Fetal Reduction Mark I. Evans, MD, and David W. Britt, PhD
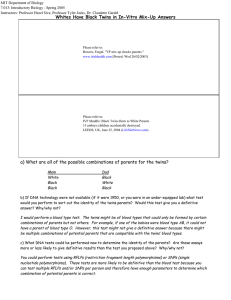
advertisement

Fetal Reduction Mark I. Evans, MD, and David W. Britt, PhD Fetal Reduction has been employed over the past two decades as a mechanism to reduce the morbidity and mortality of multiple pregnancies. Utilization of the procedure has increased dramatically as IVF has become commonplace but the average starting number has decreased with the transfer of fewer embryos. Success rates from fetal reduction have improved as a function of increasing experience, better ultrasound, and lower starting numbers. Genetic diagnosis prior to reduction can improve the overall outcomes. Reduction of triplets or more clearly improves outcomes, and reduction of twins to a singleton is now a reasonable consideration. Semin Perinatol 29:321-329 © 2005 Elsevier Inc. All rights reserved. I t will soon be 30 years since the birth of Louise Brown, the first baby to come from in vitro fertilization (IVF). Since that event, millions of babies have been born secondary to infertility therapies, including more than 1,000,000 IVF babies. These incredible success stories, however, have had corresponding serious side effects. The twin pregnancy rate, commonly quoted for decades to be 1 in 90, has more than doubled in the United States to more than 1 in 45. About 70% of all twins in the United States have come from infertility treatments. Some IVF programs create as many multiples as singletons. All multiple pregnancies have continued to rise, and the incidence of prematurity and related sequelae clearly correlate with fetal number (Fig. 1; Tables 1 and 2).1 With increasing public, professional, and legal attention, some of the very high-order multiples have diminished, particularly secondary to lower transfer numbers of embryos in IVF. There are some suggestions that the incidence of triplets and higher is slowly diminishing, but the incidence is still very high. In this arena, as with many others, it is often easier to appreciate the numerator than the denominator. Published pregnancy losses in multiple pregnancies are mostly a function of how early in pregnancy one establishes the actual number of cases.2,3 Some reports by perinatologists are overly, and we believe inappropriately, optimistic because these physicians don’t start “counting” until they begin to see patients in the second trimester, at which time most losses have already occurred.3,4 Many other articles have addressed those issues and will not be repeated here.4-6 Twenty years ago, about 75% of multifetal pregnancy pa- tients seeking reduction had pregnancies initiated with ovulation induction agents such as Pergonal.7 However, even with the first month of the lowest dose of Clomid, we have seen quintuplets. Over the years, the proportion of multiples induced by assisted reproductive technology (ART), such as IVF, have increased steadily, and currently about 70% of the patients we see seeking reduction have pregnancies generated by ART.8 Despite the increased utilization of ART, the proportion of hyperstimulated cases that result in quintuplets or more has dramatically decreased to less than 10% of all the cases we see. Regardless, the 2002 report of the Society of Assisted Reproductive Technologies (SART) published in December 2004 suggested that, of all pregnancies achieved following ART in the United States, 50.9% are singletons, 37.8% twins, 6.9% triplets or higher, and 4.4% were unknown.8-10 By birth, the percentages were 57.6% singletons, 39.6% twins, and 2.8% triplets or higher, reflecting the increased pregnancy loss rate of higher order multiples.10 In our experience with referred cases of ovulation stimulation, particularly those using FSH analogues, the proportion of cases that are quintuplets or more has fallen but not as dramatically.11 Such data continue to reinforce the significant role of vigilance in monitoring infertility therapies. It is our impression that the vast majority of multifetal cases occur to physicians with the best of equipment and the best of intentions who have an unfortunate and reasonably unpredictable or unpreventable maloccurrence. Despite this, clearly some cases might have been prevented if increased vigilance had been used.11-13 Demographics Fetal Medicine Foundation of America. Address reprint requests to Mark I. Evans, MD, Comprehensive Genetics, 131 E. 65th St., New York, NY 10021. E-mail: EVANS@COMPREGEN.COM 0146-0005/05/$-see front matter © 2005 Elsevier Inc. All rights reserved. doi:10.1053/j.semperi.2005.10.004 Over the past decade, the pattern of patients seeking multifetal pregnancy reduction (MFPR) has changed consider321 M.I. Evans and D.W. Britt 322 Figure 1 Risks of