Neonatal Acid Base Balance and Disturbances
Raymond Quigley* and Michel Baum*†
Maintaining acid base balance presents a considerable challenge to the growing neonate. The infant
must ingest protein for growth and development. The metabolism of sulfur containing amino acids
leads to the production of protons that must be secreted by the kidney. In addition, the formation of
hydroxyapatite for the mineralization of growing bone also leads to acid production. Thus, the
growing infant must excrete approximately 2 to 3 mEq of acid per kilogram of body weight per day
to avoid becoming acidotic. The mechanisms for excreting acid undergo complex maturational
changes that predispose the neonate, and the premature neonate in particular, to a great risk for the
development of acidosis. In addition, infants are susceptible to gastrointestinal disturbances that can
lead to acidosis due to acute loss of bicarbonate in the stool. The kidney is then responsible for the
production of new bicarbonate to restore the body’s acid base balance. There are also a number of
inherited disorders in the kidney that affect acid secretion and lead to acid base disturbances in
neonates. This review discusses the mechanisms by which the kidney is capable of excreting acid as
well as the developmental regulation of these processes and the basis of inherited disorders of
acidification.
© 2004 Elsevier Inc. All rights reserved.
e first review the mechanisms for acid excretion in the mature kidney. To excrete
nitrogenous wastes, the kidney forms urine by a
process of filtration in the glomerulus, followed
by secretion and reabsorption in the tubules.
The high glomerular filtration rate allows for
clearance of the nitrogenous wastes but also
places a large demand on the tubules to reabsorb solutes that are not to be excreted, such as
bicarbonate. A normal adult will form about 150
L of glomerular filtrate each day. This fluid contains about 3,750 mEq of bicarbonate ions (25
mEq/liter) that must be reabsorbed to keep
from losing any bicarbonate. The proximal tubule is responsible for the reabsorption of most
of the solutes filtered by the kidney including
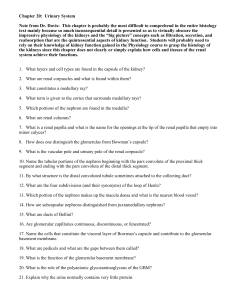
80% of the filtered bicarbonate.1,2 The mechanisms responsible for the reabsorption of bicarbonate by the kidney are illustrated in Figure 1.3
The mechanism for transporting bicarbonate
from the lumen of the tubule to the blood
stream involves several steps. First, hydrogen
ions are secreted into the tubule lumen from the
intracellular compartment. The main transporter for accomplishing this is the sodium-proton (Na⫹/H⫹) exchanger on the luminal membrane of the proximal tubule, which has been
designated NHE3.4 The driving force for the
Na⫹/H⫹ exchanger is generated by the low intracellular sodium concentration that is maintained by the basolateral sodium-potassium
W
ATPase. One turnover of the Na⫹/H⫹ exchanger will result in one sodium ion entering
the cell and one proton (H⫹) exiting the cell
into the lumen of the tubule. In the adult proximal tubule, there is also a proton pump (H⫹ATPase) that derives its energy directly from the
hydrolysis of ATP. It has been estimated that
about two-thirds of proton secretion in the adult
proximal tubule occurs via the Na⫹/H⫹ exchanger and about one third via the H⫹-ATPase.5,6
After entering the lumen of the tubule, the
proton combines with bicarbonate to form carbonic acid (H2CO3), which will dissociate in the
presence of carbonic anhydrase (C.A.) to water
and carbon dioxide as in equation 1:
¢ ¡
H ⫹ ⫹ HCO 3⫺O
carbonic anhydrase
H 2CO 3O
¢
¡H 2O ⫹ CO 2.
(1)
From the Departments of *Pediatrics; and †Internal Medicine, University of Texas Southwestern Medical Center at Dallas, Dallas, TX.
Address reprint requests to Raymond Quigley, MD, Department of
Pediatrics, UT Southwestern Medical Center, 5323 Harry Hines
Blvd., Dallas, TX 75390-9063.
