What We Have Learned About the Predictors
of Preterm Birth
Robert L. Goldenberg, Jay D. Iams, Brian M. Mercer, Paul Meis,
Atef Moawad, Anita Das, Rachel Copper, and Francee Johnson for the
National Institute of Child Health and Human Development
Maternal-Fetal Medicine Units Network
The Preterm Prediction Study conducted by the Maternal Fetal Medicine Network between 1993 and
1996 studied a large number of risk factors for preterm birth in more than 3,000 women at 10 centers.
The goals of the study were to better understand the strength of one risk factor versus another and
to explore interactions among the predictors looking for combinations of factors that were more
predictive of preterm birth than any single factor used alone. The most potent factors that were
associated with spontaneous preterm birth at <32 weeks were a positive cervical-vaginal fetal
fibronectin test (odds ratio, 32.7) and <10th percentile cervical length (odds ratio, 5.8), and in serum,
>90th percentiles of ␣-fetoprotein (odds ratio, 8.3) and alkaline phosphatase (odds ratio, 6.8), and
>75th percentile of granulocyte colony-stimulating factor (odds ratio, 5.5). Results for spontaneous
preterm birth at <35 weeks were generally similar but not as strong. The overlap among the strongest
biologic markers for predicting spontaneous preterm birth was small. This suggests that the use of
tests such as maternal ␣-fetoprotein, alkaline phosphatase, and granulocyte colony-stimulating factor
as a group or adding their results to fetal fibronectin and cervical length test results may enhance our
ability to predict spontaneous preterm birth and that the development of a multiple-marker test for
spontaneous preterm birth is feasible.
© 2003 Elsevier Inc. All rights reserved.
reterm birth (PTB) is the major obstetric
problem in developed countries, accounting for the majority of neonatal mortality and a
considerable portion of the long-term neurologic handicap.1 Despite increases in the percent
of women receiving prenatal care, the widespread availability of nutrition supplementation
programs, and the availability of several tocolytic
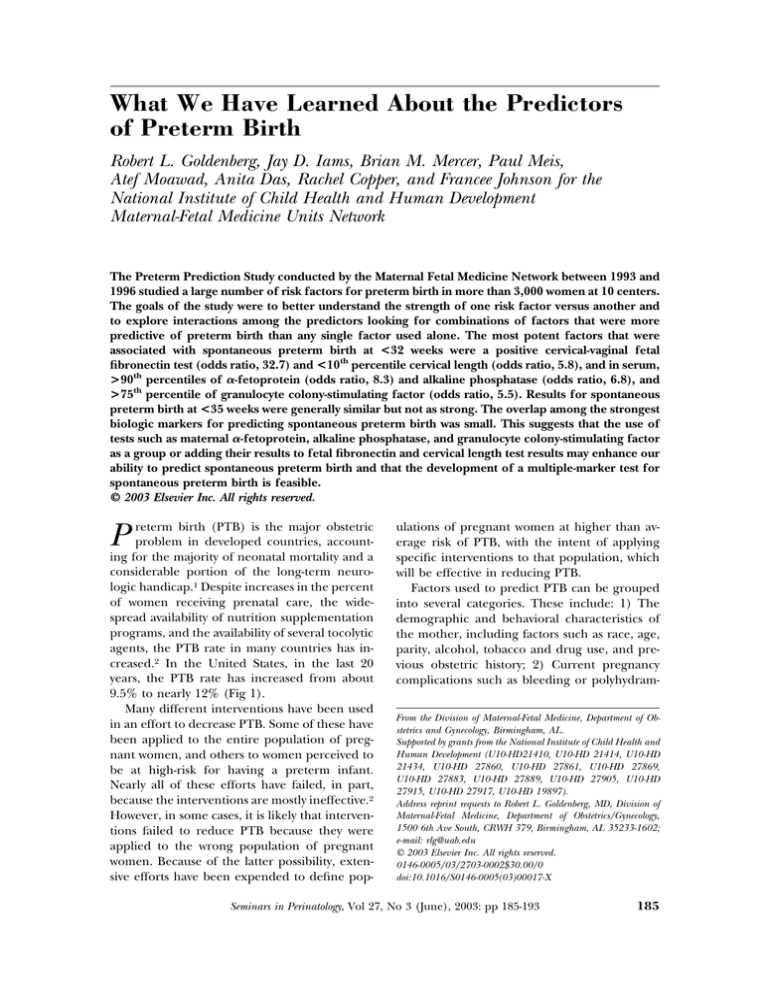
agents, the PTB rate in many countries has increased.2 In the United States, in the last 20
years, the PTB rate has increased from about
9.5% to nearly 12% (Fig 1).
Many different interventions have been used
in an effort to decrease PTB. Some of these have
been applied to the entire population of pregnant women, and others to women perceived to
be at high-risk for having a preterm infant.
Nearly all of these efforts have failed, in part,
because the interventions are mostly ineffective.2
However, in some cases, it is likely that interventions failed to reduce PTB because they were
applied to the wrong population of pregnant
women. Because of the latter possibility, extensive efforts have been expended to define pop-
P
ulations of pregnant women at higher than average risk of PTB, with the intent of applying
specific interventions to that population, which
will be effective in reducing PTB.