prematurity as a function of fetal number (2002 United States Centers for Disease Control Data). Diagonal lines: preterm birth ⬍32 weeks. Shaded area: birth weight ⬍1500 g. ably.11,12 With the rapid expansion of availability of donor eggs, the number of “older women” seeking MFPR has increased dramatically. In our experience, over 10% of all patients we see seeking MFPR are over 40 years of age, and nearly half of them are using donor eggs. As a consequence of the shift to older patients, many of whom already had previous children, there is an increased desire by these patients to have only one further child. The number of experienced centers willing to do 2 to 1 reductions is still very limited, but we believe it can be justified in the appropriate circumstances.11,13 For patients who are “older,” particularly those using their own eggs, genetic counseling and diagnosis becomes an important part of the process. By 2001, more than 50% of patients in the United States having ART cycles were over 35 (Table 3).1,9,10,14 In the1980s and early 1990s, the most common approach was to offer amniocentesis at 16 to 17 weeks on the remaining twins. However, a 1995 paper suggested an Table 1 Multiple Births in the United States Year Twins Triplets Quadruplets Quintuplets & Higher Multiples 2002 2001 2000 1999 1998 1997 1996 1995 1994 1993 1992 1991 1990 1989 % Change from 1989-2002 125,134 121,246 118,916 114,307 110,670 104,137 100,750 96,736 97,064 96,445 95,372 94,779 93,865 90,118 38.9% 6898 6885 6742 6742 6,919 6,148 5,298 4,551 4,233 3,834 3,547 3,121 2,830 2,529 172.8% 434 501 506 512 627 510 560 365 315 277 310 203 185 229 89.6% 69 85 77 67 79 79 81 57 46 57 26 22 13 40 72.5% Data taken from National Vital Statitics Report, Volume 52, #10, p22, 2003. Fetal reduction 323 Table 2 Ratio of Observed to Expected Multiples Births Observed Twins Triplets Quadruplets Quintuplets & higher multiples 125,134 6,898 434 69 Expected 44,686 496 6 0.07 Ratio 2.80:1 13.9:1 72.3:1 985.7:1 Total Births in 2002 - 4,021,726 11% loss rate in these cases, which caused considerable concern.15 Fortunately, the issue was settled by a much larger collaborative series in 1998 that showed that loss rates were no higher than comparable controls of MFPR patients who did not have amniocentesis.16 The collaborative data show a loss rate of 5%, which was certainly no higher than the group of patients post MFPR who did not have genetic studies. Since the centers with the most MFPR experience were also the ones who had the same accomplishments with chorionic villus sampling (CVS), combinations of the procedures were very logical. There are two competing possibilities as to the best approach to first trimester genetic diagnosis, ie, should it be before or after the performance of MFPR? Published data in the early 1990s suggested that performing the CVS first followed by MFPR resulted in a 1% to 2% error rate as to which fetus was which, particularly if the entire karyotype was obtained.17 Therefore, for the first 10 to 15 years, the approach we used was to generally do the reduction first at approximately 10.5 weeks in patients reducing to twins or triplets, followed by CVS approximately 1 week later.11,14 However, in patients going to a singleton pregnancy, essentially putting “all of their eggs in one basket,” we believed the best approach was to know what was in the basket before reducing the other embryos.11,12 In these cases we usually performed CVS on all the fetuses or one more than the intended stopping number, and performed a fluorescent in situ hybridization (FISH) analysis with probes for chromosomes 13, 18, 21, X, and Y. Whereas about 30% of overall anomalies seen on karyotype would not be detectable by FISH with these probes,18,19 the absolute risk of a remaining undetected anomaly is very small. Given both a normal FISH and a normal ultrasound including nuchal translucency,20 the residual risk is only about 1/400 to 1/500. We believe that such a risk is lower than the increased risk from the 2-week wait necessary to get the full karyotype. We have now commonly extended this approach to all patients who are appropriate candidates for prenatal diagnosis regardless of the fetal number (Fig. 2) Over the past few years, more than 75% our patients have combined CVS and MFPR procedures. With data now suggesting increased risks of chromosomal and other anomalies in patients conceiving by IVF and especially with intracytoplasmic sperm injection (ICSI), the utilization of prenatal diagnosis will likely increase even further.21-26 Clinical Uses MFPR is a clinical procedure developed in the 1980s where a small number of clinicians in both the United States and Europe attempted to reduce the usual and high