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2802-0003$30.00/0
doi:10.1053/j.semperi.2003.11.006
Seminars in Perinatology, Vol 28, No 2 (April), 2004: pp 97-102
97
98
Quigley and Baum
Figure 1. Mechanism of proximal tubule bicarbonate
reabsorption. Protons are secreted into the lumen of
the tubule by the Na⫹/H⫹ exchanger and the H⫹ATPase. The intracellular sodium is maintained at a
lower concentration compared to the extracellular
sodium concentration by action of the Na⫹/K⫹
ATPase, providing energy for the Na⫹/H⫹ exchanger. Once the proton is in the lumen, it combines with bicarbonate to form carbonic acid that is
converted by carbonic anhydrase (C.A.) to water and
carbon dioxide. The H2O and CO2 then diffuse into
the cell and recombine in the presence of C.A. to
form carbonic acid that ionizes into H⫹ and bicarbonate. The protons then can be secreted into the lumen
and the bicarbonate exits across the basolateral membrane and into the blood stream. (Enclosed circles
represent ATPases; Open circles represent transporters that utilize secondary transport).
The water and carbon dioxide generated can
then enter the proximal tubule cell where they
recombine, in the presence of carbonic anhydrase, to form carbonic acid.3 In the cell the
reaction then runs in the reverse direction to
generate a proton and bicarbonate. The bicarbonate exits the cell across the basolateral membrane and then goes into the blood stream,
which is mediated by a sodium-bicarbonate cotransporter.7,8 Thus, bicarbonate transport is
closely linked to sodium reabsorption in the
proximal tubule. The thick ascending limb of
Henle and the distal convoluted tubule reabsorb
the remaining 20% of the filtered bicarbonate
not reabsorbed by the proximal tubule.3
As noted above, the kidney must not only
reclaim the filtered bicarbonate but must secrete
the acid generated from the metabolism of protein (and bone formation in the growing child).
This is accomplished by secretion of protons in
the collecting duct. First, we need to realize the
problem with secreting acid as protons. If the
urine pH (-log[H⫹]) can be reduced to 4 (actually 4.5 is about the lowest attainable urine pH in
man) it would be necessary to produce 500 L of
urine for an adult to excrete 50 mmol of acid.
Thus, the kidney must be able to excrete acid
with buffers so that the urine can contain 50
mmol of acid in a small volume at a pH of 4.5.
To excrete acid in a small volume of urine the
kidney produces ammonia.3,9 Ammonia is primarily generated in the proximal tubule by the
deamination of glutamine by the enzyme glutaminase and is then protonated in the distal
tubule to form ammonium.9 There are a few
other enzymes involved in the process of ammoniagenesis, but glutaminase is by far the most
important for producing ammonia and can be
stimulated 10-fold by acidosis. Thus, most of the
acid we excrete daily is in the form of ammonium chloride. A smaller fraction of the acid is
buffered by phosphate and sulfate. This is referred to as titratable acidity.3 Net acid excretion
in the adult is the sum of ammonium and titratable acidity, which matches precisely the amount
of acid generated from metabolism and new
bone formation.
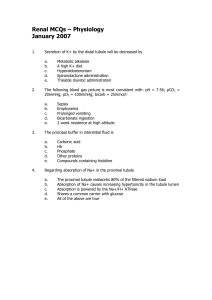
The excretion of the protons by the collecting
duct is depicted in Figure 2. The intercalated
cells of the collecting duct are divided into 2
types.3 The ␣-intercalated cells contain an H⫹ATPase in the luminal membrane for the secretion of protons. When the acid is secreted, bicarbonate is generated in the cell and must be
excreted across the basolateral membrane into
the blood stream. This occurs through a chloride-bicarbonate exchanger, which is designated
AE1 (Anion-Exchanger 1). The activity of the
␣-intercalated cell increases during acidosis. The
-intercalated cells secrete base into the lumen
and acid into the blood stream. These cells become active when a patient becomes alkalotic
and needs to correct the alkalosis.
Maturation of Acid Excretion
Neonates have a serum bicarbonate that is lower
than that of adults. The lower level of serum
bicarbonate is caused by a lower bicarbonate
threshold, the maximal capacity of the kidney to
reabsorb bicarbonate.10 In the neonate as in the
adult, most of bicarbonate reabsorption occurs
in the proximal tubule. The rate of neonatal
Neonatal Acid Base Balance and Disturbances
Figure 2. Mechanism of acid secretion in the ␣-intercalated cells. The ␣-intercalated cell has an H⫹ATPase located on the apical membrane for secreting
protons into the lumen. Protons and bicarbonate are
generated by carbonic anhydrase from water and carbon dioxide inside the cell. Bicarbonate exits across
the basolateral membrane by a chloride-bicarbonate
exchanger. The protons combine with buffers in the
tubule lumen, which include ammonia, phosphate
and sulfate. (Enclosed circles represent ATPases;
Open circles represent transporters that utilize secondary transport).