Factors used to predict PTB can be grouped
into several categories. These include: 1) The
demographic and behavioral characteristics of
the mother, including factors such as race, age,
parity, alcohol, tobacco and drug use, and previous obstetric history; 2) Current pregnancy
complications such as bleeding or polyhydramFrom the Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, Birmingham, AL.
Supported by grants from the National Institute of Child Health and
Human Development (U10-HD21410, U10-HD 21414, U10-HD
21434, U10-HD 27860, U10-HD 27861, U10-HD 27869,
U10-HD 27883, U10-HD 27889, U10-HD 27905, U10-HD
27915, U10-HD 27917, U10-HD 19897).
Address reprint requests to Robert L. Goldenberg, MD, Division of
Maternal-Fetal Medicine, Department of Obstetrics/Gynecology,
1500 6th Ave South, CRWH 379, Birmingham, AL 35233-1602;
e-mail: rlg@uab.edu
© 2003 Elsevier Inc. All rights reserved.
0146-0005/03/2703-0002$30.00/0
doi:10.1016/S0146-0005(03)00017-X
Seminars in Perinatology, Vol 27, No 3 (June), 2003: pp 185-193
185
186
Goldenberg et al
Figure 1. Incidence of preterm birth in the United States, 1981-2000.
nios; 3) Maternal nutritional status, most often
defined by the body mass index, but including
various vitamin and mineral measurements; 4)
Various biophysical characteristics such as the
cervical length or funneling as measured by ultrasound, or effacement, dilatation, and consistency as determined by digital examination, and
contraction frequency; 5) Various maternal psychosocial characteristics such as stress or anxiety;
6) Extrauterine infections such as periodontal
disease or bacterial vaginosis; and finally, 7) A
wide variety of biochemical tests using various
bodily fluids.
The Preterm Prediction Study conceived by
The Maternal Fetal Medicine Network in 1992,
and conducted between 1993 and 1996, was an
attempt to study risk factors from each of these
categories in a single large population of pregnant women and to understand the strength of
one predictor versus another. We also hoped to
explore interactions among the predictors, looking for combinations of factors that may be more
predictive of PTB than any single factor used
alone. Ultimately, it was hoped that rational interventions could be targeted to women with
specific risk factors. By doing so, we hoped to
reduce the potential for failure seen with many
previous attempts to reduce preterm births
when the interventions were applied to all pregnant women.
Attempts to predict PTB have been made over
the years with varying degrees of success. However, different from the Preterm Prediction
Study, most previous attempts investigated a single risk factor or a single category of risk factors.
In addition, except for those studies that used
vital records, the populations studied were often
relatively small and often confined to a single
medical center or geographic area.
Perhaps the most well known attempt at predicting PTB is that of Creasy and Liggins,3 who
created a scoring system by using maternal demographic and past pregnancy history characteristics. With their system, women characterized
as high-risk had about a 2-fold increase in PTB.
Many other investigators confirmed that a previous history of PTB was among the strongest
predictors of PTB in the current pregnancy. Various cervical characteristics, first measured digitally and then by ultrasound have been reported
to be associated with PTB by a large number of
investigators.4,5 An effaced cervix, dilatation,
and especially a soft cervical consistency often
predicted a 3-fold increased risk of a PTB.4 A
short cervix by ultrasound was thought to predict about a 5-fold or greater risk of PTB.5 The
presence of uterine contractions had been studied previously, often as part of a home uterine
activity monitoring program.6 There are conflicting data available as to the ability of contraction monitoring to predict PTB. The results of
self-reported contracting are reviewed here,
while the monitoring data, collected in a parallel
study are reported elsewhere in this edition. In
recent years, bacterial vaginosis (BV) has been
studied extensively and generally has been asso-
Predictors of Preterm Birth
ciated with a 2-fold increase in PTB.7 Finally at
the time of the study, cervical/vaginal fetal fibronectin had been shown to be a strong predictor of preterm birth, but mostly in women
with symptoms or preterm labor.8,9 Because of
its reported power to predict spontaneous preterm birth (SPTB), we collected extensive data
on fetal fibronectin.
The Preterm Prediction Study
Conducted at 10 medical centers in the United
States between 1993 and 1996, more than 3,000
women were recruited at approximately 24
weeks’ gestation and were evaluated at 24, 26,
28, and 30 weeks’ gestation. Delivery records
were abstracted: 2,929 women were the mothers
of singleton infants and 147 the mothers of
twins. Singleton and twin pregnancies were generally considered separately. Extensive questionnaire data were collected at the 24-week visit.
Blood, urine, and a vaginal Gram-stain for BV
were collected at the 24- and 28-week visits, and
cervical and vaginal fluids were collected for
fetal fibronectin (FFN) measurements at each of
the 4 visits. The questionnaire data were available on all women in the study, as were the BV
Gram-stains. Fetal fibronectin test results were
determined for all women from all cervical and
vaginal samples. However, for many of the other
tests, because of limited resources, a retrospective nested case control design was used. Therefore, for these women, test results are available
only for the women with preterm births and
their matched controls.
