Journal of Perinatology (2006) 26, 3–10
r 2006 Nature Publishing Group All rights reserved. 0743-8346/06 $30
www.nature.com/jp
ORIGINAL ARTICLE
Neonatal mortality and morbidity in vertex–vertex second twins
according to mode of delivery and birth weight
Q Yang1,2,3, SW Wen1,2,4, Y Chen4, D Krewski3,4, K Fung Kee Fung1 and M Walker1,2
1
OMNI Research Group, Department of Obstetrics and Gynecology, Faculty of Medicine, University of Ottawa, Ottawa, Canada;
Ottawa Health Research Institute, Ottawa, Canada; 3McLaughlin Centre for Population Health Risk Assessment, Institute of
Population Health, University of Ottawa, Ottawa, Ontario, Canada and 4Department of Epidemiology and Community Medicine,
University of Ottawa, Ottawa, Ontario, Canada
2
Introduction
Over the last two decades, industrialized countries have witnessed
dramatic increases in the incidence of twins, due in part to the
delayed pregnancy and in part to increased use of assisted
reproductive technology.1 Perinatal mortality and morbidity are
4–6-fold higher in twins than in singletons.2 There are several
contributing factors for the increased risk of adverse neonatal
outcomes in twins; one such factor is the mode of delivery,
especially for the second-born twins.3–6 There are three modes of
delivery options for twins: delivery by cesarean section after
cesarean delivery of first twin, delivery vaginally after vaginal
delivery of first twin, and delivery by cesarean section after vaginal
delivery of the first twin. This third mode of delivery occurs in
about 9.5% of second twins after vaginal delivery of the first twin.7
The second twins with emergency cesarean delivery had worst
neonatal outcomes compared with the second twins with both twins
delivered vaginally or both twins delivered by cesarean section.5,6
However, in these studies, we did not examine neonatal outcomes
according to the presentation of the twins.
Vertex for both twins is the most common presentation, occurring
from 38.4 to 47.5% of twin births.8–14 There is a general consensus
that vaginal delivery for twins is safe when both are vertex
presenting.15,16 However, it should be noted that this consensus is not
drawn on results from randomized clinical trials, but based on expert
opinion. It has also been suggested that the method of delivery for
vertex–vertex twins should be based on the infant’s birth weight. For
