The Effect of Extracorporeal Life Billie Lou Short, MD
advertisement
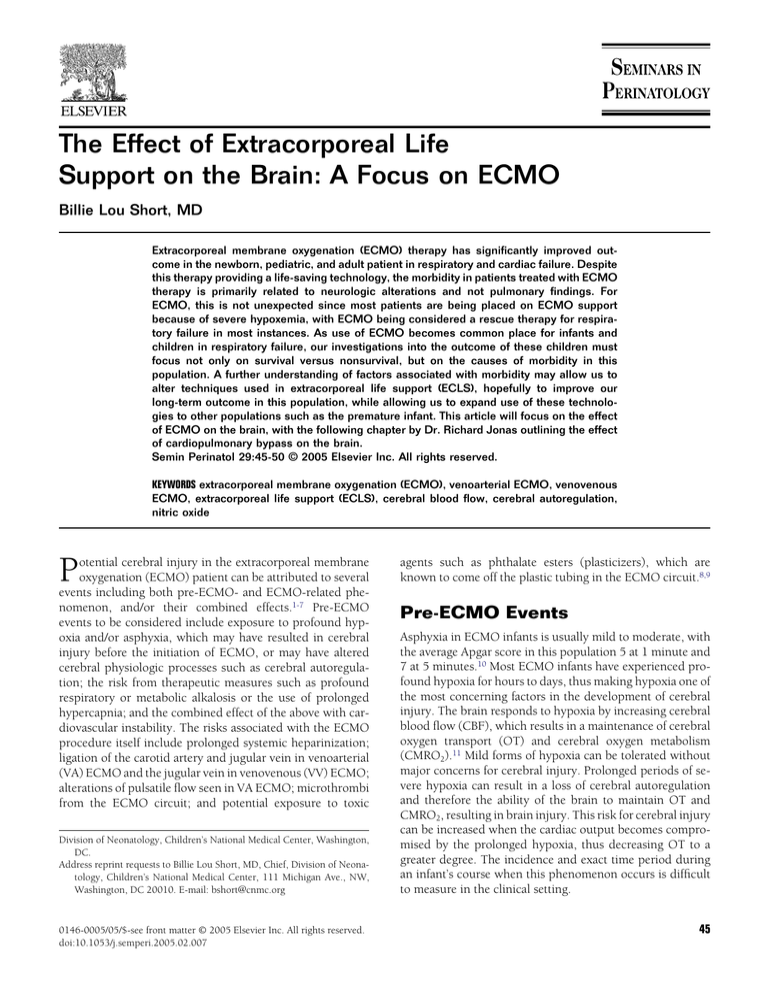
The Effect of Extracorporeal Life Support on the Brain: A Focus on ECMO Billie Lou Short, MD Extracorporeal membrane oxygenation (ECMO) therapy has significantly improved outcome in the newborn, pediatric, and adult patient in respiratory and cardiac failure. Despite this therapy providing a life-saving technology, the morbidity in patients treated with ECMO therapy is primarily related to neurologic alterations and not pulmonary findings. For ECMO, this is not unexpected since most patients are being placed on ECMO support because of severe hypoxemia, with ECMO being considered a rescue therapy for respiratory failure in most instances. As use of ECMO becomes common place for infants and children in respiratory failure, our investigations into the outcome of these children must focus not only on survival versus nonsurvival, but on the causes of morbidity in this population. A further understanding of factors associated with morbidity may allow us to alter techniques used in extracorporeal life support (ECLS), hopefully to improve our long-term outcome in this population, while allowing us to expand use of these technologies to other populations such as the premature infant. This article will focus on the effect of ECMO on the brain, with the following chapter by Dr. Richard Jonas outlining the effect of cardiopulmonary bypass on the brain. Semin Perinatol 29:45-50 © 2005 Elsevier Inc. All rights reserved. KEYWORDS extracorporeal membrane oxygenation (ECMO), venoarterial ECMO, venovenous ECMO, extracorporeal life support (ECLS), cerebral blood flow, cerebral autoregulation, nitric oxide P otential cerebral injury in the extracorporeal membrane oxygenation (ECMO) patient can be attributed to several events including both pre-ECMO- and ECMO-related phenomenon, and/or their combined effects.1-7 Pre-ECMO events to be considered include exposure to profound hypoxia and/or asphyxia, which may have resulted in cerebral injury before the initiation of ECMO, or may have altered cerebral physiologic processes such as cerebral autoregulation; the risk from therapeutic measures such as profound respiratory or metabolic alkalosis or the use of prolonged hypercapnia; and the combined effect of the above with cardiovascular instability. The risks associated with the ECMO procedure itself include prolonged systemic heparinization; ligation of the carotid artery and jugular vein in venoarterial (VA) ECMO and the jugular vein in venovenous (VV) ECMO; alterations of pulsatile flow seen in VA ECMO; microthrombi from the ECMO circuit; and potential exposure to toxic Division of Neonatology, Children’s National Medical Center, Washington, DC. Address reprint requests to Billie Lou Short, MD, Chief, Division of Neonatology, Children’s National Medical Center, 111 Michigan Ave., NW, Washington, DC 20010. E-mail: bshort@cnmc.org 0146-0005/05/$-see front matter © 2005 Elsevier Inc. All rights reserved. doi:10.1053/j.semperi.2005.02.007 agents such as phthalate esters (plasticizers), which are known to come off the plastic tubing in the ECMO circuit.8,9 Pre-ECMO Events Asphyxia in ECMO infants is usually mild to moderate, with the average Apgar score in this population 5 at 1 minute and 7 at 5 minutes.10 Most ECMO infants have experienced profound hypoxia for hours to days, thus making hypoxia one of the most concerning factors in the development of cerebral injury. The brain responds to hypoxia by increasing cerebral blood flow (CBF), which results in a maintenance of cerebral oxygen transport (OT) and cerebral oxygen metabolism (CMRO2).11 Mild forms of hypoxia can be tolerated without major concerns for cerebral injury. Prolonged periods of severe hypoxia can result in a loss of cerebral autoregulation and therefore the ability of the brain to maintain OT and CMRO2, resulting in brain injury. This risk for cerebral injury can be increased when the cardiac output becomes compromised by the prolonged hypoxia, thus decreasing OT to a greater degree. The incidence and exact time period during an infant’s course when this phenomenon occurs is difficult to measure in the clinical setting. 