RESEARCH
Abstract
Purpose: The aim of this study was to
examine the accuracy of arterial oxygen
saturation (Sao2) and venous oxygen
saturation (Svo2) with paired arterial
and venous (AV) blood in relation to
pulse oximetry saturation (Spo2) and
oxyhemoglobin (Hbo2) with fetal hemoglobin determination, and their Hbo2
dissociation curves. Method: Twelve
preterm neonates with gestational ages
ranging from 27 to 34 weeks at birth,
who had umbilical AV lines inserted,
were investigated. Analyses were
performed with 37 pairs of AV blood
samples by using a blood volume safety
protocol. Results: The mean differences
between Sao2 and Svo2, and AV Hbo2
were both 6 percent (F6.9 and F6.7
percent, respectively), with higher Svo2
than those reported for adults. Biases
were 2.1 F 0.49 for Sao2, 2.0 F 0.44 for
Svo2, and 3.1 F 0.45 for Spo2, compared against Hbo2. With left-shifted
Hbo2 dissociation curves in neonates,
for the critical values of oxygen tension
values between 50 and 75 millimeters of
mercury, Hbo2 ranged from 92 to 93.4
percent; Sao2 ranged from 94.5 to 95.7
percent; and Spo2 ranged from 93.7 to
96.3 percent (compared to 85 – 94 percent in healthy adults). Conclusions: In
neonates, both left-shifted Hbo2 dissociation curve and lower AV differences
of oxygen saturation measurements indicated low flow of oxygen to the body
tissues. These findings demonstrate the
importance of accurate assessment of
oxygenation statues in neonates.
n 2005 Elsevier Inc. All rights
reserved.
Accurate
Measurements
of Oxygen
Saturation in
Neonates: Paired
Arterial and
Venous Blood
Analyses
By Shyang-Yun Pamela K. Shiao, PhD, RN, FAAN
O
xygen saturation (So2) measurements (functional measurement, So2;
and fractional measurement, oxyhemoglobin [Hbo2]) and monitoring
are commonly investigated as a method of assessing oxygenation in
neonates. Differences exist between the So2 and Hbo2 when blood tests are
performed, and clinical monitors indicate So2 values.1 Oxyhemoglobin will
decrease with the increased levels of carbon monoxide hemoglobin (Hbco) and
methemoglobin (MetHb), and it is the most accurate measurements of oxygen
(O2) association of hemoglobin (Hb). Pulse oximeter (for pulse oximetry
saturation [Spo2] measurement) is commonly used in neonates. However, it
will not detect the changes of Hb variations in the blood for accurate So2
measurements.2 – 4 Thus, the measurements from clinical oximeters should be
used with caution. In neonates, fetal hemoglobin (HbF) accounts for most of the
circulating Hb in their blood. Fetal hemoglobin has a high O2 affinity, thus
releases less O2 to the body tissues, presenting a left-shifted Hbo2 dissociation
curve.5,6 To date, however, limited data are available with HbF correction, for
accurate arterial and venous (AV) So2 measurements (arterial oxygen saturation
[Sao2] and venous oxygen saturation [Svo2]) in neonates, using paired AV
blood samples.
Fetal Hemoglobin and Oxygen Saturation Measurements
From the School of Nursing, University of Texas
Health Science Center at Houston, Houston, TX.
Address reprint requests to Shyang-Yun Pamela
Shiao, PhD, RN, FAAN, School of Nursing,
University of Texas Health Science Center at
Houston, 6901 Bertner Ave. SONSCC 567-8,
Houston, TX 77030.
n 2005 Elsevier Inc. All rights reserved.
1527-3369/05/0504-0112$30.00/0
doi:10.1053/j.nainr.2005.09.001
A
ccurate measurements of So2 are dependent on HbF, Hbo2, and related
parameters. Although HbF was useful to fetus to compete O2 at placenta
with mother’s adult hemoglobin (HbA), it compromises oxygenation to the
body tissue after birth. Neonates manifest desaturation events as the pulse
oximeter loses sensitivity for measurement.7 A pulse oximeter can overestimate
So2 by as much as 6 percent when HbF is not accounted for.7 –11 When low O2
Newborn and Infant Nursing Reviews, Vol 5, No 4 (December), 2005: pp 170 –178
170
Arterial and Venous Oxygen Saturation
was delivered to the body tissue during events such as
bradycardia and desaturation (b90 percent for Sao2), the
neonate’s oxygenation would be further compromised.
In previous reports, widely spread Spo2 readings had
been associated with Pao2 values without providing a
reasonably precise Hbo2 dissociation curve.12,13 The
accuracy of pulse oximetry is limited when the saturation
drops to lower than 80 percent,8,14,15 and its accuracy is
of greater concern for neonates with HbF and low oxygen
to the body.16 The normal clinical Pao 2 range was
defined as 50 to 75 millimeters of mercury for infants
and could be lower for preterm infants.17 In adults, Spo2
of 85 to 94 percent was associated with Pao2 of 50 to
75 millimeters of mercury.18 Comparable ranges of So2
need to be established for neonates, taking into the account
of HbF determination.