example, authors have recommended that a planned cesarean
delivery should be considered for infants with a birth weight <1500 g,
whereas a trial of labor should be allowed for infants with a birth
weight in the range 1500–4000 g.17,18 Again, these recommendations
have been based on the expert opinion rather than the results from
randomized controlled trials or observational studies.
The objective of this study is to compare the neonatal outcomes
in the vertex–vertex second twins according to mode of delivery,
both in overall population and after stratifying the infants
according to their birth weight: those with a birth weight
of <1500 g, 1500–2499 g, and X2500 g.
Correspondence: Dr Q Yang, OMNI Research Group, Department of Obstetrics & Gynecology,
The Ottawa Hospital, General Campus, 501 Smyth Road, Box 241, Ottawa, Canada K1H 8L6.
E-mail: qyang@ohri.ca
Received 17 February 2005; revised 18 July 2005; accepted 24 August 2005; published online
24 November 2005
Methods
We carried out a population-based retrospective cohort study of all
twin births in the US for the period of 1995–1997, using the
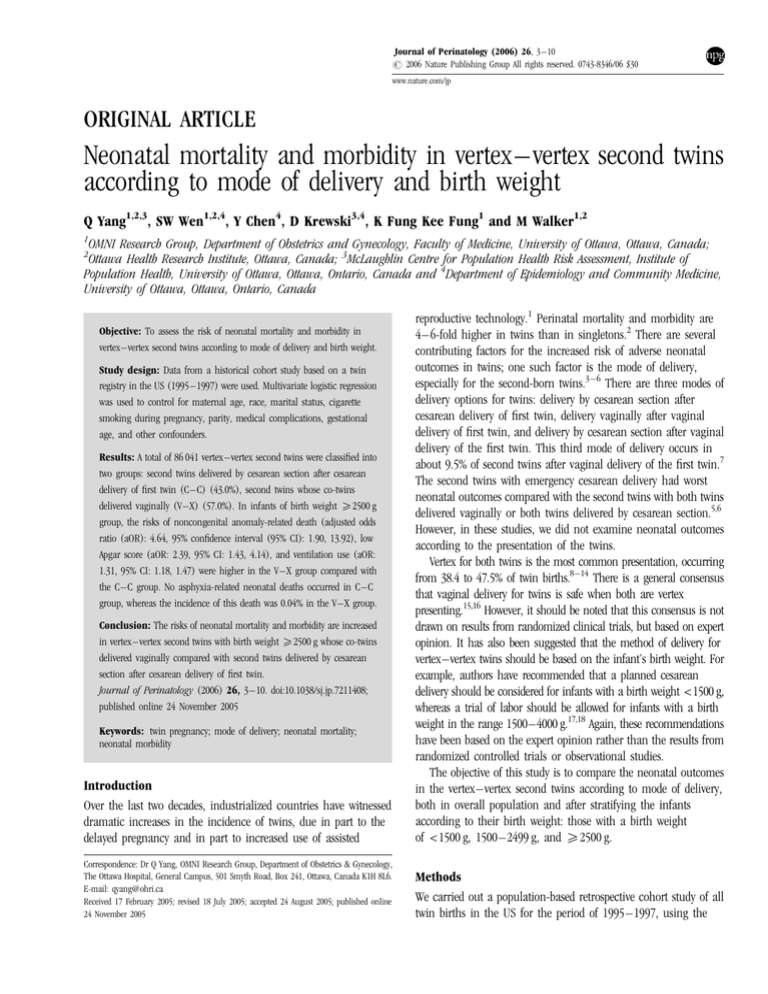
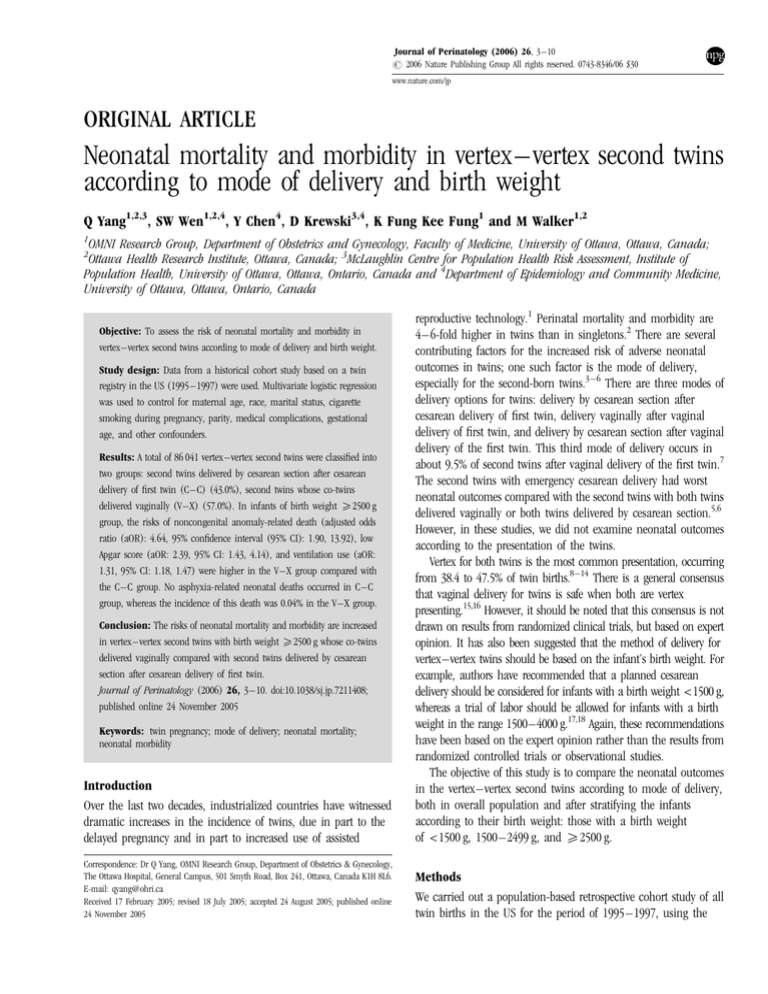
Objective: To assess the risk of neonatal mortality and morbidity in
vertex–vertex second twins according to mode of delivery and birth weight.
Study design: Data from a historical cohort study based on a twin
registry in the US (1995–1997) were used. Multivariate logistic regression
was used to control for maternal age, race, marital status, cigarette
smoking during pregnancy, parity, medical complications, gestational
age, and other confounders.
Results: A total of 86 041 vertex–vertex second twins were classified into
two groups: second twins delivered by cesarean section after cesarean
delivery of first twin (C–C) (43.0%), second twins whose co-twins
delivered vaginally (V–X) (57.0%). In infants of birth weight X2500 g
group, the risks of noncongenital anomaly-related death (adjusted odds
ratio (aOR): 4.64, 95% confidence interval (95% CI): 1.90, 13.92), low
Apgar score (aOR: 2.39, 95% CI: 1.43, 4.14), and ventilation use (aOR:
1.31, 95% CI: 1.18, 1.47) were higher in the V–X group compared with
the C–C group. No asphyxia-related neonatal deaths occurred in C–C
group, whereas the incidence of this death was 0.04% in the V–X group.