Prior to beginning the study, we choose to use
as our primary endpoint, SPTB at less than 35
weeks’ gestation. However, many of the analyses
also evaluated SPTB occurring at less than 28,
32, and 37 weeks’ as well. Spontaneous preterm
birth was defined as a PTB after the spontaneous
onset of contractions or membrane rupture, regardless of whether the delivery was vaginal or by
cesarean section, or in the case of membrane
rupture, induced. SPTB at less than 28 weeks’
was found in 0.8% of births, at less than 30
weeks’ in 1.1%, at less than 32 weeks’ in 1.9%, at
less than 35 weeks’ in 5.1%, and at less than 37
weeks’ in 11.9%.
187
Results
The Preterm Prediction Study confirmed some
of the known associations between maternal demographic, behavioral and medical characteristics, and preterm birth.10 For example, black
women had significantly more SPTB than white
women (OR ⫽1.5). Women with a previous PTB
were more likely to have a SPTB than women
who had a prior term pregnancy. On the other
hand, a number of factors that in some prior
studies had been associated with SPTB were not
associated with SPTB in this study. These factors
included maternal age less than 18 years, low
educational level, a history of spontaneous or
induced abortions, smoking, drug or alcohol
use, most medical complications, urinary tract
infections, and symptoms such as pelvic pressure
or diarrhea.10 The reasons for these discrepancies are not totally clear, but many of the previously reported associations were weak with relative risks of less than 2, and often needed very
large populations to show statistical significance,
numbers generally found in vital statistic-type
studies. For example, maternal smoking has consistently been found to be associated with SPTB,
but with a relative risk of about 1.2 to 1.3.11 With
this very weak association, it would not be expected to show a significant relationship with
SPTB in a population of only 3,000 women.
The relationship between a previous SPTB
and the current pregnancy outcome was clarified.12-14 Those with a prior SPTB had a 2.5-fold
increase in the risk of a SPTB (21.7% v 8.8%).
The earlier the prior SPTB, the earlier the SPTB
in the current pregnancy. For example, a prior
SPTB was associated with more than a 10-fold
increased risk of having a less than 28-week
spontaneous birth in the current pregnancy.
Those women who had a 23- to 28-week SPTB in
the prior pregnancy had a 22-fold increase in the
risk of repeating the outcome in a subsequent
pregnancy. However, the associations were considerably weaker for those women who had a 13
to 22 week loss in the prior pregnancy. Prior
SPTB preceded by preterm premature rupture
of the membranes was significantly associated
with similar outcomes in the current pregnancy.
The Preterm Prediction Study considered several genital tract infections in relationship to
SPTB.15,16 BV, which was found in approximately
20% of the population, was significantly associ-
188
Goldenberg et al
ated with SPTB at 28 weeks’, (OR 1.8) but not at
24 weeks’ (OR 1.4). The strongest association
was found in those women who acquired BV
between the 24th and the 28th week. If BV was
present at either time, the strongest association
was with early (less than 32-week SPTB) rather
than later SPTB. These results are somewhat
different than other studies in which women
who had BV earlier in their pregnancy had
higher rates of SPTB. The reasons for the differences remain unexplained. Nevertheless, this
study did confirm the association between BV
and SPTB. This study also confirmed previous
reports which demonstrated that BV was more
common in black than white woman.10 Because
of the 2-fold increase in prevalence and the
nearly 2-fold increase in risk, somewhere between 30% and 50% of the attributable risk of
SPTB in black women may be due to BV.
In the Preterm Prediction Study, candida was
present in about 20% of the pregnancies and
trichomonas in about 3%.15 Neither infection
was associated with SPTB. However, women with
a history of pelvic infection were at greater risk
of SPTB than other women. By using a urine
ligase chain reaction methodology, women with
a chlamydia infection were twice as likely to have
a SPTB than women without this infection.16
Interestingly, women positive for chlamydia
were more likely to have a short cervix by ultrasound, and also were less likely to have a positive
FFN test. These results suggest that chlamydia
might act locally on the cervix rather than acting
inside the uterus, disrupting the extracellular
matrix and releasing FFN, as do infections such
as ureaplasma or mycoplasma.
As in previous studies, maternal thinness, as
defined by a body mass index of less than 19.8
kg/M,2 was associated with SPTB.10 Whether the
outcome was SPTB less than 32 weeks, less than
35 weeks, or less than 37 weeks, the thinner the
woman, the greater the risk of SPTB. Overall,
the thinnest women had a 2.5- to 3.0-fold increased risk of SPTB. The relationship between
thinness and SPTB was stronger in white compared to black women.10
We also examined the relationship between a
number of psychosocial characteristics and
SPTB.17 Of these characteristics, which include
measurements of anxiety, self-esteem, and depression, only perceived stress was associated
with SPTB, and then only weakly (OR 1.3).
At 24 weeks’, we asked questions about the
presence of uterine contractions and their frequency, and about vaginal bleeding.10 The presence of either condition was associated with subsequent SPTB, both with odds ratios around 2. A
history of uterine contractions was associated
with SPTB with an odds ratio of about 2 at all
gestational ages, while a history of bleeding prior
to 24 weeks’ was more strongly associated with
SPTB ⬍ 32 weeks’ (OR 2.7) than with SPTB ⬍
37 weeks’ (OR 1.5).