Arterial and Venous S O 2
O
nly one previous study provided complete information on the validation of Sao2 and Svo2 in neonates,
however, without HbF determination and related adjustments.19 Arterial oxygen saturation and venous oxygen
saturation measurements together can be used to assess
the systemic supply and demand of O2 for systemic
oxygenation status. 20 –23 Venous oxygen saturation
changes occur sooner and in more obvious increments
than decreases in Sao2 during nursing care and interventions in adults.20 – 22 Venous oxygen saturation is rarely
measured in neonates,24 perhaps with the concern for the
accuracy of measurement for the presence of patent ductus
arteriosus and patent foramen ovale. These features could
cause central hemodynamic shunting resulting from
persistent fetal circulation, thus compromising oxygenation status to the body tissue. Nonetheless, the hemodynamic shunting can be assessed when AV So2 is measured
in neonates.23,24
Arterial and Venous Hb CO
C
arbon monoxide hemoglobin is a common cause
to overestimate So2 in clinical monitoring when
hemoximeter measurements are not determined using the
blood analyses. In addition, when HbF was not corrected
on the hemoximeter tests, Hbco readings were artificially
increased, which then widened the differences between
So2 and Hbo2 readings.4,5 The most common reason for
elevated Hbco is inhalation of CO in fire accidents.3,25,26
Examination of AV Hbco in adults yielded high correlations (0.97 – 0.99) with a negligible mean AV Hbco
difference of 0.15 percent.27,28
171
In a study of critically ill adult patients, increased
pulmonary CO production and elevation in arterial Hbco
but not venous Hbco were documented by inflammatory
stimuli inducing pulmonary heme oxygenase–1.29 In
normal adults, venous Hbco level might be slightly higher
than or equal to arterial Hbco because of production of CO
by enzyme heme oxygenase–2, which is predominantly
produced in the liver and spleen. However, hypoxia or
pulmonary inflammation could induce heme oxygenase–1
to increase endogenous CO, thus elevating pulmonary
arterial and systemic arterial Hbco levels in adults.30 Both
endogenous and exogenous CO can suppress proliferation
of pulmonary smooth muscles, a significant consideration
for the prevention of chronic lung diseases in newborns.
Despite these considerations, a later study31 in healthy
adults indicated that the AV differences in Hbco were
from technical artifacts and perhaps from inadequate
control of different instruments. Thus, further studies are
needed to provide more definitive answers for the AV
differences of Hbco for adults and neonates with acute and
chronic lung diseases.
Arterial and Venous MetHb
M
ethemoglobin is an indicator of Hb oxidation and is
essential for accurate measurement of Hbo2, So2,
and oxygenation status. No evidence exists to show the AV
MetHb difference, although this difference was elucidated
with the potential changes of MetHb with different O2
levels. Methemoglobin can be increased with nitric oxide
(NO) therapy, used in respiratory distress syndrome (RDS)
to reduce pulmonary hypertension and during heart
surgery.32,33 Nitric oxide, in vitro, is an oxidant of Hb,
with increased O2 during ischemia reperfusion. In hypoxemic conditions in vivo, nitrohemoglobin is a product
generated by vessel responsiveness to nitrovasodilators.34
Nitro-hemoglobin can be spontaneously reversible in vivo,
requiring no chemical agents or reductase. However, when
O2 levels were increased experimentally in vitro following
acidic conditions (pH 6.5) to simulate reperfusion conditions, MetHb levels were increased for the hemolysates
(broken red cells).35 Nitrite-induced oxidation of Hb was
associated with an increase in red blood cell membrane
rigidity, thus contributing to Hb breakdown.35 A newer in
vitro study of whole blood cells, however, concluded that
MetHb formation is not dependent on increased O2
levels.36 Additional studies are needed to examine in vivo
reperfusion of O2 and MetHb effects.
For oxidation stress to the tissue and cells occurring
with reperfusions, both animal models37,38 and human
(newborn umbilical blood) studies39,40 have found DNA
damage when oxygenation was increased after hypoxia
172
Shyang-Yun Pamela K. Shiao
during perinatal asphyxia to the fetuses and neonates.
Cellular oxidation injury might occur at various organs,
including brain tissue, after hypoxia (low O2 to the tissue)
in neonates.37 – 40 Considering that serum antioxidant
activity is lower in neonates than adults, especially during
the ischemia-reperfusion period,41 monitoring oxygenation
status is critical. Electron carriers such as methylene blue
as strong reducing agents can be used to treat elevated
MetHb levels.32
These findings for MetHb also indicate the rationale to
use fresh HbA for blood transfusion in neonates. In stored
blood, as the Hb cells break down, MetHb levels could
increase because of accelerated ferrous activity.42 Transfusing old HbA cells could impair cardiac function and
coronary flow in neonatal hearts experiencing ischemia
and reperfusion.41 The most recent recommendation for
the maximum storage of blood for transfusion is
35 days43,44 because the half-life of transfused HbA was
about 30 days.43 Further studies are needed for neonates
with reperfusion and blood transfusion during ventilatory
support. Arterial and venous MetHb differences could be
helpful in assessing oxidation stress with changing oxygenation status in neonates.
The purposes of this study, therefore, were (1) to
examine the difference between So2 (Sao2, Svo2, and
Spo2) in relation to Hbo2 measurements (accounting
Hbco and MetHb) with HbF determination using paired
AV blood samples and pulse oximetry, and (2) to present
the Hbo2 dissociation curves in relation to O2 tension (Po2)
values for accurate assessment of oxygenation in neonates.
Comparing paired AV blood samples allows the examination of systemic balance of oxygenation status in neonates.