adverse sequelae of multifetal pregnancies by selectively terminating or reducing the number of fetuses to a more manageable number. The first European reports by Dumez27 and the first American report by Evans and coworkers,28 followed by a further report by Berkowitz and coworkers,29 and later Wapner and coworkers,30 described a surgical approach to improve the outcome in such cases. Even these early reports appreciated the ethical dilemma faced by couples and physicians under such difficult circumstances.13 In the mid 1980s, needles were inserted transabdominally and maneuvered into the thorax for the injection of KCL or mechanical disruption of the fetus by either mechanical destruction, air embolization, or potassium chloride injections despite relatively mediocre ultrasound visualization. Transcervical aspirations were also initially tried, but with little success. Some centers also used transvaginal mechanical disruption, but data suggested a significantly higher loss rate than with the transabdominal route.31 Today virtually all experienced operators perform the procedure by inserting needles transabdominally under ultrasound guidance, although some unpublished data have suggested that some centers continue to use 6- to 8-week transvaginal reduction procedures despite considerably higher loss rates. Results Several centers with the world’s largest experience have collaborated to leverage their their data. In 1993 the first collaborative report showed a 16% pregnancy loss rate through 24 completed weeks.17 Such numbers represented a major improvement for higher order multiple pregnancies. Further collaborative papers have shown continued dramatic improvements in the overall outcomes of such pregnancies (Table 4).11 The 2001 collaborative data demonstrated that the outcome of triplets reduced to twins, and quadruplets reduced to twins, now perform essentially as if they started as twins.11 Even with the tremendous advances in neonatal care for premature babies, the 95% take home baby rate for those who start with triplets and the 92% take home baby rate for those who start with quadruplets clearly represent dramatic improvements over natural statistics. Not only has the pregnancy loss rate been substantially lowered, but so has the rate of very dangerous early prematurity. Both continue to be correlated with the starting number. Data from the past few years show that the improvements are, not surprisingly, greatest from the higher starting numbers (Fig. 3). The lowest pregnancy loss rates are for those cases reduced Table 3 Maternal Age and ART (SART Data - 2001) All Cases Fresh Non Donor <35 35-37 38-40 41-42 42ⴙ 81,915 60,780 28,778 14,416 11,301 4,365 2,190 M.I. Evans and D.W. Britt 324 Figure 2 CVS in multple pregnancies. CVS catheter inserted transcervically into posterior placenta. Anterior placenta could be done easily by either the transcervical or transabdominal approach. Table 4 Multifetal Pregnancy Reduction - Losses by Years Losses (weeks) Deliveries (weeks) % % % % % % Total < 24 > 24 25-28 29-32 33-36 37ⴙ 1986-90 508 1991-94 724 1995-98 1356 From Evans et al.11 13.2 9.4 6.4 4.5 0.3 0.2 10.0 2.8 4.3 21.1 5.4 10.2 15.7 21.1 31.5 35.4 61.0 47.4 also suggested that adverse perinatal outcomes are more common in IVF patients, specifically in singletons.33 There is disagreement as to whether reduced triplets have better outcomes than those left alone. Yaron and coworkers34 compared triplets to reduced twins to those of unreduced triplets with two large cohorts of twins. The data show substantial improvement in patients reduced to twins as compared with those with triplets. The data from the most recent collaborative series suggest that pregnancy outcomes for cases starting at triplets or even quadruplets reduced to twins do as well as starting as twins. Antsaklis and coworkers showed a reduc- % Losses & Premature Delivery to twins with increasing losses for those reduced to singletons followed by reduction to triplets. However, the rate of early premature delivery has been, not surprisingly, highest with those left with triplets followed by twins and lowest with singletons. Mean gestational age at delivery was also lower for those left with more fetuses. Birth weights following MFPR decreased, with starting and finishing numbers reflecting increasing prematurity.32 Although data in the literature are conflicting, our experience suggests that triplets reduced to twins do much better in terms of loss and prematurity than do unreduced triplets. We believe that, if a patient’s primary goal is to maximize the chances of surviving children, that reduction of triplets to twins achieves the best live born results. More recent analyses suggest that, although mortality