Conclusion: The risks of neonatal mortality and morbidity are increased
in vertex–vertex second twins with birth weight X2500 g whose co-twins
delivered vaginally compared with second twins delivered by cesarean
section after cesarean delivery of first twin.
Journal of Perinatology (2006) 26, 3–10. doi:10.1038/sj.jp.7211408;
published online 24 November 2005
Keywords: twin pregnancy; mode of delivery; neonatal mortality;
neonatal morbidity
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
4
Matched Multiple Birth File created by the Centers for Disease
Control and Prevention.19 The matching was successful for 98.8%
of twin birth sets.19 Only live births were included in this study.
Live births with gestational age less than 24 weeks or with birth
weight less than 500 g were excluded because these newborn’s
viability can be questionable.
We restricted our study to vertex–vertex second twins. The study
subjects were divided into two groups by mode of delivery: delivery
by cesarean section after cesarean delivery of first twin (C-C),
and all second twins after vaginal delivery of first twin (V–X).
We further divided second group into two subgroups: vaginal
delivery (V–V) and cesarean delivery (V–C). We derived a new
variable, which was birth-weight discordance within the pair of
twins (second twin 25% smaller or 25% larger than the first
twin).
Main study outcomes of interest included neonatal mortality
and morbidity. Neonatal death was defined as live born infant
who died within 28 days of life. To test the hypothesis that the
association between mode of delivery and neonatal mortality would
be stronger in those deaths not caused by lethal congenital
anomaly and those caused by asphyxia, we compared the rates of
noncongenital anomaly-related and asphyxia-related neonatal
mortality among these groups. For noncongenital anomaly-related
neonatal mortality, we excluded deaths with cause of death being
congenital anomaly. The grouping for noncongenital anomaly- or
asphyxia-related neonatal deaths were according to the
International Collaborative Effort on Infant Mortality,20 and the
standard National Center for Health Statistics categories. Neonatal
morbidity examined in this study included lower 5-min Apgar score
(p3), the need for mechanical ventilation, and the occurrence of
seizure.
We first compared the distribution of maternal and infant
characteristics of the three study groups. We then estimated the
crude odds ratios (ORs) and adjusted odds ratios (aORs) for mode
of delivery using unconditional logistic regression with C-C group
as the reference. Potential confounding variables included
maternal age (<20, 20–29, 30–34, and X35 years), race (white,
not white), marital status (yes, no), cigarette smoking during
pregnancy (yes, no, not stated), parity (0, 1 þ ), one of these
complications (diabetes, pregnancy-associated hypertension,
eclampsia, abruption placenta, and placenta previa) (yes, no), one
of abnormal conditions during labor (precipitous labor, prolonged
labor, dysfunctional labor, cephalopelvic disproportion, cord
prolapse, and fetal distress) (yes, no), birth-weight discordance
(second twin 25% larger, second twin 25% smaller, remaining),
fetal gender (female, male), and gestational age (24–27 weeks,
28–31 weeks, and X32 weeks in the birth weight <1500 g group,
24–35 weeks and X36 weeks both in birth weight 1500–2499,
and X2500 g groups). All analyses were performed using SAS-PC
statistical software version 8 (SAS Inc., NC).
Results
There were 95 977 vertex–vertex second twins in the database. We
excluded 9936 second twins (fetal death (1479), gestational age
<24 completed weeks (1381), birth weight <500 g (283), and
missing information on delivery (6793)), leaving 86 041 eligible
vertex–vertex second twins for analysis. Among them, 36 977
(43.0%) were in the C–C group, 46 071 (53.5%) in the V–V group,
and 2993 (3.5%) in the V–C group. The rate of emergency
cesarean delivery for the second twin after vaginal delivery of the
first twin was 6.1% in all vertex–vertex second twins, 11.3% in
birth weight <1500 g, 5.8% in birth weight 1500–2499 g, and 5.7%
in birth weight X2500 g.
Table 1 displays the distribution of maternal and infant
characteristics among the three study groups. The proportions of
non-white race, unmarried, high parity, and late prenatal care
initiation were higher in the V–C group than the C–C group
(Table 1). The differences in maternal and fetal characteristics
between the V–V group and the C–C group tended to be smaller.