One of the major purposes for conducting
the Preterm Prediction Study was to understand
the value of FFN in predicting SPTB in a relatively low risk population undergoing routine
prenatal care and without signs of early labor.
To that end, we obtained FFN samples from
both the cervix and vagina every 2 weeks from 24
to 30 weeks’ gestational age. First, we learned
that, by using the conventional cut-off of 50
ng/mL, about 3% to 4% of the samples were
FFN positive.18 Over the gestational age range
tested, the rate of positive tests did not vary by
gestational age. However, in a related study, the
rates of positive FFN tests were higher between
13 and 22 weeks’.19 From 24 to 30 weeks, the
cervical test was a slightly better predictor of
SPTB than vaginal tests.18 Also, within the 24- to
30-week period, the earlier the test was performed, the stronger was the association with
SPTB. Tests performed at 24 and 26 weeks’, for
example, were considerably stronger predictors
of SPTB than were those performed at 28 and 30
weeks. FFN was also considerably better at predicting early SPTB (⬍28 weeks), than later
SPTB. For example, when performed at 24
weeks’, a positive FFN test was associated with a
sensitivity of 63% and an odds ratio of 60 for
predicting SPTB occurring from 24 to 28 weeks’
gestation.18 From the related study, FFN tests
performed prior to 22 weeks’ were much poorer
predictors of SPTB.19
We also learned that for women remaining
undelivered after a positive FFN test, subsequent
tests generally became negative.20 For example,
if the index FFN test result was positive, and the
women remained undelivered, only 29% of the
subsequent FFN tests were positive. There was
better concordance (79%) between cervical and
vaginal tests performed concurrently. Also, if
several tests were performed in a given window,
the greater the percent of tests that were posi-
Predictors of Preterm Birth
tive, the more likely that a subsequent preterm
delivery would occur.21 Increasing quantitative
FFN values in the cervix and vagina were also
associated with increasing risk of SPTB. For example as the FFN values increased from 20-40
ng/mL to 60-90 ng/mL to values as high as
150-300 ng/mL, the relative risk of SPTB approximately doubled with each increase of
FFN.22 In a related study, similar results were
seen in women entering the hospital with symptoms of preterm labor.23 The higher the FFN
value, the more likely they were to deliver prematurely.
One of the most intriguing findings in the
preterm prediction study was the relationship
between an elevated FFN and subsequent perinatal infection.24 When the FFN test was positive
at 24 weeks’, the risk of subsequent clinical chorioamnionitis increased 15- to 20-fold and the
risk of confirmed neonatal sepsis increased
6-fold. Virtually every woman with a positive FFN
who delivered preterm had histological chorioamnionitis. The mean time interval between the
positive FFN test and the perinatal infections
described above was 7 weeks.
After FFN, a short cervical length defined by
ultrasound was the strongest predictor of
SPTB.25 From the Preterm Prediction Study, we
confirmed previous findings26 that the relationship between cervical length and SPTB follows a
linear rather than threshold pattern. Over the
entire range of measurements, the shorter the
cervix the greater was the risk of SPTB. Nevertheless, a standard cutoff to define a short cervix
is useful, and for the Preterm Prediction Study,
the 10th percentile or a cervical length of 25 mm
was used to define a short cervix. Women with a
cervix of 25 mm or less had about a 6-fold increase in SPTB, with the association even stronger if shorter cervical lengths were chosen as the
cutoff. In contrast to fluctuations in the FFN
tests, on sequential measurements, women who
had a short cervix on the first examination generally had a short cervix on subsequent examinations.20
We compared the strength of the individual
predictors described above against one another.
For nearly all definitions of SPTB, a positive FFN
test was the strongest predictor of SPTB, followed by a short cervix and then by a prior
history of SPTB.10 Because short cervical length
and a positive FFN test were the strongest pre-
189
dictors, we asked which of these 2 factors turned
positive first, to determine if we could learn
something about the pathway leading to SPTB.20
For example, if the cervix usually shorted prior
to the FFN test becoming positive, certain hypotheses relating to the pathway leading to
SPTB would seem more logical than others.
However, while a short cervix and a positive test
tended to occur in the same women,10 either
factor could appear first followed by the appearance of the other.20 Therefore, there was no
consistent pathway leading to SPTB. Other persistent correlations between risk factors leading
to SPTB included the significant relationship
between black race and both BV and pelvic infections.10 Also, women with a prior SPTB were
more likely to have a short cervix in the current
pregnancy.
Using a case-control design, we evaluated
nearly 30 potential biologic predictors found in
serum, urine and cervical and vaginal fluids.27-29
Of these, with the exception of fetal fibronectin
and a short cervix, the strongest and most consistent associations with SPTB at less than 32
(Table 1) and less than 35 weeks (Table 2) were
found in serum, with ␣-fetoprotein and alkaline
phosphatase strongly associated with SPTB.27-29
A granulocyte colony stimulating factor value
above the 75th percentile was a strong predictor
of SPTB ⬍32 weeks [OR 12.7 (28-565)] and
at ⬍35 weeks [OR 3.1 (1.4-6.9),] but similar
results were not found using the 90th percentile.