Methods
Setting
This study is part of a larger clinical study involving
around-the-clock data collection for neonates in three
neonatal intensive care units. The appropriate institutional
human subjects review boards approved the study protocols. Informed consents were obtained from the parents
and guardians of all newborn subjects before or immediately after the births of high-risk neonates. As part of care
for severe respiratory distress (RDS) and ventilatory
support in neonatal intensive care units, umbilical artery
catheters (UACs) and umbilical venous catheters (UVCs)
were inserted for these neonates as central line access to
assess blood O2 levels and to provide nutrients for the
neonates. Umbilical artery catheters were inserted at the
high positions (above lumbar 1) because lower placements
were more likely to cause vascular spasm to the lower
extremities. Umbilical venous catheters were inserted
approximately 1 centimeter above the liver, at inferior
vena cava. Blood was obtained through the UAC and
UVC lines, from first to fifth days of life, coordinated to
occur every 8 hours with routine blood gas tests. To
conserve blood volume for these critically ill neonates, a
safety blood volume protocol was instituted. Less than
4 milliliters per kilogram of blood was drawn from each
subject during the entire duration of the study. Medical
records were prospectively reviewed to obtain subject’s
demographic data, medical history, and laboratory and
monitoring parameters.
Sample
Immediately after birth, neonates who were diagnosed
with RDS requiring ventilatory support were included in
the study. All neonates had successful insertions of UAC
and UVC. Neonates with major congenital defects (heart,
brain, and neurological, or gastrointestinal defects) were
excluded because interpretation of accurate Sao2 and Svo2
would be problematic in these cases. Neonates who had
life-threatening persistent pulmonary hypertension and
needed NO treatments or extracorporeal membrane oxygenation were excluded with added features to intensive
care for feasibility concerns. A priori power analysis
indicated that 36 (nonindependent) blood tests were needed
for accuracy testing of Spo2 with HbF correction. The
sample included 12 neonates, all having severe respiratory
distress, who provided 37 pairs of AV blood samples. Gestational ages of the neonates ranged from 27 to 34 weeks,
and birth weights ranged from 875 to 2245 grams.
Instruments
Fetal hemoglobin and all So2 parameters were measured by using a hemoximeter (co-oximeter) model
OSM3 (Radiometer Corp, Cleveland, Ohio), using sixwavelength fiberoptic reflectance oximetry (535, 560, 577,
622, 636, and 670 nanometers). Newer models of
hemoximeter (after 1993) have been reported to adjust
So2 or Hbo2 readings by HbF levels using a linear
relationship assumption.45 The accuracy of this newer cooximeter, as reported by the manufacturer, is a test-retest
variability of less than 0.1 percent for normal Hb level
and 0.2 to +0.4 percent for extreme anemia and polycythemia (Hb measurement ranges, 3.2 to 28 grams per
deciliter). The instrument allowed in vitro measurements
of So2, Hbo2, total hemoglobin (tHb) levels, and HbF
concentrations through determination of P50 on the Hbo2
dissociation curve. Validity was ensured by zero-point
calibration using the manufacturer’s rinse solution before
Arterial and Venous Oxygen Saturation
and after each test. Quality control procedures included the
reference method every 8 hours, cleansing the internals of
tubing with appropriate solutions every week, and changing maintenance tubing and tHb calibration every quarter to
ensure test accuracy. To follow the recommended guidelines from a consensus meeting for So2 measurements,46
the cap for the restrictions of 100 percent maximum for So2
and Hbo2 measurements was lifted so that the test results
exceeding 100 percent can be shown as measured by the
equipment. Blood gas and monitor data were recorded
simultaneously with the blood tests.
Clinical monitor readings included pulse oximeter
readings, respiratory rate and heart rate readings, and
incubator temperature and skin temperature readings.
Pulse oximetry saturation readings were recorded by using
a pulse oximeter (Nellcor NPB 290; Tyco HealthCare,
Mansfield, Mass) for all subjects. This instrument was
capable of measuring the percentage of peripheral So2
detected transcutaneously by a probe positioned on either
side of a pulsating arterial bed around the neonate’s foot.
The transmittance sensor was configured so that the lightemitting diodes transmit infrared and red light through the
pulsating vascular bed to a photodetector positioned on the
opposite site.47 The sensors for pulse oximeter were all
placed postductally on infants’ foot. The pulse oximeter
has shown excellent correlations (r = 0.98 –0.99) with
Sao2 without corrections for HbF percentage in neonates48,49 and sound correlations (r = 0.5, 0.88) with
corrections for HbF.7,50 Interrater agreement on data
coding was double-checked to reach 100 percent to ensure
no difference was present between raters.
Procedures
Paired AV blood samples were obtained through UAC
and UVC every 8 hours in coordination with routine
blood gas sampling when neonates were sleeping quietly
to obtain stable measurements. All clinical monitor
readings of vital functions except respiratory rate were
observed to ensure their normal ranges with the blood
sampling. The mean readings of clinical monitors were
Spo2 97.1 F 2.4 percent, 137 F 14.7 beats per minute for
heart rate, 36.4 F 0.83 degrees Celsius for incubator temperature, 36.7 F 0.2 degrees Celsius for skin temperature,
and 41.6 F 19.5 breaths per minutes for respiratory rate.
The hemoximeter test, including HbF determination,
needed less than 0.1 milliliter blood. As part of study
protocol, blood samples were split for the HbF test and the
So2 tests. Fetal hemoglobin determination included
oxygenating blood samples with 100 percent O2 and
twirling the syringe containing the sample between the
hands for 90 seconds to yield fully oxygenated samples.
173
The oxygenation status was confirmed by So2 readings
close to 100 percent. Fetal hemoglobin was then determined by using the hemoximeter. Using this determined
HbF value, the blood So2 test was performed to determine
So2, Hbo2, Hbco, MetHb, and reduced Hb (or deoxyhemoglobin) in paired AV blood samples when routine
blood gas tests were performed.