Table 1 Maternal and fetal characteristics for the vertex–vertex second twins according to mode of delivery, US, 1995–1997
Characteristics
C–C group
Number
V–V group
V–C group
Percent
Number
Percent
Number
Percent
Maternal age (years)
<20
20–29
30–34
X35
2463
16 185
11 024
7305
6.7
43.8
29.8
19.7
3658
22 235
13 003
7175
7.9
48.3
28.2
15.6
230
1448
825
490
7.7
48.4
27.5
16.4
Maternal race
White
Non-white
29 220
7757
79.0
21.0
36 839
9232
80.0
20.0
2143
850
71.6
27.4
Journal of Perinatology
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
5
Table 1 Continued
Characteristics
C–C group
Number
V–V group
V–C group
Percent
Number
Percent
Number
Percent
Marital status
Married
Others
27 431
9546
74.2
25.8
33 353
12 718
72.4
27.6
1990
1003
66.5
33.5
Education
<12 years
12 years
13–15 years
X16 years
5624
11 389
8700
10 891
15.4
31.1
23.8
29.7
7211
14 253
10 586
13 499
15.8
31.3
23.2
29.7
544
954
657
809
18.3
32.2
22.2
27.3
Smokinga
No
Yes
Unavailable
2958
25 222
8797
8.0
68.2
23.8
4083
32 926
9062
8.9
71.4
19.7
308
2101
584
10.3
70.2
19.5
Parity
0
1+
16 496
20 462
44.6
55.4
18 105
27 936
39.3
60.7
1043
1949
34.9
65.1
Prenatal care initiation
First trimester
Second trimester
Third trimester or None
31 409
3862
747
87.2
10.7
2.1
38 691
5048
1197
86.1
11.3
2.6
2453
350
117
84.0
12.0
4.0
Maternal complication
No
Yes
31 320
5657
84.7
15.3
41 673
4398
90.4
9.6
2620
373
7.5
12.5
Infant gender
Male
Female
18 506
18 471
50.1
49.9
23 030
23 041
50.0
50.0
1316
1677
44.0
56.0
Gestational age (weeks)
24–31
32–35
36–44
4.54
10 292
22 175
11.1
28.2
60.7
3231
12 386
29 897
7.1
27.2
65.7
360
833
1769
12.2
28.1
59.7
Birth weight >4000 g
No
Yes
36 904
73
99.8
0.2
46 009
62
99.9
0.1
2987
6
99.8
0.2
Birth weight discordance
Second twin 25% larger
Second twin 25% smaller
Remaining
2505
2645
31 827
6.8
7.1
86.1
2759
1773
41 539
6.0
3.8
90.2
228
108
2657
7.6
3.6
88.8
a
The State of California, Indiana, South Dakota, and New York (except for New York city) did not send data on smoking. C–C group: delivery by cesarean section after cesarean delivery
of first twin; V–V group: delivery vaginally after vaginal delivery of first twin; V–C group: the second twins delivered by cesarean section after vaginal delivery of the first twin.
Journal of Perinatology
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
6
The proportion of maternal complications was significantly higher in the
C–C group as compared with both V–V and V–C groups (Table 1).
In second twins with birth weight <1500 g, the incidence of
noncongenital anomaly-related death was significantly higher in
the V–X group (8.29%) than in the C–C group (5.81%). The aOR
was 1.24 (1.01, 1.52). However, the relationship was only true in
the V–V group when the V–X group was broken into the V–V
group and the V–C group. The incidence of low Apgar score was
significantly higher in the V–X group (3.94%) than in the C–C
group (2.42%). The OR and its 95% CI was 1.66 (1.26, 2.17). After
adjusting for confounders, the aOR was 1.38 (1.04, 1.84). Again,
the relationship was true only in the V–V group, and not in the
V–C group (Table 2).
In second twins with birth weight 1500–2499 g, the ORs and its
95% CI were 2.97 (1.27, 6.12) for noncongenital anomaly-related
death, 7.36 (1.51, 30.01) for asphyxia-related death, 3.47 (1.92,
5.90) for low Apgar score, 1.84 (1.54, 2.18) for ventilation use, and
7.37 (2.50, 19.88) for occurrence of seizure in the V–C group
compared with the C–C group. The aORs were slightly attenuated
by adjusting for confounders. However, these relationships were
not true in the V–X group when we combined the V–V group and
V–C group (Table 3).
In second twins with birth weight X2500 g, the ORs and its
95% CI were 4.28 (1.81, 12.56) for noncongenital anomaly-related
death, 2.00 (1.22, 3.41) for low Apgar score, 1.22 (1.10, 1.36) for
ventilation use in the V–X group compared with the C–C group.