proximal tubule bicarbonate reabsorption is approximately one third that of the adult proximal
tubule.11 The lower rate of bicarbonate reabsorption is not due to a back leakage of transported bicarbonate from the blood stream into
the lumen but due to a lower rate of bicarbonate
reabsorption.12
All of the transporters responsible for the
reabsorption of bicarbonate have a lower activity
in the neonatal proximal tubule when compared
to the adult.13,14 The basolateral sodium-potassium ATPase, responsible for maintaining the
low intracellular sodium concentration, has
about one half the activity compared to that of
the adult.15 The apical Na⫹/H⫹ exchanger has a
much lower activity and is in much lower abundance on the apical membrane of the neonatal
proximal tubule.5 There appears to be no activity of the H⫹-ATPase in the proximal tubule of
the neonate.5 In addition, the basolateral sodium-bicarbonate cotransporter is in lower
abundance in the neonatal proximal tubule
compared to that of the adult.5 Thus, all of the
active transport steps for the reabsorption of
bicarbonate are underdeveloped in the neonate.
The factors that induce the maturation of
99
bicarbonate reabsorption are currently under
investigation. It is clear that one of the major
hormones that stimulate the development of bicarbonate transport are glucocorticoids.13,14 Neonates are relatively glucocorticoid deficient
during the first weeks of life. There is a developmental increase of glucocorticoids that precedes
the increase in bicarbonate transport. Indeed, if
pregnant rabbits are injected with glucocorticoids prior to giving birth, the neonates have a
proximal tubule bicarbonate transport rate that
is comparable to that of the adult proximal tubule.16 Glucocorticoids affect several steps in the
regulation of transport. Thyroid hormone also
affects the development of bicarbonate transport but plays a much less important role.17
If glucocorticoids can hasten the development of transport in the kidney tubules, why
don’t we treat all premature infants with these
drugs? There is mounting evidence that there
can be considerable detrimental effects of prenatal glucocorticoids. Rats that were treated with
dexamethasone prenatally during specific times
during gestation were found to develop hypertension when they became adults.18 In addition,
examination of their kidneys revealed an increase in glomerulosclerosis. While one cannot
and should not make any conclusions about humans from these studies, it is possible that prenatal glucocorticoids may have adverse effects in
humans if given at particular times during renal
development.
The collecting duct is divided into the cortical
collecting duct and the inner and outer medullary collecting duct. Data from perfused tubules
from rabbit kidneys indicate that the cortical
collecting duct has a decreased ability to secrete
acid in the neonate when compared to the
adult.19 This is because of the fact that there is
about one half the number of intercalated cells
in the cortical collecting duct of the neonate as
compared to the adult.20-22 The medullary collecting duct in the neonate has transport rates
that are comparable to that of the adult and the
number of intercalated cells is also comparable.
So the overall developmental change in the collecting duct is that the neonatal collecting duct
has a lower rate of transport than the adult
collecting duct.
There is also evidence for developmental
changes in renal carbonic anhydrase activity.
There are 2 major isoforms of carbonic anhy-
100
Quigley and Baum
drase in the kidney that are designated C.A. II,
which is located in the intracellular compartment, and C.A. IV, which is located on the luminal membranes of the tubules, primarily the
proximal tubules.23,24 In maturing rabbits, carbonic anhydrase IV has been shown to increase
its activity and parallels the developmental increase in bicarbonate reabsorption in the proximal tubule.25,26 Thus, there is a lower activity
rate of this enzyme in the neonatal kidneys that
may contribute to the lower rates of acid secretion. More recently, carbonic anhydrase II was
also shown to have lower abundance in neonatal
rats.27 This isoform appears to be critical for the
function of the intercalated cells of the collecting duct and may be responsible for the developmental increase in the collecting ducts ability
to excrete acid. However, when studied in humans, it appears that there is not much difference in carbonic anhydrase activity between the
neonate and adult kidneys.28 Neonatal human
kidneys do have more carbonic anhydrase activity in the juxtamedullary region where the
nephrons are more developed than the superficial cortical region.29 Thus, it is unclear in humans if the differences in carbonic anhydrase
activity between neonates and adults are critical
for the development of acidification.