Data Analysis
Data were examined with AV blood samples for matched
HbF readings. Although the training protocol was used,
some HbF determinations indicated inadequate oxygenation because technical errors were difficult to prevent for
this 24-hour, around-the-clock study, particularly for newer
staff personnel. Without adjusting HbF correctly, Hbco
values were an average of 2 percent higher (r = 0.70, df =
73, P b .001), which caused significant differences between
So2 and Hbo2 measurements.51 Thus, using a 4 percent
criterion,20 unmatched HbF results between AV blood
samples were not included in the analysis. The final sample
included 37 pairs of AV blood samples (1–14 per subject).
Although one neonate provided more samples than others,
no difference was found when the data were compared with
the subject from other subjects.
Data were analyzed by using Statistical Packages for
Social Studies (SPSS, Chicago, Ill). Multivariate linear
mixed model (MLMM) approach51 (maximum likelihood
method for the model estimation and autoregressive model for repeated measurements) was attempted to examine
the differences between the measurements for repeated
measurements of multiple data points from some subjects.
When the levels of the repeated effects were not different
for the observations within the repeated subjects to warrant
the MLMM approach, the original technique of Bland and
Altman52 was used. The MLMM approach51 was an
addition to the original technique reported by Bland and
Altman52,53 to test hypotheses using multivariate level
analyses for repeated measurements. However, the original
technique of Bland and Altman52 still provided additional
useful information and interpretation such as bias and
precision, and limits of agreement. The bias was defined
as the mean difference, and the precision was defines as
the SE of the mean difference. The limits of agreement as
defined by Bland and Altman52 is a proportional function
of distribution for differences between the two measurements. With normal distributions, 67 percent should fall
within F1 SD of the mean difference and 95 percent
should fall within F2 SD of the mean difference, based on
the statistical principles.
Oxygen saturation measurements along the Hbo2
dissociation curves need to be examined for the critical
174
Shyang-Yun Pamela K. Shiao
values in clinical assessment. Oxyhemoglobin dissociations
were examined by using multiple regression (R) curvefitting analysis on sigmoid (S) curve for Po2 values and all
of the So2 measurements of the study (Hbo2, So2, and
Spo2). These curves are useful when examining the relative
values of So2 measurements (So2, Hbo2, and Spo2) against
clinical diagnostic Po2 values for the detection of hypoxemia (b50 millimeters of mercury) and hyperoxemia (N75
millimeters of mercury).
Results
Table 2. Summary Statistics on Mean Difference, SE, and
SDs for SO2 Against HbO2 With Arterial, Venous, and Total
Blood Samples
Parameters
Arterial
Venous
Total
Correlation
Mean difference
SE
F1 SD
Percent total
F2 SD
Percent total
0.96T
2.14T
0.08
F0.49
70.3
F0.97
97.3
1.00T
2.00T
0.07
F0.44
59.5
F0.88
97.3
1.00T
2.07T
0.05
F0.47
67.5
F0.93
97.2
TP b .001.
T
able 1 presents descriptive statistics for hemoximeter
and blood gas analyzer results for general references
and the differences between AV blood samples of these
measurements. The mean difference between AV pairs on
HbF was 0.3 F 1.7 percent and not significant (NS). The
difference for AV Hbco was 0.03 F 0.13 percent (NS),
and the correlation for paired AV Hbco was 0.96 ( P b
.001). The mean difference for AV MetHb was 0.02 F
0.14 percent, and the correlation for paired AV MetHb was
0.52 ( P b .001). The limits of agreement with F2 SD
for the disagreement between AV measurements were
5.4 percent for Hbco and 2.7 percent for MetHb. The
difference for AV So2 was 6 F 7.91 percent ( P b .001)
and the correlation was 0.04 (NS), whereas the difference
for AV Hbo2 was 5.9 F 7.63 percent ( P b .001) and the
correlation was 0.04. For limits of agreement with F2 SD,
the disagreements between AV measurements were
2.7 percent (percent outside the 2 SD) for both So2 and
Hbo2. The low differences between AV So2 (6 percent)
indicated that these neonates had low oxygen to the body
tissue. Carbon monoxide hemoglobin and methemoglobin,
together, on average, accounted for less than 2.3 percent of
total Hb for both AV blood samples (Table 1).
Table 2 presents the differences between measurements
for the accurate So2 measurements. The bias for So2
against Hbo2 was 2.14 F 0.49 percent for arterial samples,
2 F 0.44 percent for venous samples, and 2.07 F
Table 1. Descriptive Statistics and Differences Between AV Blood Samples
Arterial
Venous
Differences
OSM3 hemoximeter
tHb (grams per deciliter)
HbF (percent)
Hbco (percent)
MetHb (percent)
Hbo2 (percent)
RHb (percent)
So2 (percent)
12.9
94.1
1.6
0.7
93.7
4.1
95.8
F
F
F
F
F
F
F
2.24
20.55
0.47
0.14
1.72
1.68
1.72
12.9
93.8
1.5
0.7
87.8
10.0
88.9
F
F
F
F
F
F
F
2.28
20.97
0.44
0.14
7.60
7.60
7.83
0.2
0.3
0.03
0.02
5.9
5.9
6.0
Blood gas analyzer
So2 (percent)
pH
Po2 (millimeters of mercury)
Pco2 (millimeters of mercury)
HCO3 (milliequivalents per liter)
Base excess
94.2
7.4
99.9
35.3
20.8
3.4
F
F
F
F
F
F
4.06
0.06
73.15
5.39
2.77
3.14
80.7
7.3
58.8
37.7
21.0
4.1
F
F
F
F
F
F
12.71
0.09
42.40
5.38
4.55
5.28
13.5 F
0.03 F
41.5 F
2.3 F
0.5 F
1.0 F
Values are presented as mean F SD. RHb indicates reduced Hb.