Adjustment for potential confounding factors did not change these
results. Moreover, these relationships were also true in both the
V–V group and the V–C group and the ORs were much higher in
the V–C group. No asphyxia-related death occurred in the C–C
Table 2 Comparison of neonatal outcomes in vertex–vertex second twins according to mode of delivery (birth weight 500–1499 g), US, 1995–1997
Type of neonatal outcomes and mode of delivery
Noncongenital anomaly-related deaths
C–C group
V–X group
V–V group
V–C group
Number (%) of outcomes
Crude OR (95% CI)
Adjusted OR (95% CI)a
235
243
224
19
(5.81)
(8.29)
(8.62)
(5.71)
Reference
1.47 (1.22, 1.77)
1.53 (1.27, 1.85)
0.98 (0.59, 1.55)
Reference
1.24 (1.01, 1.52)
1.32 (1.07, 1.62)
0.71 (0.40, 1.19)
10
13
12
1
(0.24)
(0.43)
(0.45)
(0.29)
Reference
1.80 (0.79, 4.22)
1.87 (0.81, 4.44)
1.22 (0.07, 6.41)
Reference
1.49 (0.63, 3.66)
1.57 (0.65, 3.92)
0.89 (0.05, 5.00)
Low Apgar score (p3 at 5 minutes)
C–C group
V–X group
V–V group
V–C group
100
118
103
15
(2.42)
(3.94)
(3.88)
(4.42)
Reference
1.66 (1.26, 2.17)
1.63 (1.23, 2.15)
1.87 (1.03, 3.16)
Reference
1.38 (1.04, 1.84)
1.41 (1.05, 1.89)
1.23 (0.64, 2.17)
Ventilation use
C–C group
V–X group
V–V group
V–C group
975
701
619
82
(23.56)
(23.39)
(23.29)
(24.19)
Reference
0.99 (0.89, 1.11)
0.99 (0.88, 1.11)
1.04 (0.80, 1.34)
Reference
0.99 (0.88, 1.12)
1.00 (0.88, 1.13)
0.91 (0.68, 1.19)
(0.17)
(0.13)
(0.15)
(0.00)
Reference
0.79 (0.21, 2.61)
0.89 (0.23, 2.95)
N/A
Reference
0.67 (0.17, 2.31)
0.80 (0.20, 2.77)
N/A
Asphyxia-related deaths
C–C group
V–X group
V–V group
V–C group
Occurrence of seizure
C–C group
V–X group
V–V group
V–C group
a
7
4
4
0
Odds ratios (95% confidence interval) were adjusted for maternal age, race, marital status, cigarette smoking during pregnancy, parity, medical complications (diabetes, pregnancyassociated hypertension, and abnormal labor), abnormality during delivery (precipitous labor, prolonged labor, dysfunctional labor, cephalopelvic disproportion, cord prolapse, and fetal
distress), fetal gender, and gestational age (24–27 weeks, 28–31 weeks, and X32 weeks). C–C group: delivery by cesarean section after cesarean delivery of first twin; V–X group: all
second twins after vaginal delivery of first twin; V–V group: delivered vaginally after vaginal delivery of first twin; V–C group: the second twins delivered by cesarean section after
vaginal delivery of the first twin. N/A: not applicable.
Journal of Perinatology
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
7
Table 3 Comparison of neonatal outcomes in vertex–vertex second twins according to mode of delivery (birth weight 1500–2499 g), US, 1995–1997
Type of neonatal outcomes and mode of delivery
Noncongenital anomaly-related deaths
C–C group
V–X group
V–V group
V–C group
Asphyxia-related deaths
C–C group
V–X group
V–V group
V–C group
Low Apgar score (p3 at 5 min)
C–C group
V–X group
V–V group
V–C group
Ventilation use
C–C group
V–X group
V–V group
V–C group
Occurrence of seizure
C–C group
V–X group
V–V group
V–C group
Number (%) of outcomes
Crude OR (95% CI)
Adjusted OR (95% CI)a
33
34
26
8
(0.21)
(0.15)
(0.12)
(0.61)
Reference
0.73 (0.45, 1.19)
0.60 (0.35, 0.99)
2.97 (1.27, 6.12)
Reference
0.75 (0.45, 1.26)
0.64 (0.37, 1.09)
1.92 (0.75, 4.28)
5
6
3
3
(0.03)
(0.03)
(0.01)
(0.23)
Reference
0.86 (0.26, 2.97)
0.45 (0.09, 1.85)
7.36 (1.51, 30.01)
Reference
1.06 (0.31, 3.81)
0.56 (0.11, 2.36)
5.42 (1.02, 21.66)
57
88
72
16
(0.36)
(0.39)
(0.34)
(1.22)
Reference
1.10 (0.79, 1.54)
0.96 (0.68, 1.36)
3.47 (1.92, 5.90)
Reference
1.13 (0.80, 1.59)
0.99 (0.69, 1.42)
2.36 (1.29, 4.12)
(7.41)
(7.85)
(7.55)
(12.82)
Reference
1.07 (0.99, 1.15)
1.02 (0.94, 1.10)
1.84 (1.54, 2.18)
Reference
1.11 (1.02, 1.20)
1.06 (0.98, 1.16)
1.75 (1.46, 2.09)
(0.06)
(0.08)
(0.05)
(0.46)
Reference
1.21 (0.56, 2.75)
0.83 (0.35, 2.00)
7.37 (2.50, 19.88)
Reference
1.47 (0.66, 3.50)
0.99 (0.40, 2.52)
5.28 (1.69, 15.47)
1188
1767
1599
168
10
17
11
6
a
Odds ratios (95% confidence interval) were adjusted for maternal age, race, marital status, cigarette smoking during pregnancy, parity, medical complications (diabetes, pregnancyassociated hypertension, and abnormal labor), abnormality during delivery (precipitous labor, prolonged labor, dysfunctional labor, cephalopelvic disproportion, cord prolapse, and fetal
distress), fetal gender and gestational age (24–35 weeks and X36 weeks). C–C group: delivery by cesarean section after cesarean delivery of first twin; V–X group: all second twins
after vaginal delivery of first twin; V–V group: delivered vaginally after vaginal delivery of first twin; V–C group: the second twins delivered by cesarean section after vaginal delivery
of the first twin.