One other aspect of acidification that is important in the development of acidification is
ammoniagenesis. As we discussed earlier, most
of our acid is secreted in the form of ammonia.9
Without this crucial buffer, it is very difficult to
excrete large amounts of acid in a relatively
small volume of urine. The enzymes for ammoniagenesis are present in the neonate, but the
rates of ammonia production are somewhat less
than that of the adult.30,31 The primary enzyme,
glutaminase, has a lower activity in the neonatal
kidney. The renal content of glutamine as a
substrate is also lower in the neonatal kidney
than the adult kidney. There is a higher concentration of glutaminate in the neonatal kidney
that probably inhibits the action of glutaminase.
In addition, while the adult kidney can increase
ammonia production by 10-fold during acidosis,
the neonate cannot. Thus, when neonates become acidotic (for instance with diarrhea) it
takes them much longer to recover from the
acidosis.
The neonate, as the adult, must excrete acid
generated form metabolism in the form of am-
monia and titratable acid. While adults need to
excrete about 1 mEq/kg per day of acid, neonates need to excrete 2 to 3 times this amount
because of their protein intake and the formation of new bone. As we have just seen, the
transport mechanisms for the excretion of acid
undergo complex developmental changes. We
will next review how the neonate manages to
survive and grow and also review some of the
disturbances that affect neonates.
Acid Base Disturbances
So how does the growing infant survive with
these developmentally low rates of acid excretion? Acid-base balance is maintained in part by
the ingestion of base equivalents contained in
the mother’s milk. The mineralization of bone
places a huge demand on the kidney to excrete
acid, which it probably could not keep up with.
Thus, the ingested base equivalents help keep
the growing infant in acid base balance at a time
when its kidney’s ability to excrete acid is underdeveloped.
Premature neonates have tubules which are
much less mature that that of the term neonate.10 Thus, very premature neonates can have
a generalized proximal tubule transport disorder known as the Fanconi syndrome. They will
have glucosuria with normal serum glucose levels, aminoaciduria, and lower serum bicarbonate levels. Administration of bicarbonate does
little to improve growth in very premature neonates.32
Another common problem for neonates is
the loss of bicarbonate due to gastrointestinal
disturbances. The pancreas secretes bicarbonate
into the small intestine to neutralize the stomach acid. When the baby develops diarrhea,
much of this bicarbonate is lost and the infant
becomes acidotic. Several aspects of development make this a severe problem in the infant.
First, the growing infant is dependent on base
equivalents in the mother’s milk to help maintain acid base balance. When the infant has
diarrhea, milk is often withheld from the neonate, which deprives him of this source of base.
Second, while the ammonia production of the
kidney of the neonate may help keep him in
balance under normal conditions, unlike the
adult, there is limited ability of the neonatal
kidney to increase NH3 production to replace
Neonatal Acid Base Balance and Disturbances
the bicarbonate that was lost in the gastrointestinal tract. Thus, it will take the infant much
longer than an adult to recover from the loss of
bicarbonate. And last, the tubules’ (both proximal and distal) ability to secrete protons is also
somewhat limited, which will again cause the
infant to take a long time to recover from the
acidosis.
These same factors probably also limit the
infant’s ability to recover from acidosis generated by sepsis (ie, lactic acidosis) or from the
administration of amino acids in the TPN. Arginine in the TPN is a source of HCl. One must
remember that large amounts of arginine in the
TPN of premature infants can result in a metabolic acidosis.
Inherited Defects in Acidification
We will next consider some of the genetic defects that result in acid-base disturbances. In
general, defects that interfere with the reabsorption of bicarbonate in the proximal tubule or
with the secretion of protons in the collecting
duct lead to renal tubular acidosis. This form of
metabolic acidosis is characterized by a low bicarbonate concentration and an elevated chloride concentration, thus the anion gap in these
patients is normal. A discussion of metabolic
acidosis with an elevated anion gap is beyond the
scope of this review.
The proximal tubule reabsorbs not only bicarbonate, but glucose, phosphate and amino
acids. Most disorders that cause a defect in proximal tubule acidification also involve these other
solute transporters and are referred to as the
Fanconi syndrome. These solutes are all transported by sodium coupled transporters, thus,
the common factor to these transport processes
is the luminal membrane sodium concentration
gradient. So the Fanconi’s syndrome results
from a defect in maintaining the luminal membrane sodium concentration gradient.