TP b .001.
TTP b .05.
TTTP b .01.
F
F
F
F
F
F
F
1.41
1.65
0.13
0.14
7.63T
7.76T
7.91T
13.57T
0.07TT
61.83T
1.65TTT
4.05
3.41
Arterial and Venous Oxygen Saturation
Table 3. Summary Statistics on Mean Difference, SE, and
SDs for SpO2 Against SO2 and HbO2 With
Arterial Blood Samples
175
PO2
vHbO2 S-CURVE
PO2
SvO2 S-CURVE
100
98
96
Parameters (percent)
Spo2-So2
Spo2-Hbo2
Correlation
Mean difference
SE
F1 SD
Percent total
F2 SD
Percent total
0.44T
0.96TT
0.45
F2.74
70.3
F5.47
94.6
0.44T
3.10TTT
0.45
F2.73
73
F5.46
94.6
94
92
90
% 88
86
84
82
80
TP b .01.
TTP b .05.
TTTP b .001.
78
76
30
40
50
60
70
80
90
100
PvO2, mm Hg
0.47 percent for total AV blood samples (all P b .001). The
correlation between So2 and Hbo2 was close to 1.0 for all
samples, 0.96 for arterial samples, 1.0 for venous samples,
and 1.0 for total blood samples (all P b .001). For the
limits of agreement within F2 SD, the disagreements
between So2 and Hbo2 were 2.7 percent for both paired
AV samples and 2.8 percent for total samples.
The same analyses were performed for Spo2 and related
measurements. The biases for Spo2 against Sao2 and
arterial Hbo2 were 1 percent ( P b .05) and 3.1 percent ( P b
.001), respectively (Table 3). Therefore, the mean bias for
pulse oximeter readings against the most accurate mea-
PO2
aHbO2 SCURVE
PO2
SaO2 S-CURVE
PO2
SpO2 S-CURVE
100
99
98
97
96
% 95
94
93
92
91
90
50
60
70
80
90
100
PaO2, mm Hg
Fig 1. Arterial Hbo2 sigmoid curves with Pao2 for arterial
Hbo2, Sao2, and Spo2.
Fig 2. Venous Hbo2 sigmoid curves with Pvo2 for venous
Hbo2 and Svo2.
surement using arterial Hbo2 was 3.1 percent. The
correlation between Spo2 and Sao2 was 0.44, and that
between Spo2 and arterial Hbo2 was 0.44 (all P b .01). For
limits of agreement, the disagreements were both 5.4 percent between Spo2 and Sao2, as well as for Spo2 and
arterial Hbo2.
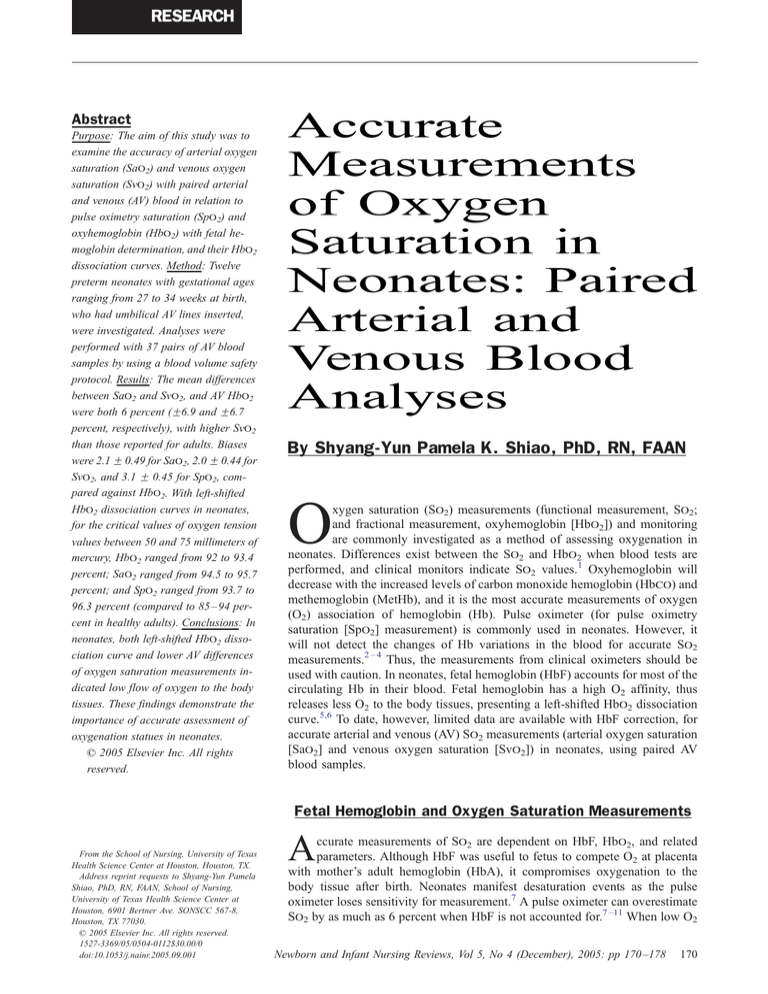
Fig 1 presents the significant So2 dissociation sigmoid
(S) fitted curves for arterial blood samples using multiple
regression curve-fitting approach. For the ease of examinations, the ranges of Pao2 were focused at 100 millimeters of mercury or less. Significant S curves were
established for Hbo2, Sao2, and Spo2 with Pao2. On the
Hbo2 curves, in relation to Po2 ranges of 50 to 75 millimeters of mercury, arterial Hbo2 ranged from 92 to 93.4
percent (R = 0.514, P b .005), Sao2 ranged from 94.5 to
95.7 percent (R = 0.434, P b .01), and Spo2 ranged from
93.7 to 96.3 percent (R = 0.496, P b .01). Fig 2 presents
the significant S curves for venous blood samples, and
Fig 3 presents the significant S curves for the total merged
blood samples. In Fig 2, for venous blood samples, in
relation to venous oxygen tension (Pvo2) ranges of 50 to
75 millimeters of mercury, venous Hbo2 ranged from 88 to
94 percent (R = 0.514, P b .005) and Svo2 ranged from 90
to 96.2 percent (R = 0.801, P b .0001). The best S curves
were produced when both AV blood samples were merged
as the total samples, with greater R and better fit. In Fig 3,
for the total merged blood samples, in relation to Po2
ranges of 50 to 75 millimeters of mercury, Hbo2 ranged
from 88 to 93 percent (R = 0.807, P b .0001) and So2
ranged from 90 to 95 percent (R = 0.802, P b .0001). No
significant S curves were established for Spo2 and Pvo2
176
Shyang-Yun Pamela K. Shiao
PO2
HbO2 S-CURVE
PO2
SO2 S-CURVE
100
98
96
94
92
90
%
88
86
84
82
80
78
76
30
40
50
60
70
80
90
100
PO2, mm Hg
Fig 3. Oxyhemoglobin sigmoid curves for total merged AV
blood samples with Po2 for Hbo2 and So2.
and for Spo2 and Po2 with the total merged blood
samples. No significant correlations were found between
Spo2 and Svo2, or Spo2 and venous Hbo2.
Discussion
I
n these neonates, the mean AV blood differences for
both So2 and Hbo2 were about 6 percent, which was
much lower than those reported for healthy adults
(23 percent) for O2 supply and demand.20-23 In addition,