group, whereas the incidence of this death was 0.45% in the V–C
group (Table 4).
Discussion
Our large population-based study found a 6.1% rate of emergency
cesarean delivery for the second twin after vaginal delivery of the
first twin in vertex–vertex twin pairs, lower than 9.5% in all second
twins7 and much lower than 24.8% in vertex–nonvertex second
twins of the same population.21 This finding is consistent with
physicians’ consensus that vaginal delivery for twins is safer when
both twins are vertex than vertex–nonvertex presentation.15,16 Only
one previous study has examined the mode of delivery for secondborn twin with vertex–vertex presentation.22 The rate of cesarean
delivery for the second twin after vaginal delivery of the first twin in
that study was 16.9%,22 which was much higher than the rate
observed in our study (6.1%). The study by Sullivan et al.22 was
based on a single obstetric care center with a very small sample
(106 twin sets). The rates of emergency cesarean delivery for the
second twin after vaginal delivery of the first twin were 11.3% in
birth weight <1500 g, 5.8% in birth weight 1500–2499 g, and 5.7%
in birth weight X2500 g in our study, which indicate that
physicians may have a lower threshold to perform an emergency
cesarean section for the second-born twin when the fetus was likely
to be <1500 g. As a result, the rate of cesarean delivery for the
second twin after vaginal delivery of the first twin was higher in
this group of infants than those with a birth weight X1500 g.
Our study found that in second twins with birth weight
<1500 g, the risks of noncongenital anomaly-related neonatal
death, and low Apgar score were increased in all second twins after
Journal of Perinatology
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
8
Table 4 Comparison of neonatal outcomes in vertex–vertex second twins according to mode of delivery (birth weight X2500 g), US, 1995–1997
Type of neonatal outcomes and mode of delivery
Number (%) of outcomes
Crude OR (95% CI)
Adjusted OR (95% CI)a
Noncongenital anomaly-related deaths
C–C group
V–X group
V–V group
V–C group
5
30
18
12
(0.03)
(0.13)
(0.08)
(0.90)
Reference
4.28 (1.81, 12.56)
2.72 (1.09, 8.24)
30.29 (11.22, 95.31)
Reference
4.64 (1.90, 13.92)
2.69 (1.02, 8.39)
19.98 (6.82, 66.58)
Asphyxia-related deaths
C–C group
V–X group
V–V group
V–C group
0
10
4
6
(0.00)
(0.04)
(0.02)
(0.45)
Reference
N/A
N/A
N/A
Reference
N/A
N/A
N/A
Low Apgar score (p3 at 5 min)
C–C group
V–X group
V–V group
V–C group
20
56
40
16
(0.12)
(0.24)
(0.18)
(1.20)
Reference
2.00 (1.22, 3.41)
1.51 (0.90, 2.64)
10.13 (5.16, 19.55)
Reference
2.39 (1.43, 4.14)
1.84 (1.07, 3.27)
5.86 (2.90, 11.68)
594
1010
896
114
(3.56)
(4.31)
(4.06)
(8.55)
Reference
1.22 (1.10, 1.36)
1.15 (1.03, 1.28)
2.54 (2.05, 3.11)
Reference
1.31 (1.18, 1.47)
1.24 (1.11, 1.40)
2.08 (1.66, 2.60)
9
18
12
6
(0.05)
(0.08)
(0.05)
(0.45)
Reference
1.43 (0.66, 3.33)
1.01 (0.43, 2.47)
8.38 (2.81, 23.28)
Reference
1.46 (0.66, 3.46)
1.01 (0.42, 2.50)
6.35 (2.01, 18.75)
Ventilation use
C–C group
V–X group
V–V group
V–C group
Occurrence of seizure
C–C group
V–X group
V–V group
V–C group
a
Odds ratios (95% confidence interval) were adjusted for maternal age, race, marital status, cigarette smoking during pregnancy, parity, medical complications (diabetes, pregnancyassociated hypertension, and abnormal labor), abnormality during delivery (precipitous labor, prolonged labor, dysfunctional labor, cephalopelvic disproportion, cord prolapse, and fetal
distress), fetal gender, and gestational age (24–35 weeks and X36 weeks). C–C group: delivery by cesarean section after cesarean delivery of first twin; V–X group: all second twins
after vaginal delivery of first twin; V–V group: delivered vaginally after vaginal delivery of first twin; V–C group: the second twins delivered by cesarean section after vaginal delivery of
the first twin. N/A: not applicable.