The most common inherited defect that
causes this is cystinosis.33 Cystinosis is a defect in
the lysosomal transporter for cystine and leads to
accumulation of cystine in the lysosomes. This
then leads to depletion of ATP as the energy
source for the sodium-potassium ATPase and
the sodium concentration gradient is dissipated.34 Thus, all of the lumen transporters that
are sodium coupled have a lower rate of trans-
101
port, which results in bicarbonaturia, glucosuria,
phosphaturia, and aminoaciduria. The other defects that lead to proximal tubule acidosis probably have the same mechanism and include tyrosinemia, galactosemia, and inherited fructose
intolerance. Rarely, proximal tubule acidosis
can be inherited without the Fanconi syndrome.
Recently, a defect in the sodium-bicarbonate cotransporter was found that caused proximal tubular acidosis and eye defects.35
Defects in the collecting duct’s ability to secrete protons lead to distal renal tubular acidosis. The primary inherited defect that has recently been characterized is in the H⫹-ATPase.36
This transporter has multiple subunits. The
most commonly inherited defect is in the -subunit. This subunit is also found in the inner ear,
so children with this defect have sensorineural
hearing loss. Another form of distal RTA that is
inherited as an autosomal dominant trait is due
to a defect in the basolaterally located chloridebicarbonate exchanger, AE1.37
Another rare form of renal tubular acidosis is
due to a defect in carbonic anhydrase.38 This
causes a combined proximal and distal renal
tubular acidosis. Because carbonic anhydrase is
also involved in the mineralization of bone,
these patients also develop osteopetrosis.
Renal tubular acidosis can also be acquired.
The most common cause of this is due to administration of drugs. Aminoglycosides, in particular
gentamicin, has been associated with proximal
renal tubular acidosis and the Fanconi syndrome.39 Amphotericin B has been associated
with distal tubular acidosis.40 It is thought that
amphotericin B causes an increase in the permeability of the distal nephron so that the tubule
cannot maintain the necessary hydrogen ion
concentration gradient to excrete acid.
References
1. Liu FY, Cogan MG: Axial heterogeneity of bicarbonate,
chloride, and water transport in the rat proximal convoluted tubule. Effects of change in luminal flow rate and
of alkalemia. J Clin Invest 78:1547-1557, 1986
2. Rector FC: Sodium, bicarbonate, and chloride absorption by the proximal tubule. Am J Physiol Renal Physiol
244:F461-F471, 1983
3. Hamm LL, Alpern RJ: Cellular mechanisms of renal
tubular acidification, in Seldin DW, Giebisch G (eds):
The Kidney: Physiology and Pathophysiology New York,
102
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
Quigley and Baum
NY, Lippincott, Williams and Wilkins, 2000, pp 1935–
1979
Tse C-M, Brash AR, Walker P, et al: Cloning and sequencing of a rabbit cDNA encoding an intestinal and
kidney-specific Na⫹/H⫹ exchanger isoform (NHE-3).
J Biol Chem 267:9340-9346, 1992
Baum M: Neonatal rabbit juxtamedullary proximal convoluted tubule acidification. J Clin Invest 85:499-506,
1990
Preisig PA, Ives HE, Cragge EJ Jr, et al: Role of the
Na⫹/H⫹ antiporter in rat proximal tubule bicarbonate
absoprtion. J Clin Invest 80:970-978, 1987
Aronson PS, Soleimani M, Grassl SM: Properties of the
renal Na(⫹)-HCO3- cotransporter. Semin Nephrol 11:
28-36, 1991
Grassl SM, Aronson PS: Na⫹/HCO3- Co-transport in
basolateral membrane vesicles isolated from rabbit renal
cortex. J Biol Chem 261:8778-8783, 1986
Nagami G: Renal ammonia production and excretion, in
Seldin DW, Giebisch G (eds): The Kidney: Physiology
and Pathophysiology New York, NY, Lippincott, Williams
and Wilkins, 2000, pp 1995–2013
Baum M, Quigley R: Postnatal Renal Development, in
Seldin DW, Giebisch G (eds): The Kidney: Physiology
and Pathophysiology New York, NY, Lippincott, Williams
and Wilkins, 2000, pp 703–726