with very high levels of HbF releasing less O2 to the body
tissue, the results of blood analyses are worrisome for
these critically ill neonates for low systemic oxygen states.
O’Connor and Hall19 determined AV So2 in neonates
without HbF determination. Much of the AV So2
difference is dependent on Svo2 measurement. The ranges
of Svo2 spanned for 35 percent, and the ranges of Sao2
spanned 6 percent in these neonates (Fig 1). The greater
intervals for Svo2 measurements contribute to greater
sensitivity for the measurements (than Sao2 measurements) in responding to nursing care and changes of O2
demand.20,21 Thus, Svo2 measurement is essential for
better assessment of oxygenation status in neonates.
When neonates were resting quietly, the bias between
So2 and Hbo2 was less than 2.5 percent on average with
the correction of HbF factor, with another 1 percent
difference between Spo2 and So2, and slightly greater than
3 percent between Spo2 and Hbo2 measurements. These
findings were comparable to those reported for adults.54
However, blood sampling (either venous or arterial or
both) is needed to accurately determine So2 because
clinical monitors cannot detect changes of Hb variations
for accurate So2 measurements.1,46,54 In summary, the
mean difference between pulse oximetry and blood Hbo2
differed by 3.1 percent. The differences between the
measurements could become greater as neonates develop
desaturation events.7
The paired AV blood samples are difficult to obtain,
especially when ensuring safety concerns for blood
volumes in these vulnerable neonates, with accurate
measurements. These delicate blood analyses require
dedications of conscientious staff personnel. Repeated
practices using simulated solutions and volunteer adult
blood1 before handling neonates’ blood yielded the
precision limits better than 0.1 percent limit recommended
by the manufacturer’s standards, indicating successful
training of staff personnel, excluding unmatched AV pairs.
Precision (SE) is a common indicator of accuracy for
instruments in marketing by manufacturers. The precision
for clinical Spo2 against both So2 and Hbo2 was
0.45 percent, which was at least five times less precise
than the blood analyses. These findings confirmed that
clinical pulse oximeters cannot demonstrate the same
precision standards as the benchtop instruments.54
On the sigmoid curves, the ranges of So2 readings in
relation to Pao2 were much narrower for these neonates,
when compared with that for adults. As compared with
the ranges of 95 to 84 percent Spo2 in adults,18,47 for the
Pao2 ranges from 50 to 75 millimeters of mercury, the
ranges of So2 measurements in neonates were higher and
narrower (about 94 to 96.3 percent for Spo2, 94.5 to 95
percent for Sao2, and 92 to 93.4 percent for arterial
Hbo2). In relation to 50 millimeters of mercury of Pao2
measurement on the Hbo2 dissociation curve, critical So2
ranges of 92 to 94 percent were identified for neonates.
With the limited accuracy capacity of pulse oximetry in
neonates during desaturation events, it is preferable to
keep the Sao2 and Spo2 measurements at greater than 92
to 94 percent. These narrower ranges of So2 measurements require clinicians to exercise more careful and
closer observations to assess critical changes of oxygenation conditions in neonates.
The findings of this study on AV differences of So2
were limited with very small number of paired AV blood
samples. However, critically ill neonates need accurate
assessment of oxygenation status because of HbF, which
releases less O2 to the tissues. Decreased differences of AV
So2 measurements added further possibilities of lower
flow of O2 to the body tissues and demonstrated the
greater need to accurately assess the proper oxygenation in
the neonates. The findings of this study continued to
Arterial and Venous Oxygen Saturation
clarify the accuracy of So2 measurements for neonates.