vaginal delivery of first twin as compared with those with both
twins delivered by cesarean section. However, none of the ORs was
larger than 2. Immediate action by physicians might have
prevented some deaths or other severe conditions from occurring
in these infants, and the V–C-related neonatal mortality and
morbidity was therefore less frequent in them because physicians
might have a lower threshold to perform an emergency cesarean
section for the second-born twin when the fetus was likely to be
<1500 g. However, we should interpret our results with caution
because this conclusion was not drawn from randomized clinical
trial, and for those delivered by cesarean section, both selective and
emergency cesarean section were included. These cases might have
different conditions. When there is an indication such as placenta
previa or severe pre-eclampsia, elective cesarean section is likely to
be offered for the delivery of both twins. As a result, the effect of
Journal of Perinatology
mode of delivery on neonatal mortality may be biased towards a
higher risk of neonatal mortality in the group with both twins
delivered by cesarean section.
In second twins with birth weight 1500–2499 g, none of the
risks of mortality and morbidity was higher than in all second
twins after vaginal delivery of first twin as compared with those
both twins delivered by cesarean section, which suggests that
routing cesarean section for vertex–vertex second twins may not be
necessary. Again, we should interpret our results with caution
because this conclusion was not from randomized clinical trial.
However, we should pay attention to the higher risks of mortality
and morbidity in those delivered by cesarean section after vaginal
delivery of the first twin. Physicians may be more reluctant to
perform emergency cesarean section for the second twin when the
fetus was likely to be X1500 g. As a result, delay in intervention
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
9
by physicians might have caused some deaths or other severe
conditions in these infants, and the V–C-related neonatal mortality
and morbidity were therefore much higher.
In second twins with birth weight X2500 g, the risks of
mortality and morbidity were significantly higher in all second
twins who delivered after vaginal delivery of first twin. And these
ORs were much higher in those cesarean delivered after vaginal
delivery of first twin. Again, physicians might be more reluctant to
perform emergency cesarean section for the second twin when the
fetus was likely to be X2500 g. We suggest that routine cesarean
section might be beneficial for those with birth weight X2500 g.
However, our conclusion needs to be confirmed from randomized
clinical trial.
The limitations of our data should be pointed out. Our study
used birth certificate data, which might underestimate certain
complications of pregnancy.23 Other qualities of the data, such as
fetal presentation, order of the birth, and the causes of neonatal
death might be uncertain. As this was a cohort study, there might
be some pre-existing reasons for why a physician chose to offer a
patient with vertex–vertex twins a trial of labor, as opposed to an
outright cesarean section. The reasons for the decision to perform a
cesarean section or vaginal delivery were not available in the data.
Selection bias seemed to be the major methodological issue of this
study. There might also be characteristics of patients who agreed to
a trial of labor that were different from those who desired an
elective cesarean section for both twins. Obviously, the only way to
obtain the most unbiased estimate of the effects of mode of delivery
would be to do a prospective, randomized control trial. In addition,
some of the relative risks were based on very small number of
subjects. Endogeneity is the second major methodological issue.
Endogeneity refers to the fact that an independent variable
included in the model is potentially a choice variable, correlated
with unobservables relegated to the error term. The use of
unconditional logistic regression in this study could not adequately
address endogeneity.24 Potential errors in the coding of cause of
death may not be random. For example, for unknown reasons, the
incidence of asphyxia-related death in this data was lower than
that found in other studies.25 Another limitation is that we did not
analyze separately the twins delivered by the university
perinatologist and residents from the twins delivered by the private
obstetricians because we have no information on that. However,
Greig et al.26 found that there was no significant difference in the
percentage of twins delivered by cesarean section (48 vs 49%)
between the two groups.
In conclusion, our large population-based study found the
emergency cesarean delivery rate in vertex–vertex second twins
whose co-twins delivered vaginally was 6.1%. The risks of mortality
and morbidity are significantly increased in second twins with birth
weight X2500 g whose co-twins delivered vaginally compared with
second twins delivered by cesarean section after cesarean delivery of
first twin.
References
1 Blondel B, Kaminski M. Trends in the occurrence, determinants, and
consequences of multiple births. Semin Perinatol 2002; 26: 239–249.
2 Power WP, Wampler NS. Further defining the risks confronting twins.
Am J Obstet Gynecol 1996; 175: 1522–1528.
3 Rydhstroem H. Should all twins be delivered by caesarean section?
A preliminary report. Twin Res 2001; 4: 156–158.