is lowest with twins, morbidity is lowest with remaining singletons. Recent data have MULTIFETAL PREGNANCY REDUCTION Losses and Very Prematures by Starting Number 20 18 16 15.4 14 12 10 8 6 3.8 4 2 0 Starting # 6+ < 24 wks 25-28 wks 11.4 9.6 7.3 6.2 4.9 4.5 3.5 5 4 3 0.0 2 Figure 3 Multifetal pregnancy reduction losses and very prematures by starting number. (Modified from Evans et al.11) Fetal reduction 325 Table 5 Reduced vs “Unreduced” Triplets Comparison MFPR Cases Deliveries (weeks) Years Losses <24 wks 1980s 90-94 95-98 98-02 6.7% 5.7% 4.5% 5.1% 98-02(3ⴚ>1) 8.0% 24-28 wk 29-32 33-36 6.1% 5.2% 3.2% 4.6% Mean GA 35.5 4.0% Mean GA 39.5 9.1% 9.9% 6.9% 10.8% 36.9% 39.2% 28.3% 41.8% PMR 10.0/1000) 4.0% PMR 0/1000 12.0% 37ⴙ 47.9% 45.2% 55.1% 37.6% 72.0% Non Reduced Triplets 98 99 99 02 (Leondires) (Angel) (Lipitz) (Francois) 9.9% 8.0% 25.0% 8.3% Mean Mean Mean Mean GA GA GA GA 33.3 32.3 33.5 31.0 PMR PMR PMR PMR 55/1000 29/1000 109/1000 57.6/1000 From Evans MI, Krivchenia EL, Kaufman M, et al: The optimal management of first trimester triplets. The Central Association of Obstetricians and Gynecologists. Annual Meeting, Las Vegas, Nevada, October 27-30, 2002. tion of losses from 15.41% to 4.76% for twins and diminishment of low birth weight fom 28% to 11%.35 These data therefore support some cautious aggressiveness in infertility treatments to achieve pregnancy in difficult clinical situations. However, when higher numbers occur, good outcomes clearly diminish. Luke and coworkers have suggested that, in twin pregnancies with assisted reproduction, fetal reduction increased the risks for birth at ⬍30 weeks, very low birth weight, and slowed midgestational growth.36 This analysis, however, ignores the starting conditions, ie, how did they do compared with keeping triplets or quadruplets? Kozinsky and coworkers showed that the perinatal outcomes of singleton and twin pregnancies following ART were comparable to spontaneously conceived, matched pregnancies.37 McDonald and coworkers have recently shown in a metaanalysis that twins from IVF, even when matched to spontaneously conceived twins, had a somewhat higher risk for preterm birth but no significant differences in perinatal deaths, congenital malformations, or low birth weight.38 A 2001 paper suggested that reduced triplets did worse than continuing ones.39 However, analysis of that series showed a loss rate following MFPR twice that seen in our collaborative series11 and poorer outcomes in every other category for remaining triplets Several other recent papers have likewise shown higher risks for “unreduced” triplets than for reduced cases.40-43 It is clear that one must use extreme caution in choosing comparison groups (Table 5). Blickstein has reported that triplets do worse than reduced twins in every perinatal category in his large database.44 An ever increasing situation involves the inclusion of a monozygotic pair of twins in a higher order multiple.45 Our experience suggests that, provided the “singleton” seems healthy, the best outcomes are achieved by reduction of the monochorionic twins. Obviously, if the singleton is not healthy, then keeping the twins is the next choice. Pregnancy loss is not the only deleterious outcome. Very early preterm delivery correlates with the starting number. However, it has not been well appreciated that about 20% of babies born at less than 750 g develop cerebral palsy.46 In Western Australia, Peterson and coworkers showed that the rate of cerebral palsy was 4.6 times higher for twins than singletons per live births, but 8.3 times higher when calculated per pregnancy.47 Pharoah and Cooke calculated cerebral palsy rates per 1000 first year survivor at 2.3 for singletons, 12.6 for twins, and 44.8 for triplets.48 In a small series in a report of a questionnaire, Dimitiriou and coworkers showed no differences between triplets and twins, but there is not enough power to reach such conclusions.49 In the 2001 collaborative report, the subset of patients who reduced from two to one (not for fetal anomalies), included 154 patients. These data suggested a loss rate comparable to three to two, but, in about one-third of the two to one cases, there was a medical indication for the procedure, eg, maternal cardiac disease, prior twin pregnancy with severe prematurity, or uterine abnormality.11 In recent years, however, the demographics are changing, and the vast majority of such cases are from women in their 40s, or even 50s, some who of whom are using donor eggs and who, more for social than medical reasons, only want a singleton pregnancy.50-52 New data suggest that twins reduced to a singleton do better than remaining as twins.13 Consistent with the above, more women are desiring to