Additional studies are needed to examine So2 levels in
neonates to further validate these findings by using larger
sample sizes.
Acknowledgments
T
hree different awards support this study in part: KCIAACN Critical Care Research Award from the
American Association of Critical Care, Aliso Viejo, CA;
Research Award from the National Association of Neonatal Nurses, Glenview, IL; and the National Institutes of
Health, R01-NR04447, Bethesda, MD. The author
acknowledges the nurses, physicians, and respiratory
therapists who participated and helped with the blood
sample collection at the clinical settings.
References
1. Shiao S-YPK: Functional versus fractional oxygen saturation
readings: bias and agreement using simulated solutions and adult blood.
Biol Res Nur 3:210 – 221, 2002
2. Harris AP, Sendak MJ, Donham RT, et al: Absorption characteristics of human fetal hemoglobin at wavelengths used in pulse oximetry.
J Clin Monit 4:175 – 177, 1988
3. Moyle JT: Uses and abuses of pulse oximetry. Arch Dis Child
74:77 – 80, 1996
4. Rausch-Madison S, Mohsenifar Z: Methodologic problems
encountered with cooximetry in methemoglobinemia. Am J Med Sci
314:203 – 206, 1997
5. Wimberly PD: Oxygen monitoring in the newborn. Scand J Clin
Lab Invest 127 – 130, 1993 (54 Suppl 214)
6. Wimberly PD, Siggaard-Anderson O, Fogh-Anderson N: Accurate measurement of hemoglobin oxygen saturation, and fraction of
carboxyhemoglobin and methemoglobin in fetal blood using Radiometer
OSM3: corrections for fetal hemoglobin fraction and pH. Scand J Clin
Lab Invest 235 – 239, 1990 (50 Suppl 203)
7. Shiao S-YPK: Desaturation events in neonates during mechanical
ventilation. Crit Care Nurs Q 24:14 – 29, 2002
8. Blaisdell CJ, Goodman S, Clark K, et al: Pulse oximetry is a poor
predictor of hypoxemia in stable children with sickle cell disease. Arch
Pediatr Adolesc Med 154:900 – 903, 2000
9. Carter BG, Carlin JB, Tibballs J, et al: Accuracy of two pulse
oximeters at low arterial hemoglobin-oxygen saturation. Crit Care Med
26:1128 – 1133, 1998
10. Rajadurai VS, Walker AM, Yu VY, et al: Effect of fetal
haemoglobin on the accuracy of pulse oximetry in preterm infants. J
Paediatr Child Health 28:43 – 46, 1992
11. Whyte RK, Jangaard KA, Dooley KC: From oxygen content to
pulse oximetry: completing the picture in the newborn. Acta Anaesthesiol
Scand Suppl 107:95 – 100, 1995
12. Bucher H-U, Fanconi S, Beeckert P, et al: Hyperoxemia in
neuborn infants: detection by pulse oximetry. Pediatrics 84:226 – 230,
1989
13. Poets CF, Wilken M, Seidenberg J, et al: Reliability of a
pulse oximeter in the detection of hyperoxemia. J Pediatr 122:87 – 90,
1993
14. Trivedi NS, Ghouri AF, Lai E, et al: Pulse oximeter performance
during desaturation and resaturation: a comparison of seven models.
J Clin Anesth 9:184 – 188, 1997
177
15. Trivedi NS, Ghouri AF, Shah NK, et al: Effects of motion,
ambient light, and hypoperfusion on pulse oximeter function. J Clin
Anesth 9:179 – 183, 1997
16. Hohl RJ, Sherburne AR, Feeley JE, et al: Low pulse oximeter–
measured hemoglobin oxygen saturation with Hb Cheverly. Am J
Hematol 59:181 – 184, 1998
17. Askin DF: Interpretation of neonatal blood gases, part II:
disorders of acid-bas balance. Neonatal Netw 16:23 – 28, 1997
18. Grossbach I: Case studies in pulse oximetry monitoring. Crit Care
Nurse 13:63 – 65, 1993
19. O’Connor TA, Hall RT: Mixed venous oxygenation in critically
ill neonates. Crit Care Med 22:343 – 346, 1994
20. Chulay M, Palmer J, Neblett J, et al: Clinical comparison of twoand three-wavelength systems for continuous measurement of venous
oxygen saturation. Am J Crit Care 1:69 – 75, 1992
21. Nakanishi N, Yoshioka T, Okano Y, et al: Continuous Fick
cardiac output measurement during exercise by monitoring of mixed
venous oxygen saturation and oxygen uptake. Chest 104:419 – 424, 1993
22. Siggaard-Andersen O, Gothgen IH: Oxygen and acid-base
parameters of arterial and mixed venous blood, relevant versus redundant.
Acta Anaesthesiol Scand Suppl 107:21 – 27, 1995
23. Whyte RK: Mixed venous oxygen saturation in the newborn:
can we and should we measure it. Scand J Clin Lab Invest 203 – 211,
1990 (50 Suppl 203)
24. Hirschl RB, Palmer P, Heiss KF, et al: Evaluation of right arterial
venous oxygen saturation as a physiologic monitor in a neonatal model.