Schwartz GJ, Evan AP: Development of solute transport
in rabbit proximal tubule. I. HCO3 and glucose absorption. Am J Physiol 245:F382-F390, 1983
Quigley R, Baum M: Developmental changes in rabbit
juxtamedullary proximal convoluted tubule bicarbonate
permeability. Pediatr Res 28:663-666, 1990
Baum M, Quigley R: Maturation of proximal tubular
acidification. Pediatr Nephrol 7:785-791, 1993
Baum M, Quigley R: Ontogeny of proximal tubule acidification [editorial]. Kidney Int 48:1697-1704, 1995
Schwartz GJ, Evan AP: Development of solute transport
in rabbit proximal tubule. III. Na-K-ATPase activity. Am J
Physiol 246:F845-F852, 1984
Baum M, Quigley R: Prenatal glucocorticoids stimulate
neonatal juxtamedullary proximal convoluted tubule
acidification. Am J Physiol 261:F746-F752, 1991
Baum M., Dwarakanath V, Alpern RJ, et al: Effects of
thyroid hormone on the neonatal renal cortical
Na⫹/H⫹ antiporter. Kidney Int 53:1254-1258, 1998
Ortiz LA, Quan A, Weinberg A, et al: Effect of prenatal
dexamethasone on rat renal development. Kidney Int
59:1663-1669, 2001
Mehrgut F.M, Satlin LM, Schwartz G J: Maturation of
HCO3- transport in rabbit collecting duct. Am J Physiol
259:F801-F808, 1990
Kim J, Tisher CC, Madsen KM: Differentiation of intercalated cells in developing rat kidney: An immunohistochemical study. Am J Physiol 266:F977-F990, 1994
Satlin LM, Matsumoto T, Schwartz GJ: Postnatal matu-
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
ration of rabbit renal collecting duct III. Peanut lectinbinding intercalated cells. Am J Physiol 262:F199-F208,
1992
Satlin LM, Schwartz GJ: Postnatal maturation of rabbit
renal collecting duct: intercalated cell function. Am J
Physiol 253:F622-F635, 1987
Brown D, Zhu XL, Sly WS: Localization of membraneassociated carbonic anhydrase type IV in kidney epithelial cells. Proc Natl Acad Sci USA 87:7457-7461, 1990
Schwartz GJ: Physiology and molecular biology of renal
carbonic anhydrase. J Nephrol 15suppl 5:S61-S74, 2002
Schwartz GJ, Olson J, Kittelberger AM, et al: Postnatal
development of carbonic anhydrase IV expression in
rabbit kidney. Am J Physiol 276:F510-F520, 1999
Winkler CA, Kittelberger AM, Watkins RH, et al: Maturation of carbonic anhydrase IV expression in rabbit
kidney. Am J Physiol 280:F895-F903, 2001
Karashima S, Hattori S, Ushijima T, et al: Developmental
changes in carbonic anhydrase II in the rat kidney.
Pediatr Nephrol 12:263-268, 1998
Day R, Franklin J: Renal carbonic anhydrase in premature and mature infants. Pediatrics 7:182-185, 1951
Lonnerholm G, Wistrand PJ: Carbonic anhydrase in the
human fetal kidney. Pediatr Res 17:390-397, 1983
Goldstein L: Renal ammonia and acid excretion in infant rats. Am J Physiol 218:1394-1398, 1970
Goldstein L: Ammonia metabolism in kidneys of suckling rats. Am J Physiol 220:213-217, 1971
Schwartz GJ, Haycock GB, Edelmann CM Jr, et al: Late
metabolic acidosis: A reassessment of the definition.
J Pediatrics 95:102-107, 1979
Gahl WA, Thoene JG, Schneider JA: Cystinosis. New
Engl J Med 347:111-121, 2002
Baum M: The Fanconi syndrome of cystinosis: insights
into the pathophysiology. Pediatr Nephrol 12:492-497,
1998
Usiu T, Hara M, Satoh H, et al: Molecular basis of ocular
abnormalities associated with proximal tubular acidosis.
Journal of Clinical Investigation 108:107-115, 2001
Borthwick KJ, Karet FE: Inherited disorders of the H⫹ATPase. Curr Opin Nephrol Hypertens 11:563-568, 2002
Bruce LJ, Cope DL, Jones GK, et al: Familial distal renal
tubular acidosis is associated with mutations in the red
cell anion exchanger (Band 3, AE1). J Clin Invest 100:
1693-1707, 1997
Al Rajeh S, el Mouzan MI, Ahlberg A, et al: The syndrome of osteopetrosis, renal acidosis and cerebral calcification in two sisters. Neuropediatrics 19:162-165,
1988
Melnick J.Z, Baum M, Thompson JR: Aminoglycosideinduced Fanconi’s syndrome. Am J Kidney Dis 23:118122, 1994
Steinmetz PR, Lawson LR: Defect in urinary acidification
induced in vitro by amphotericin B. J Clin Invest 49:596601, 1970