45 B.L. Short 46 Figure 1 Lower end of an autoregulation curve in newborn lambs after 2 hours of exposure to hypoxia (SaO2 40%). Control animals (diamond) maintain autoregulation to a cerebral perfusion pressure (CPP) of 25 mm Hg, while animals exposed to hypoxia and then recovered by turning the ventilator FIO2 to maintain normoxia (square) lost autoregulation at a CPP of 25 to 39 mm Hg (P ⱕ 0.05). Animals recovered using ECMO to maintain normoxia (triangle) loss autoregulation at a CPP of 40 to 55 mm Hg (P ⱕ 0.05). Systemic insults such as severe asphyxia, hypoxia, and hypercarbia can disrupt cerebral autoregulation leaving the cerebral microcirculation vulnerable to alterations in systemic blood pressure.12-15 In this state, hypotension can result in ischemic cerebral damage, whereas hypertension can cause cerebral hyperemia and thus the risk for cerebral hemorrhage. Loss of autoregulation in an already injured brain, in the presences of systemic heparinization, such as occurs with ECMO, can result in cerebral hemorrhage. Tweed and coworkers and Short and coworkers have demonstrated in the newborn lamb that exposure to prolonged hypoxia resulted in loss of cerebral autoregulation during the recovery phase from hypoxia.16,17 In the study by Tweed and coworkers, a 20-minute exposure to a PaO2 of 30 torr resulted in loss of cerebral autoregulation for 6 hours after the hypoxic insult. Short and coworkers exposed newborn lambs to 2 hours of severe hypoxia (SaO2s of 40%) combined with carotid artery and jugular vein ligation, simulating that seen in pre-ECMO events. Cerebral autoregulation was evaluated 1 hour after the hypoxic insult and found to be altered. When recovery from hypoxia was done by placing the animal on ECMO instead of increasing FIO2 in the ventilator, the effect on cerebral autoregulation was even more profound (see Fig. 1). Of more concern was the finding that, at the cerebral perfusion pressure level that CBF decreased, significant differences in right-to-left CBF were noted, indicating that if a pathophysiologic event such as hypotension would occur during this period, then vessel ligation may be a risk factor for unilateral cerebral injury. Supporting this concern was the observation that CMRO2 also decreased at this point, indicating the potential for cerebral injury. Ashwal and coworkers have also shown in the fetal lamb that the hyperemic, posthypoxia state lasts 4 hours after recovery from the hypoxia.18 These animal studies with those of Short and Tweed all indicate that the brain may be vulnerable to further insults such as hypotension and/or hyperten- sion during the recovery period from severe hypoxia, and that this high risk period can be quite prolonged. Exposure in these studies was relatively short-term, making concern for the actual length of this vulnerable time in the ECMO patient who has been exposed to hours and days of hypoxia of great concern. Other factors placing these infants at risk for intracranial injury can be our clinical management, with specific concerns for our respiratory management of these infants, ie, hyperventilation or gentle ventilation with hypercapnia. Although controversial, hyperventilation is still used in some infants with pulmonary hypertension today.19 Alkalosis can be achieved by either respiratory or metabolic means. If respiratory alkalosis is used, the effect of lowering systemic pCO2 on the cerebral circulation must be taken into account. As hyperventilation causes vasodilation in the pulmonary bed, it causes vasoconstriction in the cerebral circulation, which can reduce cerebral blood flow. Outcome studies evaluating infants treated with severe hyperventilation, although small, indicate that neurodevelopmental outcome can be adversely affected by this therapy.20-22 Several studies in animals evaluating the effect of hyperventilation on the brain have shown an initial decrease of 20% to 30%, with normalization of the CBF after 4 to 6 hours