J Pediatr Surg 28:901 – 905, 1993
25. Hampson NB: Pulse oximetry in severe CO poisoning. Chest
114:1036 – 1041, 1998
26. Haney M, Tait AR, Tremper KK: Effect of carboxyhemoglobin
on the accuracy of mixed venous oximetry monitors in dogs. Crit Care
Med 22:1181 – 1185, 1994
27. Touger M, Gallagher EJ, Tyrell J: Relationship between venous
and arterial HbCO levels in patients with suspected carbon monoxide
poisoning. Ann Emerg Med 25:481 – 483, 1995
28. Lopez DM, Weingarten-Arams JS, Singer LP, et al: Relationship
between arterial, mixed venous, and internal jugular HbCO concentrations at low, medium, and high concentrations in a piglet model of CO
toxicity. Crit Care Med 28:1998 – 2001, 2000
29. Meyer J, Prien T, Van Aken H, et al: Arterio-venous carboxyhemoglobin difference suggests carbon monoxide production by human
lungs. Biochem Biophys Res Commun 244:230 – 232, 1998
30. Zhen G, Xue Z, Zhang Z, et al: Carbon monoxide inhibits
proliferation of pulmonary smooth muscle cells under hypoxia. Chin Med
J 116:1804 – 1809, 2003
31. Weber TP, Gross-Hartlage MA, Meyer J, et al: Arteriovenous
carboxyhemoglobin gradient is a technical artifact that is eliminated by
special calibration (SAT 100). Biochem Biophys Res Commun 278:
447 – 448, 2000
32. Burke-Martindale CH: Inhaled nitric oxide therapy for adult
respiratory distress syndrome. Crit Care Nurse 18:21 – 27, 1998
33. Dotsch J, Demirakca S, Hamm R, et al: Extracorporeal circulation
increases nitric oxide–induced methemoglobinemia in vivo and in vitro.
Crit Care Med 25:1153 – 1158, 1997
34. Crawford JH, White CR, Patel RP: Vasoactivity of S-nitrosohemoglobin: role of oxygen, heme, and NO oxidation states. Blood
101:4408 – 441519, 2003
35. Zavodnik IB, Lapshina EA, Rekawiecka K, et al: Membrane
effects of nitrite-induced oxidation of human red blood cells. Biochem
Biophys Acta 1421:306 – 316, 1999
36. Huang Z, Louderback JG, Goyal M, et al: Nitric oxide biding to
oxygenated hemoglobin under physiological conditions. Biochem Biophys Acta 1568:252 – 260, 2001
37. Mishra OP, Akhter W, Ashraf QM, et al: Hypoxia-induced
modification of poly (ADP-ribose) polymerase and DNA polymerase B
activity in cerebral cortical nucliei of newborn piglets: role of nitric oxide.
Neuroscience 119:1023 – 1032, 2003
38. Spandou E, Papoutsopoulou S, Soubasi V, et al: Hypoxiaischemia affects erythropoietin and erythropoietin receptor expression
pattern in the neonatal rate brain. Brain Res 1021:167 – 172, 2004
178
Shyang-Yun Pamela K. Shiao
39. Fellman V, Raivio KO: Reperfusion injury as the mechanism of
brain damage after perinatal asphysia. Pediatr Res 41:599 – 606, 1997
40. Zhao J, Liu X-J, Ma J-W, et al: DNA damage in healthy term
neonate. Early Hum Dev 77:89 – 98, 2004
41. Nemeto S, Aoki M, Dehua C, et al: Free hemoglobin impairs
cardiac function in neonatal rabbit heart. Ann Thorac Surg 69:1484 – 1489,
2000
42. Hirano K, Morinobu T, Kim H, et al: Blood transfusion increases
radical promoting non-transferrin bound iron in preterm infants. Arch Dis
Child Fetal Neonatal Ed 84:F188 – F193, 2001
43. Bard H, Widness JA: The life span of erythrocytes transfused to
preterm infants. Pediatr Res 42:9 – 11, 1997
44. Corwin HL: Anemia in the critically ill: the role of erythropoietin.
Semin Hematol 38:24 – 32, 2001 (3 Suppl 7)
45. Krzeminski A: How is fetal hemoglobin determined and
corrected for in the OSM3, the ABL510, and the ABL 520? Radiometer
Copenhagen; May 1992. Info, No:1992-4,1-4
46. Ehrmeyer S, Burnett RW, Chatburn RL, et al: Fractional
oxyhemoglobin, oxygen content and saturation, and related quantities
in blood: terminology, measurement, and reporting; Approved guidelines.
NCCLS; January 1997:C25-A17(3)
47. Yelderman M, New W: Evaluation of pulse oximetry. Anesthesiology 59:349 – 352, 1985
48. Barrington KJ, Finer NN, Ryan CA: Evaluation of pulse oximetry
as a continuous monitoring technique in the neonatal intensive care unit.
Crit Care Med 16:1147 – 1153, 1988
49. Hay Jr WW, Brockway JM, Eyzaguirre M: Neonatal pulse
oximetry: accuracy and reliability. Pediatrics 83:717 – 722, 1989
50. Rajadural VS, Walker AM, Yu VY, et al: Effect of fetal
hemoglobin on the accuracy of pulse oximetry in preterm infants. J
Paediatr Child Health 28:43 – 46, 1992
51. Lai D, Shiao S-YPK: Comparing two clinical measurements: a
linear mixed model approach. J Appl Stat [In Press]
52. Bland JM, Altman DG: Statistical methods for assessing
agreement between two methods of clinical measurement. Lancet
1:307 – 310, 1986
53. Bland JM, Altman DG: Measuring agreement in method
comparison studies. Stat Methods Med Res 8:161 – 179, 1999
54. Smatlak P, Knebel AR: Clinical evaluation of noninvasive
monitoring of oxygen saturation in cirtically ill patients. Am J Crit Care
7:370 – 373, 1998