, married, employed, and college graduates. It is possible that these successful survivors were more aware of their levels of achievement and thus either more or less likely to express dissatisfaction with their outcome. Based on our data, we could interpret the findings of our study as good news. Overall, most of the measures indicate that survivors and siblings both report lower psychological distress and better HRQOL, as well as life satisfaction, in comparison with population norms. Where there were differences, generally effect sizes were small, except for the vitality subscale as noted above. In fact, our sample seems to report significantly better mental health than that of population norms, with a large effect size. We could explain our findings as ‘‘posttraumatic growth’’ or the psychological resilience that develops in coping with adverse circumstances (36, 37). That is, experiencing childhood cancer or being a young sibling of a sister or brother with cancer inoculates individuals to other negative life experiences and provides them with feelings of life satisfaction and overall psychological well being. In one study, lower level of worry during cancer treatment was related to ultimate life satisfaction (37). On the other hand, there are some data indicating that most people show life satisfaction even with very poor health states, such as amputation (38, 39), and several studies indicating that survivors of cancers in general and childhood cancers in particular may be biased reporters and tend to deny difficulties and overestimate their positive health and satisfaction (40-44). O’Leary et al. (45) reported from a sample of Dana-Farber patients participating in CCSS that survivors had a strong tendency toward an enhanced self-appraisal and such bias had a differential effect on self-reported physical and emotional quality of life. Unlike smaller cohort studies, our large sample permits analyses that identify vulnerable subgroups and suggest specific diagnostic/treatment pathways to psychological symptoms and poor HRQOL. Understanding reasons for pain in bone tumor survivors or poor future outlook in CNS tumor survivors might lead to earlier preventive strategies, such as better pain management during bone cancer treatment or early educational interventions for children with CNS tumors (46). Rather than implying poor HRQOL in all survivors, we have identified certain survivor groups with more severe effect and suggest the need for prospective, longitudinal, in-depth examination of pathways and mediators of psychological distress and poor HRQOL. Studies of these high-risk subgroups can inform strategies designed to reduce psychosocial and HRQOL sequelae. References 1. 2. 3. 4. 5. 6. 7. 8. 9. National Cancer Institute. U.S. estimated complete prevalence counts on 1/1/2002. Available from: http://srab.cancer.gov/prevalence/ canques.html. Casillas JN, Zebrack BJ, Zeltzer LK. Health-related quality of life for Latino survivors of childhood cancer. J Psychosoc Oncol 2006;24: 125 – 45. Langeveld NE, Stam H, Grootenhuis MA, Last BF. Quality of life in young adult survivors of childhood cancer. Support Care Cancer 2002;10:579 – 600. Seitzman RL, Glover DA, Meadows AT, et al. Self-concept in adult survivors of childhood acute lymphoblastic leukemia: a cooperative Children’s Cancer Group and National Institutes of Health study. Pediatr Blood Cancer 2004;42:230 – 40. Stam H, Grootenhuis MA, Caron HN, Last BF. Quality of life and current coping in young adult survivors of childhood cancer: positive expectations about the further course of the disease were correlated with better quality of life. Psychooncology 2006;15: 31 – 43. Zeltzer LK, Chen E, Weiss R, et al. Comparison of psychologic outcome in adult survivors of childhood acute lymphoblastic leukemia versus sibling controls: a cooperative Children’s Cancer Group and National Institutes of Health study. J Clin Oncol 1997;15: 547 – 56. Nagarajan R, Clohisy DR, Neglia JP, et al. Function and quality-of-life of survivors of pelvic and lower extremity osteosarcoma and Ewing’s sarcoma: the Childhood Cancer Survivor Study. Br J Cancer 2004;91: 1858 – 65. Zebrack BJ, Gurney JG, Oeffinger K, et al. Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivor study. J Clin Oncol 2004;22:999 – 1006. Zebrack BJ, Zeltzer LK, Whitton J, et al. Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin’s disease, and non-Hodgkin’s lymphoma: a report from the Childhood Cancer Survivor Study. Pediatrics 2002;110:42 – 52. Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008 445 446 Psychological Distress, HRQOL, and Life Satisfaction 10. Zebrack BJ, Zevon MA, Turk N, et al. Psychological distress in longterm survivors of solid tumors diagnosed in childhood: a report from the childhood cancer survivor study. Pediatr Blood Cancer 2007;49: 47 – 51. 11. Nathan PCNK, Greenberg ML, Hudson M, et al. Health-related quality of life in adult survivors of childhood Wilms tumor or neuroblastoma: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer 2007;49:704 – 15. 