of hyperventilation. Gleason and coworkers, in the newborn lamb, showed this same pattern with hyperventilation, but extended the study to evaluate the posthyperventilation period.23 In their model, after 6 hours of hyperventilation, animals were made acutely normocarbic, simulating what happens when placing an infant on ECMO. At this point, extreme hyperemia occurred, with an increase in CBF by 104%. This hyperemia lasted for the remaining 90 minutes of the study. Since the study did not extend beyond 90 minutes, the exact period needed to normalize the CBF after normalization of pCO2 was not determined. As a result of this study, we now normalize the patient’s pCO2 over a 24-hour period. The exact period needed to accomplish this safely is unknown. Hino and coworkers studied the effect on CBF of acute normalization of pCO2 after exposure to prolonged hypercapnia24 in the newborn lamb. It could be hypothesized that a period of cerebral ischemia might occur. Although CBF increased dramatically during hypercarbia (a normal reaction), normalization of pCO2 did not result in ischemia. Although these finding were assuring, for many centers are now changing respiratory management to include a “gentle ventilation” or hypercapnic approach to therapy pre-ECMO, only CBF was studied, not the effect of this prolonged hypercarbia on cerebral autoregulation. ECMO Risk Factors When infants are being placed on VA ECMO, there is a time period during cannulation that the infant is still hypoxic, and both the carotid artery and jugular vein must be ligated as the catheters are placed. Short and coworkers undertook a study in newborn lambs to determine whether this combination of exposure to prolonged hypoxia (4 hours) followed by vessel ligation altered cerebral blood flow and metabolism.25 In this ECMO and the brain study, after exposure to 4 hours of an arterial PaO2 of 40 torr, either the jugular vein or carotid artery was ligated (randomized to determine the effect of ligation of each separately), followed by the opposite vessel ligated (evaluating the effect of ligation of both the carotid artery and jugular vein). The results showed that this degree of hypoxia caused a 100% increase in CBF with maintenance of OT and CMRO2, and that during this hyperemic period, ligation of either the carotid artery, jugular vein, or both did not alter CBF, OT, or CMRO2. Klein and associates also evaluated the effect of vessel ligation on the brain.26 MRI studies immediately post study in this same model did not reveal any difference in the ligated and nonligated animals. Although the results of this study are reassuring, it does not address the events which may occur if other pathophysiologic events are superimposed during this period, such as systemic hypotension or hypertension. Concerns of the potential effect of the ECMO procedure itself on the brain have been observed both clinically and in the laboratory. Outcome studies showing that most ECMO deaths are not secondary to respiratory causes, but to intracranial hemorrhage, have made many investigators attempt to evaluate the timing and type of intracranial hemorrhage, and the relationship of ICH to clinical and ECMO events. A full discussion of the risk associated with ICH and neurodevelopmental outcome of the ECMO population is outlined in this series by Bulas and Glass.27 The concern for ligation of the carotid artery resulted in the development of the single-double lumen venovenous catheter, and the use of VV ECMO. It is of interest that both Doppler blood flow studies and angiographic evaluation of the brain by magnetic resonance have shown antegrade flow in the carotid artery and/or the circle of Willis in 35% to 50% of infants with permanent ligation of the carotid artery.28-31 These findings indicate that collateral flow can develop quite quickly in these infants. The only long-term follow-up study to date evaluating flow in the right internal carotid artery of post-VA-ECMO children has been conducted by Lott and coworkers. In this study, although there was flow on the right, it was reduced by 74%.28 