Interestingly, although significantly associated
with SPTB in some analyses, corticotropin releasing factor was not nearly as good a predictor as
either alpha fetoprotein or alkaline phosphatase.29 Markers found in cervical and vaginal
fluids associated with SPTB,30 in addition to
FFN, included ferritin,31 interleukin 6,32 alpha
fetoprotein,33 prolactin,34 and a marker of collagen synthesis.35
Because there was generally little overlap
among the positive tests, we next questioned
whether using several tests together would increase the predictive values over any single test.
In other words, we hoped to develop a “multiple
marker test” for SPTB.27 Therefore, in a series of
analyses, we compared individual tests of FFN,
cervical length, serum alpha-fetoprotein, alkaline phosphatase, and granulocyte colony stimulating factor against various combinations of
tests.27 No specific grouping clearly outshown
190
Goldenberg et al
Table 1. Risk Factors and Tests for Spontaneous Preterm Birth ⬍32 Weeks Obtained or Available at 24
Weeks’ Gestational Age in Cases and Controls
Factor
Corticotropin
releasing factor
Alpha fetoprotein
Alkaline
Phosphatase
Beta2-macroglobulin
Ferritin
Interstitial cell
adhesion
molecule-1
Interleukin-6
C-reactive protein
Cortisol
Lactoferrin
Defensins
Relaxin
Interleukin-10
Granulocyte colony
stimulating factor
Activan
Interleukin-6
Lactoferrin
Defensins
Sialidase
Short cervix
Fetal fibronectin
Gram stain score
PH
Chlamydia
Previous SPTB
Contractions
Bleeding
Body mass index
Source of
Data or Fluid
Test
Cutoff
n ⫽ 48
Cases %
Positive
n ⫽ 48
Controls %
Positive
OR Cases
v Controls
Significant
(P ⬍ .05)
Serum
Serum
90th %ile
90th %ile
10.6
36.1
4.3
6.4
2.7
8.3
No
Yes
Serum
Serum
Serum
90th %ile
90th %ile
90th %ile
22.9
6.3
14.6
4.2
2.1
2.1
6.8
3.1
8.0
Yes
No
No
Serum
Serum
Serum
Serum
Serum
Serum
Serum
Serum
90th
90th
90th
90th
90th
90th
90th
90th
23.4
10.4
10.4
10.4
11.6
20.9
10.9
6.4
6.4
8.3
6.3
2.1
9.3
4.7
10.9
12.8
4.5
1.3
1.7
5.5
1.3
5.4
1.0
0.5
Yes
No
No
No
No
Yes
No
No
Serum
Serum
Cervix
Cervix
Cervix
Cervix
Ultrasound
Cervix/Vagina
Vagina
Vagina
Vagina
History
History
History
Measured
90th %ile
Pos
90th %ile
90th %ile
90th %ile
90th %ile
⬍25mm
ⱖ50 ng/mL
ⱖ9
ⱖ5.0
Pos
Pos
Pos
Pos
⬍19.8
8.5
8.5
20.4
4.3
10.5
8.2
44.9
40.0
30.0
42.9
15.2
42.0
24.0
36.0
29.2
10.6
10.6
6.1
0.0
18.4
6.1
12.2
2.0
24.0
18.4
6.5
14.0
32.0
24.0
14.6
0.8
0.8
3.9
Inf
0.5
1.4
5.8
32.7
1.4
3.3
2.6
4.5
0.7
1.8
2.4
No
No
Yes
No
No
No
Yes
Yes
No
Yes
No
Yes
No
No
No
%ile
%ile
%ile
%ile
%ile
%ile
%ile
%ile
the others, but the use of the 3 serum tests,
requiring 1 or 2 to be positive had reasonable
promise. Clearly, further work needs to be conducted before any “multiple marker test” for
SPTB is ready for clinical use.
To date, we have not studied the twins as
extensively as we have the singleton pregnancies.36 The smaller number of cases has also
limited our ability to make statements as to the
weaker predictors of SPTB in twins. Nevertheless, certain comments can be made. The most
important is that of twin pregnancy is one of the
strongest predictors of SPTB yet described.