reduce to a singleton. In a recent series of triplets, we found the average age of outpatients reducing to twins to be 37 years and to a singleton, 41 years.50 Although the reduction in pregnancy loss risk for three to one is not as much as three to two (15% to 7% and 15% to 5%, respectively), the gestational age at delivery for the resulting singleton is higher, and the incidence of births ⬍1500 g is 10 times higher for twins than singletons.1 These data have made counseling of such patients far more complex than previously (Figs. 4 and 5). Not surprisingly, there are often differences between members of the couple as to the desirability of twins or singleton.52 There are also profound public health implications to these decisions, as 2000 United States 326 Figure 4 Risk reduction as a function of starting number. Numbers on left are risks of spontaneous loss without reduction. Numbers on right are after reduction. Data show that, of $10.2 billion spent per year on initial newborn care, 57% of the money is spent on the 9% of babies born at ⬍37 weeks.53 In 2003, more than $10 billion was spent on the 12.3% born preterm.54 Data are now also emerging that there are considerably higher neurologic and developmental disabilities in 6-year-olds who survive after being born at 26 weeks or less. The rates of severe, moderate, and mild disabilty were 22%, 24%, and 34%, respectively. Significant cerebral palsy was present in 12%.55 Hack et al. have now shown that, in babies born at less than 1000 g, the rate of cerebral palsy was 14% as opposed to 0% for controls. Asthma, poor vision, IQ ⬍85, and poor motor skills were all also substantially higher.56 As a result of the changing demographics of infertility and MFPR, we believe that reduction of twins to a singleton is likely to become more common over the next several years. M.I. Evans and D.W. Britt believe this is a frivolous procedure, but see it in terms of the principle of proportionality, ie, therapy to achieve the most good for the least harm.13,57-59 In this section, we review a few studies that have immediate implications for MFPR clinics and ART clinics by virtue of giving some insight into how patients frame the decisions they are making and structure their social environments so as to reduce the risk of hostility in reaction to these choices. How patients “hear” and internalize data and make decisions with respect to reduction have been fascinating to us over the years. Much of the literature on medical decision making has emphasized a rational choice model that puts hard data regarding relative risks center stage and treats emotions, feelings, and values as complications that should be considered only as a second-stage analysis.60,61 Even in the literature that talks about genuine alternative models of decision making (systematic versus heuristic, for example), a central assumption is that there are individual differences in style that can be identified through what people say.62,63 We have approached this problem from a different direction, arguing that where controversial, high-anxiety decisions are concerned, patients treat these decisions as an ongoing part of the social reality that they are creating to live in and raise a family.64 This reality-construction process is proactive, with couples aware of the potential consequences of sharing with others what they are going through. In a recent study of sharing strategies among MFPR patients, we discovered four sharing strategies that varied in how selectively their situation and choices were shared.65 Strategies for sharing ranged in terms of selectivity from a defended-relationship approach, in which only the partner and patient knew about the problems the patient was facing, and the decision to reduce through a qualified family and friends strategy, in which information is shared only with those who appear to be trustworthy in terms of their reactions. Two less selective strategies also emerged from our analysis. In the first, both sets of Societal Issues MFPR will always be controversial. We believe that the real debate over the next 5 to 10 years will not be whether or not MFPR should be performed with triplets or more. A serious debate will emerge over whether or not it will be appropriate to offer MFPR routinely for twins, even natural ones for whom the outcome has been considered “good enough.”50 Our data suggest that reduction of twins to a singleton actually improves the outcome of the remaining fetus.50 No consensus on appropriateness of routine two to one MFPR, however, is ever likely to emerge. We do, however, expect the proportion of patients reducing to a singleton to steadily increase over the next several years. Over the years, much has been written