Lohrer and associates examined blood flow velocities of the internal carotid artery in VA ECMO patients before, during, and after ECMO.29 Changes in carotid blood flow velocities did not correlate with major intracranial insults. Perlman and coworkers examined the cerebral blood flow patterns in infants post-VA ECMO using positron emission tomography and found symmetric hemispheric CBF.31 Serial electroencephalographic (EEGs) studies were performed in infants before and while on ECMO by Streletz and coworkers.32 Their findings corroborate that of neuroimaging data that no acute change in EEG rhythm or amplitude over the right hemisphere was noted after ligation, or during ECMO, with their conclusion that carotid ligation in the short-term is a safe procedure. VV ECMO has its own risk. Although the carotid artery is spared, the internal jugular vein must still be ligated and there are concerns for the obstructive nature of the large venovenous catheter to superior vena cava flow. A high incidence of posterior-fossa hemorrhages in the ECMO popula- 47 Figure 2 Doppler flow changes see in the pericallosal artery of an infant pre-ECMO and while on ECMO. The increase in diastolic flow is secondary to flow from the nonpulsatile ECMO pump. Studies indicate that this change alters the endothelial production of nitric oxide, and thus alters vasodilation in vessels exposure to this shear stress/flow changes. tion have made the concern for venous congestion secondary to ligation of this vessel a concern.33,34 Another phenomenon which has been noted in the ECMO population pointing toward venous congestion is the high incidence of widened interhemispheric fissure seen on CT scans in as many as 68% of patients treated with VV ECMO.35 This incidence in VV ECMO is much greater then that seen in VA ECMO, where it has been reported to be only 5% to 10%,33 raising further concerns for venous congestion caused by the VV catheter. The exact etiology of this finding and the long-term consequences of this observation are unknown. Doppler studies of the pericallosal artery of infants on VAECMO showed a significant change in diastolic flow velocities as seen in Fig. 2, representing the effect of the nonpulsatile flow coming from the ECMO pump. When cerebral blood flow changes were compared with left ventricular output data, in a study conducted by Taylor and coworkers, in VA ECMO infants, as suspected, left ventricular output decreased as the pump flows were increased, and that with this change, the anterior cerebral artery pulsatility index decreased.36,37 These findings also indicate the effect of the takeover of cardiac output by the nonpulsatile ECMO pump. These findings are not seen in VV ECMO, where the heart acts as the pump.38 The effect of this altered blood flow pattern in VA ECMO on brain is not fully understood, but may play a role in the altered cerebral autoregulation seen secondary to ECMO as described in the next section. Key physiologic studies on the effect of ECMO on the brain include the initiation of both VA and VV ECMO, CO2 responsiveness of the brain while on ECMO, cerebral autoregulation on ECMO, the initiation of ECMO after exposure to hypoxia, and the combined effect of pre-ECMO exposure to hypoxia and recovery from hypoxia using ECMO, on cerebral autoregulation.39-43 Initial findings by Short and coworkers, of the acute effects of initiation of VA ECMO on brain did not show 48 Figure 3 The effect of intraluminal acetylcholine infusion on vascular diameter in control, nonpulsatile (VA) and pulsatile (VV) ECMO. Vasodilation is noted in the vessels from control and VV ECMO animals, with vasoconstriction in vessels exposed to VA or nonpulsatile ECMO, indicating altered endothelial reactivity.45 altered CBF, CMRO2, cerebral OT, or cerebral oxygen extraction.39 These studies were conducted at ECMO flows of 150 mL/kg/min. Studies by Rosenberg and Kinsella, at ECMO flow rates ⬍100 mL/kg/min, showed a drop in CBF.40 The differences in flow rates may be responsible for the differing findings between these studies. In the newborn VA ECMO lamb