Nearly 35% of twin pregnancies deliver spontaneously prior to 35 weeks’ and nearly half by 37
weeks. In women with twins, however, the stron-
gest risk factors, FFN and short cervical length
remain potent predictors of SPTB.36
Finally, we examined risk factors for indicated
preterm births.37 Overall, of the 15.4% of all
births which were delivered at ⬍ 37 weeks’,
27.7% were indicated preterm births. Risk factors in the final multivariable model were, in
order of decreasing odds ratios, müllerian duct
abnormality (odds ratio 7.02), proteinuria at
⬍24 weeks’ gestation (odds ratio 5.85), history
of chronic hypertension (odds ratio 4.06), history of previous indicated preterm birth (odds
ratio 2.79), history of lung disease (odds ratio
2.52), previous spontaneous preterm birth
(odds ratio 2.45), age ⬎30 years (odds ratio
2.42), black ethnicity (odds ratio 1.56), and
191
Predictors of Preterm Birth
Table 2. Risk Factors and Tests for Spontaneous Preterm Birth ⬍35 Weeks Obtained or Available at 24
Weeks’ Gestational Age in Cases and Controls
Factor
Corticotropin
releasing factor
Alpha fetoprotein
Alkaline
phosphatase
Beta2-macroglobulin
Ferritin
Interstitial cell
adhesion
molecule-1
Interleukin-6
C-reactive protein
Cortisol
Lactoferrin
Defensins
Relaxin
Interleukin-10
Granulocyte colony
stimulating factor
Activan
Interleukin-6
Lactoferrin
Defensins
Sialidase
Short cervix
Fetal fibronectin
Gram stain score
PH
Chlamydia
Previous SPB
Contractions
Bleeding
Body mass index
Source of
Data or Fluid
Test
Cutoff
n ⫽ 107
% Positive
Cases
n ⫽ 107
% Positive
Controls
OR Cases
V Controls
Significant
(P ⬍ .05)
Serum
Serum
90th %ile
90th %ile
11.7
35.3
8.3
13.5
1.5
3.5
No
Yes
Serum
Serum
Serum
90th %ile
90th %ile
90th %ile
14.9
5.1
9.9
3.3
6.8
7.4
5.1
0.7
1.4
Yes
No
No
Serum
Serum
Serum
Serum
Serum
Serum
Serum
Serum
90th
90th
90th
90th
90th
90th
90th
90th
16.4
10.0
8.3
12.6
8.8
18.4
13.6
4.3
9.1
9.2
6.7
7.6
11.4
10.5
8.2
10.3
2.0
1.1
1.3
1.8
0.8
1.9
1.8
0.4
No
No
No
No
No
No
No
No
Serum
Serum
Cervix
Cervix
Cervix
Cervix
Ultrasound
Cervix/vagina
Vagina
Vagina
Vagina
History
History
History
Measured
90th %ile
Pos
90th %ile
90th %ile
90th %ile
90th %ile
ⱕ25 mm
ⱖ50 ng/mL
ⱖ9
⬎5
Pos
Pos
Pos
Pos
⬍19.8
7.7
14.2
20.0
5.0
16.7
9.6
36.8
22.8
22.8
38.1
12.8
43.3
31.5
35.4
30.9
7.7
11.7
9.6
0.0
10.0
9.6
9.6
3.2
15.0
21.4
5.1
15.0
31.5
20.5
17.9
1.0
1.3
2.4
Inf
1.8
1.0
5.5
9.1
1.7
2.3
2.7
4.3
1.0
2.1
2.1
No
No
No
Yes
No
No
Yes
Yes
No
Yes
Yes
Yes
No
Yes
Yes
%ile
%ile
%ile
%ile
%ile
%ile
%ile
%ile
working during pregnancy (odds ratio 1.49). Alcohol use in pregnancy was actually associated
with a lower risk of indicated preterm birth
(odds ratio 0.35).
Discussion
Being able to predict which women are likely to
have a preterm birth is a prerequisite for the
effective use of most interventions aimed at preventing preterm birth.38 Without this ability, we
will be forced to apply potential interventions to
large numbers of pregnant women, the vast majority of whom are destined to deliver at term
without any interventions. More specific knowledge about which risk factors predict SPTB also
might be helpful as we design our interventions.
For example, while tocolytic agents might be
useful in women whose predominant risk factor
is the presence of contractions, tocolytics may be
less useful where risk factors suggest the presence of an intrauterine infection. Placement of a
cerclage might be useful if the risk factor is a
short cervix, but this intervention will likely not
be effective if the risk factors suggest an infection or contractions. Therefore, simply knowing
someone is at a high- risk from a demographic
survey or from previous pregnancy history may
turn out to be less useful than if we know why a
pregnant woman is high-risk and can use this
information to select an appropriate intervention.
From the Preterm Prediction Study, we have
confirmed that there are a number of factors
192
Goldenberg et al
strongly related to preterm birth. These include
the history of a previous preterm birth, especially an early one, the presence of cervical or
vaginal FFN, especially at 24-26 weeks’, and the
presence of a short cervix. Bacterial vaginosis is
a much weaker predictor, but its presence early
in gestation and its potential elimination by antibiotic treatment, make it an interesting risk
factor to study further
The confirmation that a low body mass index,
or maternal thinness, is a relatively strong risk
factor for SPTB raises issues related to the mechanism of association, and potential treatment.
Some recent data, which suggest that this association may be mediated by micronutrient depletion resulting in failure to expand plasma
volume, opens several lines of research and also
suggests some potential interventions.39-41 For a
short cervix, generally the second strongest predictor of SPTB, one potential intervention suggests itself. In fact, 2 small trials of a cervical
cerclage in women with a short cervix have already been published, although with conflicting
results.42,43 A much larger trial is currently underway.
For the strongest predictor of SPTB, a positive
FFN test at 24-26 weeks, no clearly specific intervention has presented itself, other than antibiotics to treat the associated intrauterine infection.