12. Zebrack B, Zeltzer LK, Whitton J, Berkow R, Chesler MA. Survivors of childhood cancer: using siblings as a control group. Pediatrics 2003;112:1454 – 5. 13. Robison LL, Green DM, Hudson M, et al. Long-term outcomes of adult survivors of childhood cancer. Cancer 2005;104:2557 – 64. 14. Robison LL, Mertens AC, Boice JD, et al. Study design and cohort characteristics of the Childhood Cancer Survivor Study: a multiinstitutional collaborative project. Med Pediatr Oncol 2002;38:229 – 39. 15. Mertens AC, Walls RS, Taylor L, et al. Characteristics of childhood cancer survivors predicted their successful tracing. J Clin Epidemiol 2004;57:933. 16. Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595 – 605. 17. Derogatis L. Brief Symptom Inventory (BSI) 18. Administration, scoring, and procedures manual. Minneapolis (MN): NCS Pearson, Inc.; 2000. 18. Recklitis CJ, Parsons SK, Shih MC, Mertens A, Robison LL, Zeltzer L. Factor structure of the brief symptom inventory-18 in adult survivors of childhood cancer: results from the childhood cancer survivor study. Psychol Assess 2006;18:22 – 32. 19. Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473 – 83. 20. Cantril H. The pattern of human concerns. New Brunswick (NJ): Rutgers University Press; 1965. 21. Ashing-Giwa K, Ganz PA, Petersen L. Quality of life of AfricanAmerican and white long term breast carcinoma survivors. Cancer 1999;85:418 – 26. 22. Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst 2002;94:39 – 49. 23. Taylor P, Funk C, Craighill P. Americans see less progress on their ladder of life. Washington (DC): Pew Research Center; 2006. 24. Hudson MM, Mertens AC, Yasui Y, et al. Health status of adult longterm survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Jama 2003;290:1583 – 92. 25. Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13 – 22. 26. McCullock C, Searle S. Generalized, linear, and mixed models. Wiley (NY): John Wiley & Sons, Inc.; 2001. 27. Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 2006;355:1572 – 82. 28. Derogatis LR. SCL-90-R Symptom Checklist-90-R. Minneapolis (MN): National Computer Systems, Inc.; 1994. 29. Elkin TD, Phipps S, Mulhern RK, Fairclough D. Psychological functioning of adolescent and young adult survivors of pediatric malignancy. Med Pediatr Oncol 1997;29:582 – 8. 30. Derogatis L. SCL-90-R: administration, scoring and procedures manual. Minneapolis (MN): National Computer Systems; 1997. 31. Recklitis C, O’Leary T, Diller L. Utility of routine psychological screening in the childhood cancer survivor clinic. J Clin Oncol 2003; 21:787 – 92. 32. Blaauwbroek R, Stant AD, Groenier KH, Kamps WA, Meyboom B, Postma A. Health-related quality of life and adverse late effects in adult (very) long-term childhood cancer survivors. European Journal of Cancer 2007;43:122. 33. Langeveld NE, Grootenhuis MA, Voûte PA, de Haan RJ, van den Bos C. Quality of life, self-esteem and worries in young adult survivors of childhood cancer. Psychooncology 2004;13:867 – 81. 34. Maunsell E, Pogany L, Barrera M, Shaw AK, Speechley KN. Quality of life among long-term adolescent and adult survivors of childhood cancer. J Clin Oncol 2006;24:2527 – 35. 35. Pogany L, Barr RD, Shaw A, Speechley KN, Barrera M, Maunsell E. Health status in survivors of cancer in childhood and adolescence. Quality of Life Research 2006;15:143 – 57. 36. Zebrack BJ, Zeltzer LK. Quality of life issues and cancer survivorship. Curr Probl Cancer 2003;27:198 – 211. 37. Zebrack BJ, Chesler M. Health-related worries, self-image, and life outlooks of long-term survivors of childhood cancer. Health Soc Work 2001;26:245 – 56. 38. Albrecht G, Devlieger P. The disability paradox: high quality of life against all odds. Soc Sci Med 1999;48:977 – 88. 39. Asendorpf J, Ostendorf F. Is self-enhancement healthy? Conceptual, psychometric, and empirical analysis. J Pers Soc Psychol 1998;74: 955 – 66. 40. Phipps S, Steele RG, Hall K, Leigh L. Repressive adaptation in children with cancer: a replication and extension. Health Psychol 2001;20:445 – 51. 41. Phipps S, Srivastava D. Repressive adaptation in children with cancer. Health Psychol 1997;16:521 – 8. 42. Phipps S, Steele R. Repressive adaptive style in children with chronic illness. Psychosom Med 2002;64:34 – 42. 43. Zachariae R, Jensen AB, Pedersen C, et al. Repressive coping before and after diagnosis of breast cancer. Psychooncology 2004; 13:547 – 61. 44. Breetvelt I, Van Dam F. Underreporting by cancer patients: the case of response-shift. Soc Sci Med 1991;32:981 – 7. 45. O’Leary T, Diller L, Recklitis CJ. The effects of response bias on selfreported quality-of-life among childhood cancer survivors. Quality of Life Research 2007;16:1211 – 20. 46. Glover DA, Byrne J, Mills JL, et al. Impact of CNS treatment on mood in adult survivors of childhood leukemia: a report from the Children’s Cancer Group. J Clin Oncol 2003;21:4395 – 401. Cancer Epidemiol Biomarkers Prev 2008;17(2). February 2008