model, Walker and coworkers were able to show that CO2 reactivity of the brain was preserved while on VA ECMO.41 Short and coworkers, in the same lamb model, evaluated the effect on cerebral autoregulation of exposure to VA ECMO.42 One hour of exposure to VA ECMO in the healthy newborn lamb resulted in alteration of cerebral autoregulation. As seen with hypoxia, when CBF decreased in this study, right-to-left blood flow differences were seen. Although autoregulation changes were seen in VV ECMO, they were less severe than those seen in VA ECMO, and no right–left CBF differences were noted.43 Studies by Russo and coworkers, using the closed cranial window (pial cerebral artery method) technique, corroborated findings by Short and coworkers. In their study, cerebral arteriolar vasodilatation during VA ECMO was markedly altered (data presented at the 6th Annual ELSO Meeting, October 1994). Further studies by Short and colleagues in isolated vessel chamber studies have shown that VA ECMO significantly alters vessel reactivity to acetylcholine (an endothelial-dependent vasodilator), while VV ECMO does not alter this reactivity (Fig. 3). The vasoconstrictive effect of exposure to NG-nitro-L-arginine methyl ester (L-NAME, a potent blocker of nitric oxide production) was markedly blunted in cerebral arteries from animals exposed to VA ECMO compared with controls with normal pulsatility (Fig. 4).44 These findings indicate that the flow and shear stress changes in VA ECMO may alter endothelial reactivity through alterations in the nitric oxide pathway (Fig. 2).45 This alteration may be responsible for the altered autoregulatory changes seen in the VA ECMO animals. This hypothesis has been corroborated by findings that the altered vessel reactivity can be returned B.L. Short Figure 4 The effect of the intraluminal infusion of LG-nitro-L-arginine methyl ester (L-NAME) on vascular diameter in control and nonpulsatile VA ECMO animals. Control animals had a significant vasoconstrictive response compared with animals exposed to VA ECMO (P ⱕ 0.05), indicating an altered production of nitric oxide in the vessels of animals exposed to VA ECMO.44 to normal after exposure to a nitric oxide donor (see Fig. 5). Other studies indicating endothelial dysfunction have been noted in a hypothermic lamb model of cardiopulmonary bypass.46 Autoregulation changes have been related to endothelial alterations caused by pressure changes in a piglet model studied by Martinez-Orgado and colleagues.47 Peckel and colleagues showed an altered autoregulatory response after Figure 5 The effect of the nitric oxide donor, 3-morpholinyl sydnonelmine chloride (SIN-1), on vessel diameter, comparing vessels from control animals (white bar), vessels from animals exposed to VA ECMO (black bar), and vessels from animals exposure to VV ECMO (hatch bar). The increased vasodilation in the VA ECMO vessels indicates that these vessels have an altered production of nitric oxide, with marked vasodilation after replacement of nitric oxide with SIN-145 ECMO and the brain nitric oxide blockage in their rat model, implicating endothelial dysfunction.48 ECMO and the Brain: Conclusions In summary, ECMO infants are at risk for cerebral injury secondary to their critical pre-ECMO state, and possibly from the ECMO therapy itself. The animal studies described in this chapter indicate that the recovery period from hypoxia, whether with or without ECMO, is a vulnerable period, where physiologic alterations such as hypotension or hypertension may place the brain at risk for injury. If these studies in ECMO animals can be extrapolated to the newborn human infant, VA ECMO may increase this risk, indicating that stabilization of the infant during the initial recovery period on ECMO, and treatment of such events such as hypertension and hypotension, should be undertaken in an expedient manner. Further studies are needed to understand the mechanisms of these alterations, which would hopefully allow us to alter our therapies such that this potential risk could be decreased. Acknowledgment This work is supported in part