Unfortunately, in a large randomized trial conducted in FFN positive women, antibiotic treatment was not effective in reducing SPTB.44
Therefore, at present it is not clear how to use
the information gained from FFN testing of
asymptomatic women to reduce SPTB. The situation is different for testing symptomatic
women, those presenting in the hospital with
contractions and cervical change. In these
women, a negative test strongly suggests that the
woman will not deliver within the next week or
2, and generally can be sent home without undue concern. Since only 20% or so of symptomatic women with a positive test deliver in the next
2 weeks or so, how to treat those women is less
clear.
In summary, the Preterm Prediction Study
has clearly demonstrated that it is possible to
predict SPTB using a variety of demographic,
behavioral, historical, and biophysical risk factors as well as tests of biological fluids. Among
these tests, FFN and a short cervix are generally
the strongest predictors, although in the case-
control study, serum markers such as alpha fetoprotein and alkaline phosphatase have similar
predictive value. Predicting SPTB, however, is
only an intermediate goal. Without an effective
intervention linked to the factor(s) that predict
SPTB, we will not be able to reduce SPTB and
the associated adverse outcomes. Defining the
appropriate interventions that can be linked to
the predictors defined above is the next order of
business.
References
1. McCormick MC: The contribution of low birth weight to
infant mortality and childhood morbidity. N Engl J Med
312:82-90, 1985
2. Goldenberg RL, Rouse DJ: The prevention of premature
birth. N Engl J Med 339:313-320, 1998
3. Creasy RK, Gummer BA, Liggins GC: System for predicting spontaneous preterm birth. Obstet Gynecol 55:692695, 1980
4. Copper RL, Goldenberg RL, DuBard MB, et al: Cervical
examination and tocodynamometry at 28 weeks’ gestation: Prediction of spontaneous preterm birth. Am J
Obstet Gynecol 172:666-671, 1995
5. Andersen HF, Nugent CE, Wanty SD, et al: Prediction of
risk for preterm delivery by ultrasonographic measurement of cervical length. Am J Obstet Gynecol 163:859867, 1990
6. Moore TR, Iams JD, Creasy RK, et al: Diurnal and gestational patterns of uterine activity in normal human
pregnancy. Obstet Gynecol 83:517-523, 1994
7. Gravett MG, Nelson HP, DeRouen T, et al: Independent
associations of bacterial vaginosis and chlamydia trachomatis infection with adverse pregnancy outcome. JAMA
256:1899-1903, 1986
8. Nageotte MP, Casal D, Senyei AE: Fetal fibronectin in
patients at increased risk for premature birth. Am J
Obstet Gynecol 170:20-25, 1994
9. Lockwood CJ, Senyei AE, Dische MR, et al: Fetal fibronectin in cervical and vaginal secretions as a predictor of preterm delivery. N Engl J Med 325:669-674, 1991
10. Goldenberg RL, Iams JD, Mercer BM, et al: The Preterm
Prediction Study: The value of new vs standard risk
factors in predicting early and spontaneous preterm
birth. Am J Public Health 88:233-238, 1998
11. Kramer MS: Determinants of low birth weight: Methodological assessment and meta-analysis. Bull World
Health Organ 65:663-737, 1987
12. Mercer BM, Goldenberg RL, Moawad AH, et al: The
Preterm Prediction Study: effect of gestational age and
cause or preterm birth on subsequent obstetric outcome. Am J Obstet Gynecol 181:1216-1221, 1999
13. Iams JD, Goldenberg RL, Mercer BM, et al: The Preterm
Prediction Study: Recurrence risk of spontaneous preterm birth. Am J Obstet Gynecol 178:1035-1040, 1998
14. Mercer BM, Goldenberg RL, Meis PJ, et al: The Preterm
Prediction Study: Prediction of preterm premature rup-
Predictors of Preterm Birth
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
ture of membranes through clinical findings and ancillary testing. Am J Obstet Gynecol 183:738-745, 2000
Meis PJ, Goldenberg RL, Mercer B, et al: The Preterm
Prediction Study: Significance of vaginal infections. Am J
Obstet Gynecol 173:1231-1235, 1995
Andrews WW, Goldenberg RL, Mercer B, et al: The
Preterm Prediction Study: association of mid-trimester
genital chlamydia infection and subsequent spontaneous preterm birth. Am J Obstet Gynecol 183:662-668,
2000
Copper RL, Goldenberg RL, Das A, et al: The Preterm
Prediction Study: maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks’ gestation. Am J Obstet Gynecol 175:1286-1292, 1996
Goldenberg RL, Mercer BM, Meis PJ, et al: The Preterm
Prediction Study: Fetal fibronectin testing and spontaneous preterm birth. Obstet Gynecol 87:643-648, 1996
Goldenberg RL, Klebanoff M, Carey JC, et al: Vaginal
fetal fibronectin measurements from 8 to 22 weeks’
gestation and subsequent spontaneous preterm birth.
Am J Obstet Gynecol 183:469-475, 2000
Goldenberg RL, Iams JD, Das A, et al: The Preterm
Prediction Study: Sequential cervical length and fetal
fibronectin testing for the prediction of spontaneous
preterm birth. Am J Obstet Gynecol 182:636-643, 2000
Goldenberg RL, Mercer BM, Iams JD, et al: The Preterm
Prediction Study: patterns of cervicovaginal fetal fibronectin as predictors of spontaneous preterm delivery. Am J Obstet Gynecol 177:8-12, 1997
Goepfert AR, Goldenberg RL, Mercer B, et al: The Preterm Prediction Study: Quantitative fetal fibronectin values and the prediction of spontaneous preterm birth.