4 Smith GC, Pell JP, Dobbie R. Birth order, gestational age, and risk of
delivery related perinatal death in twins: retrospective cohort study. BMJ
2002; 325: 1004–1009.
5 Wen SW, Fung Kee Fung K, Oppenheimer L, Demissie K, Yang Q, Walker M.
Neonatal mortality in second twin according to cause of death, gestational
age, and mode of delivery. Am J Obstet Gynocol 2004; 191: 778–783.
6 Wen SW, Fung Kee Fung K, Oppenheimer L, Demissie K, Yang Q, Walker M.
Neonatal morbidity in second twin according to gestational age at birth and
mode of delivery. Am J Obstet Gynocol 2004; 191: 773–777.
7 Wen SW, Fung Kee Fung K, Oppenheimer L, Demissie K, Yang Q, Walker M.
Occurrence and clinical predictors of emergent cesarean delivery for second
twin. Obstet Gynecol 2004; 103: 413–419.
8 Chervenak FA, Johnson RE, Berkowitz RL, Hobbins JC. Intrapartum external
version of the second twin. Obstet Gynecol 1983; 62: 160–165.
9 Crawford JS. A prospective study of 200 consecutive twin deliveries.
Anaesthesia 1987; 42: 33–43.
10 Divon MY, Marin MJ, Pollack RN, Katz NT, Henderson C, Aboulafia Y et al.
Twin gestation: fetal presentation as a function of gestational age. Am J
Obstet Gynecol 1993; 168: 1500–1502.
11 Kelsick F, Minkoff H. Management of the breech second twin. Am J Obstet
Gynecol 1982; 144: 783–786.
12 Thompson SA, Lyons TJ, Makowski EL. Outcomes of twin gestation at the
University of Colorado Health Science centre. J Reproduct Med 1987; 32:
328–329.
13 Laros RK, Dattel BJ. Management of twin pregnancy; the vaginal route is still
safe. Am J Obstet Gynecol 1998; 158: 1330–1338.
14 Piekarski P, Czajkowski K, Maj K, Milewczyk P. Neonatal outcome depending
on the mode of delivery and fetal presentation in twin gestation (abstract).
Ginekol Pol 1997; 68: 187–192.
15 Boggess KA, Chisholm CA. Delivery of the nonvertex second twin: a review of
the literature. Obstet Gynecol Surv 1997; 52: 728–735.
16 Blickstein I. Cesarean section for all twins? J Perinat Med 2000; 28:
169–174.
17 Anonymous. Special problems of multiple gestations. Int J Gynaecol Obstet
1999; 64: 323–333.
18 Barrett J, Bocking A. The SOGC consensus statement on management of twin
pregnancies (Part I). J SOGC 2000; 91: 519–532.
19 National Center for Health Statistics. 1995–1997 Matched Multiple Birth
Data Set. NCHS CD-ROM Series 21, No. 12. U.S. Department of Health and
Human Services, Centers for Disease Control and Prevention: Hyattsville,
Maryland; 2000.
20 Cole S, Hartford RB, Bersjo P, McCarthy B. International collaborative effort
(ICE) in birth weight, plurality, perinatal and infant mortality. Acta Obstet
Gynecol Scand 1989; 68: 113–117.
21 Yang Q, Wen SW, Chen Y, Krewski D, Fung Kee Fung K, Walker M. Neonatal
mortality and morbidity in vertex–nonvertex second twins according to mode
of delivery and birth weight. Am J Obstet Gynecol 2005; 192: 840–847.
Journal of Perinatology
Neonatal mortality and morbidity in vertex–vertex second twins
Q Yang et al
10
22
23
24
Sullivan CA, Harkins D, Seago DP, Roberts WE, Morrison JC. Cesarean
delivery for the second twin in the vertex–vertex presentation: operative
indications and predictability. South Med J 1998; 91: 155–158.
Huston P, Naylor CD. Health services research: reporting on studies using
secondary data sources. Can Med Assoc J 1996; 155: 1697–1702.
Millimet D. What is the difference between ‘endogeneity’ and ‘sample
selection bias’? Frequently Asked Questions (FAQ) for STATA, http://
www.stata.com/support/faqs/stat/bias.html.
Journal of Perinatology
25
26
Wen SW, Joseph KS, Kramer MS, Demissie K, Oppenheimer L, Liston R,
et al., For the Fetal and Infant Mortality Study Group. Canadian
Perinatal Surveillance System. Recent secular trends in fetal and
infant outcomes among post-term pregnancies. Chron Dis Can 2001; 22:
1–5.
Greig P, Veille J, Morgan T, Henderson L. The effect of presentation and
mode of delivery on neonatal outcome in the second twin. Am J Obstet
Gynecol 1992; 167: 901–906.