by: NINDS, 1R21NS4038101A2, PI: BL Short. References 1. Bulas DI, Taylor GA, O’Donnell, et al: Intracranial abnormalities in infants treated with extracorporeal membrane oxygenation: update on sonographic and CT findings. Am J Neuroradiol 17:287-294, 1996 2. Glass P, Bulas DI, Wagner AE, et al: Severity of brain injury following neonatal extracorporeal membrane oxygenation and outcome at age 5 years. Dev Med Child Neurol 39:441-448, 1997 3. Graziani LJ, Gringlas M, Baumgart S: Cerebrovascular complications and neurodevelopmental sequelae of neonatal ECMO. Clin Perinatol 24:655-675, 1997 4. Vaucher YE, Dudell GG, Bejar R, et al: Predictors of early childhood outcome in candidates for extracorporeal membrane oxygenation. J Pediatr 128:109-117, 1996 5. Glass P, Miller M, Short BL: Morbidity for survivors of extracorporeal membrane oxygenation: neurodevelopmental outcome at 1 year of age. Pediatrics 83:72-78, 1989 6. Schumacher RE, Palmer TW, Roloff DW, et al: Follow-up of infants treated with extracorporeal membrane oxygenation for newborn respiratory failure. Pediatrics 87:451-457, 1991 7. Hofkosh D, Thompson AE, Nozza RJ, et al: Ten years of extracorporeal membrane oxygenation: neurodevelopmental outcome. Pediatrics 87: 549-555, 1991 8. Karle VA, Short BL, Martin GR, et al: Extracorporeal membrane oxygenation (ECMO) exposes infants to the plasticizer Di(2-ethylhexyl) phthalate (DEHP). Crit Care Med 25:696-703, 1997 9. Schneider B, Schena J, Troug R, et al: Exposure to Di(2-ethyl-hexyl)phthalate in infants receiving extracorporeal membrane oxygenation. N Engl J Med 78:699 (letter), 1989 10. Stolar CJH, Snedecor SM, Bartlett RH: Extracorporeal membrane oxygenation and neonatal respiratory failure: experience from the extracorporeal life support organization. J Pediatr Surg 26:563-571, 1991 11. Jones MD, Hudak ML: Regulation of the fetal cerebral circulation, in Polin RA, Fox WW (eds): Fetal and Neonatal Physiology. Philadelphia, PA, W.B. Saunders, 1992, pp 682-690 12. Lassen NA: Autoregulation of cerebral blood flow. Circ Res 14:I-201I-204, 1964 (suppl 1) 49 13. Paulson OB, Walseman G, Schmidt JF, et al: Cerebral circulation under normal and pathologic conditions. Am J Cardiol 63:2C-5C, 1989 14. Standgaard S, Paulson OB: Cerebral autoregulation. Stroke 15:413415, 1984 15. Papile LA, Rudolph AM, Heymann MA: Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 19:159-161, 1985 16. Tweed A, Cote J, Lou H, et al: Impairment of cerebral blood flow autoregulation in the newborn lamb by hypoxia. Pediatr Res 20:516519, 1986 17. Short BL, Walker LK, Traystman RJ: Impaired cerebral autoregulation in the newborn lamb during recovery from severe, prolonged hypoxia, combined with carotid artery and jugular vein ligation. Crit Care Med 22:1262-1268, 1994 18. Ashwal S, Majcher JS, Longo L: Patterns of fetal lamb regional cerebral blood flow during and after prolonged hypoxia: studies during the posthypoxia recovery period. Am J Obstet Gynecol 14:1104-1110, 1981 19. Wlash-Sukys MC, Cornell DJ, Houston LN, et al: Treatment of persistent pulmonary hypertension of the newborn without hyperventilation: an assessment of diffusion of innovation. Pediatrics 94:303-306, 1994 20. Bifano EM, Pfannenstiel A: Duration of hyperventilation and outcome in infants with persistent pulmonary hypertension. Pediatrics 81:657661, 1988 21. Gannon CM, Wiswell TE, Spitzer AR: Volutrauma, PaCO2 levels, and neurodevelopmental sequelae following assisted ventilation. Clin Perinatol 25:159-175, 1998 22. Sell EJ, Gaines JA, Gluchman C, et al: Persistent fetal circulation: neurodevelopmental outcome. Am J Dis Child 139:25-28, 1985 23. Gleason CA, Short BL, Jones DM: Cerebral blood flow and metabolism during and after prolonged hypocapnia in newborn lambs. J Pediatr 115:309-314, 1989 24. Hino JK, Short BL, Rais-Bahrami K, et al: Cerebral blood flow and metabolism during and after prolonged hypercapnia in newborn lambs. Crit Care Med 28:3505-3510, 2000 25. Short BL, Bender K, Walker LK, et al: The cerebrovascular response to prolonged hypoxia with carotid artery and jugular vein ligation