Am J Obstet Gynecol 183:1480-1483, 2000
Lu GC, Goldenberg RL, Cliver SP, et al: Vaginal fetal
fibronectin levels and spontaneous preterm birth in
symptomatic women. Obstet Gynecol 97:225-228, 2001
Goldenberg RL, Thom E, Moawad AH, et al: The Preterm Prediction Study: Fetal fibronectin, bacterial vaginosis and peripartum infection. Obstet Gynecol 87:656660, 1996
Iams JD, Goldenberg RL, Meis PJ, et al: The length of
the cervix and the risk of spontaneous premature delivery. N Engl J Med 334:567-572, 1996
Iams JD, Johnson FF, Sonek J, et al: Cervical competence
as a continuum: A study of ultrasonographic cervical
length and obstetric performance. Am J Obstet Gynecol
172:1097-1106, 1995
Goldenberg RL, Iams JD, Mercer BM, et al: The Preterm
Prediction Study: Toward a multiple-marker test for
spontaneous preterm birth. Am J Obstet Gynecol 185:
643-651, 2001
Goldenberg RL, Andrews WW, Mercer BM, et al: Granulocyte colony stimulating factor and spontaneous preterm birth. Am J Obstet Gynecol 182:625-630, 2000
Moawad AH, Goldenberg RL, Mercer B, et al: The Preterm Prediction Study: the value of serum alkaline phosphatase, ␣ fetoprotein, plasma corticotropin-releasing
hormone, and other serum markers for the prediction
of spontaneous preterm birth. Am J Obstet Gynecol
186:990-996, 2002
193
30. Ramsey PS for the NICHD MFMU Network: Cervical
markers at 22-24 weeks’ gestation improve the prediction of subsequent spontaneous preterm birth. J Soc
Gynecol Investig 8:64A, 2001 (abstr)
31. Ramsey PS, Tamura T, Goldenberg RL, et al: The Preterm Prediction Study: elevated cervical ferritin levels at
22 to 24 weeks of gestation are associated with spontaneous preterm delivery in asymptomatic women. Am J
Obstet Gynecol 183:458-463, 2002
32. Ramsey PS, Boots L, Goldenberg RL for the NICHD
MFMU Network: The Preterm Prediction Study: cervical
alpha-fetoprotein levels and spontaneous preterm birth
in asymptomatic women. Am J Obstet Gynecol 184:S6,
2001 (abstr)
34. Ramsey PS, Shinetugs B, Goldenberg RL: The Preterm
Prediction Study: Elevated vaginal prolactin levels at
22-24 weeks gestation are associated with spontaneous
preterm delivery in asymptomatic women. Am J Obstet
Gynecol 185:S146(abstr), 2001
35. Ramsey PS, Shinetugs B, Goldenberg for the NICHD
MFMU Network: The Preterm Prediction Study. Increased vaginal levels of a marker of collagen synthesis
are associated with spontaneous preterm birth and preterm premature rupture of membranes in asymptomatic
women. Am J Obstet Gynecol 185:S146, 2002 (abstr)
36. Goldenberg RL, Iams JD, Miodovnik M, et al: The Preterm Prediction Study: risk factors in twin gestations.
Am J Obstet Gynecol 175:1047-1053, 1996
37. Meis PJ, Goldenberg RL, Mercer BM, et al: The Preterm
Prediction Study: Risk factors for indicated preterm
births. Am J Obstet Gynecol 178:562-567, 1998
38. Goldenberg RL, Andrews WW, Hauth JC: Markers of
preterm birth. Prenat Neonat Med 3:43-46, 1998
39. Rosso P, Donoso E, Braun S, et al: Hemodynamic
changes in underweight pregnant women. Obstet Gynecol 79:908-912, 1992
40. Mardones-Santander F: Nutritional intervention to prevent intrauterine growth retardation: Evidence from
randomized controlled trials. Eur J Clin Nutr 53:970971(letter), 1999
41. Rao S, Yajnik CS, Kanade A, Fall CHD, et al: Intake of
micronutrient-rich foods in rural Indian mothers is associated with size of their babies at birth: Pune maternal
nutrition study. J Nutr 21:1217-1224, 2001
42. Althuisius SM, Dekker GA, van Geijn HP, et al: Cervical
incompetence prevention randomized cerclage trial (CIPRACT): Study design and preliminary results. Am J
Obstet Gynecol 183:823-828, 2000
43. Rust OA, Atlas RO, Jones KJ, et al: A randomized trial of
cerclage versus no cerclage among patients with ultrasonographically detected second-trimester preterm dilatation of the internal os. Am J Obstet Gynecol 183:830835, 2000
44. Andrews WW for the NICHD MFMU Network: Randomized clinical trial of metronidazole plus erythromycin to
prevent spontaneous preterm delivery in fetal fibronectin positive women. J Soc Gynecol Investig 8:47A, 2001
(abstr)