in the newborn lamb. J Pediatr Surg 29:887-891, 1994 26. Klein MD, Lessin MS, Whittlesey GC, et al: Carotid artery and jugular vein ligation with and without hypoxia in the rat. J Pediatr Surg 32: 565-570, 1997 27. Glass P, Bulas D: Neonatal ECMO: neuroimaging and neurodevelopmental outcome. Semin Perinatol 29:58-65, 2005 28. Lott IT, McPherson D, Towne B, et al: Long-term neurophysiologic outcome after neonatal extracorporeal membrane oxygenation. J Pediatr 116:343-349, 1990 29. Lohrer RM, Bejar RF, Simko AJ, et al: Internal carotid artery blood flow velocities before, during, and after extracorporeal membrane oxygenation. Am J Dis Child 146:201-207, 1992 30. Lewin JS, Masaryk RJ, Modic MT, et al: Extracorporeal membrane oxygenation in infants: angiographic and parenchymal evaluation of the brain with MR imaging. Radiology 173:361-365, 1989 31. Perlman JM, Altman DI: Symmetric cerebral blood flow in newborns who have undergone successful extracorporeal membrane oxygenation. Pediatrics 89:235-239, 1992 32. Streletz LJ, Bej MD, Graziani LJ, et al: Utility of serial EEGs in neonates during extracorporeal membrane oxygenation. Pediatr Neurol 8:190196, 1992 33. Taylor GA, Short BL, Fitz CR: Imaging of cerebrovascular injury in infants treated with extracorporeal membrane oxygenation. J Pediatr 114:635-639, 1989 34. Bulas DI, Taylor GA, Fitz CR, et al: Posterior fossa intracranial hemorrhage in infants treated with extracorporeal membrane oxygenation: sonographic findings. Am J Radiol 156:571-575, 1991 35. Brunberg JA, Kewitz G, Schumacher RE: Venovenous extracorporeal membrane oxygenation: early CR alterations following use in management of severe respiratory failure in neonates. AJNR 14:595-603, 1993 36. Taylor GA, Catena LM, Garin DB, et al: Intracranial flow patterns B.L. Short 50 37. 38. 39. 40. 41. 42. in infants undergoing extracorporeal membrane oxygenation: preliminary observations with Doppler US. Radiology 165:671-674, 1987 Taylor GA, Martin GR, Short BL: Cardiac determinants of cerebral blood flow during extracorporeal membrane oxygenation. Invest Radiol 24:511-516, 1989 Holley DG, Short BL, Karr SS, et al: Mechanisms of change in cardiac performance in infants undergoing extracorporeal membrane oxygenation. Crit Care Med 22:1865-1870, 1994 Short BL, Walker LK, Gleason CA, et al: Effect of extracorporeal membrane oxygenation on cerebral blood flow and cerebral oxygen metabolism in newborn sheep. Pediatr Res 28:50-53, 1990 Rosenberg AA, Kinsella JP: Effect of extracorporeal membrane oxygenation on cerebral hemodynamics in newborn lambs. Crit Care Med 20:1575-1581, 1992 Walker LK, Short BL, Gleason CA, et al: Cerebrovascular response to carbon dioxide in lambs receiving extracorporeal membrane oxygenation. Crit Care Med 22:291-298, 1994 Short BL, Walker LK, Bender KS, et al: Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr Res 33:289-294, 1993 43. Walker LK, Short BL, Traystman RJ: Impairment of cerebral autoregulation during venovenous extracorporeal membrane oxygenation in the newborn lamb. Crit Care Med 24:2001-2006, 1996 44. Ingyinn M, Lee J, Short BL, et al: Venoarterial extracorporeal membrane oxygenation (VA ECMO) impairs basal nitric oxide production in cerebral arteries of newborn lambs. Pediatr Crit Care Med 1:161-165, 2000 45. Ingyinn M, Evangelista R, Rais-Bahrami L, et al: Pulsatile ECMO maintains cerebral arterial endothelial function compared to non-pulsatile ECMO in newborn lambs. Pediatr Res 51:48, 2002 46. Wagerle LC, Russo P, Dahdah NS, et al: Endothelial dysfunction in cerebral microcirculation during hypothermic cardiopulmonary bypass in newborn lambs. J Thorac Cardiovas Surg 115:1047-1054, 1998 47. Martinez-Orgado J, Gonzalez R, Rodriguez-Martinez MA, et al: Endothelial factors and autoregulation during pressure changes in isolated newborn piglet cerebral arteries. Pediatr Res 44:161-167, 1998 48. Peckel MP, Leftheriotis G, Ferber C, et al: Effect of nitric oxide blockade on the lower limit of the cortical cerebral autoregulation in pentobarbital-anesthetized rats. Int J Microcirc Clin Esp 16:277283, 1996