on the subject. Opinions on MFPR, in our experience, have never followed the classic “pro-choice/pro-life” dichotomy.2,7,11,14 Opinions will always vary substantially from outraged condemnation to complete acceptance. No short paragraph could do justice to the subject other than to state that most proponents do not Figure 5 Risks starting with triplets. Reduction of triplets to twins has lower loss rates but higher incidence of prematurity, low birth weight, and infant mortality than reducing to a singleton. Numbers on left are risks with triplets, in the middle risks with twins, and on the right, risks with a remaining singleton. (Color version of figure is available online.) Fetal reduction 327 Table 6 Frame Comparison Medical Frame Intensity of Commitment to having children Intensity of training in medicine, dentistry, hard sciences and the law Intensity of commitment to belief that life begins at conception Intensity of commitment to career Source of moral authority for resolution Fundamentalist Frame Lifestyle Frame High High High High Low Modest Modest High Modest High Relative survivability of fetuses Low Minimization of damage to moral beliefs though a “barely sufficient” reduction High Having a “normal” life in a culture that values both careers and family for women parents are privy to what the couple is going through, and finally, there is an extended, open network strategy of family, friends, and colleagues being in the loop. No sharing strategy is completely free of the risk of encountering hostility. Even so, the odds of encountering hostility are significantly greater with the more open, less selective strategies. MFPR and ART clinics will vary in terms of the cultural style they have for handling patient anxiety and stress, but these results suggest that some way should be found to sensitize couples to the fact that selectively sharing what they are going through is an effective technique for at least neutralizing some of the hostility that they are at risk of confronting from family, friends, and others. To the extent that anxiety and stress have implications for clinic success rates, such results regarding sharing strategies become doubly important. The realities people construct— composed of supportive people and institutions together with complexes of supportive values, norms, and attitudes—are what patients use to view the data.57-59 The decisions they make and how they justify those decisions may help resolve incompatible elements in the realities in which they find themselves enmeshed. It may often happen, for example, that parents who have gone through reduction to two or one live in families and/or work in communities where having engaged in reduction would be considered as something shameful. The less control they have over the selection of family, friends, and workplaces, given the prospect of such stigma, the more likely they are to simply present their pregnancies to these publics as if their pregnancies had always involved twins or a singleton. Where they have more control over the situation—as typically happens with friends versus family—they may be more likely to selectively share their experiences. The social realities in which people live, however, involve more than people: they also involve values, norms, and attitudes. The one thing all MFPR patients have in common is a very strong desire to have a family (Table 6). But there does not appear to be a single set of supportive institutions, people, and norms that is conducive to going through the pain, stress, and resource expenditure of IVF. Rather, there are three alternative resolutions. The first of these, a rational Medical Frame, looks superficially like what one would ex- pect from the rational analysis model. But the commitment to factual analysis comes from patients’ having selected themselves into the hard sciences, medicine, dentistry, engineering, or the law— disciplines in which an appreciation of and trust in “facts” form a fundamental part of their disciplinary identity. Such women will want to see the numbers regarding the relative risk associated with different reduction choices and will want to engage in a rigorous discussion of the data and their implications. And they will be likely to choose a final number for reduction that maximizes the chances of a “take-home” baby. The lens of scientific objectivity is not the only frame through which women who have gone through IVF to have a child will examine these data (Table 6). For those who have immersed themselves in a social reality that has a strong emphasis on norms against abortion and/or reduction—such that they themselves have such normative beliefs and are heavily involved in religious institutions which reinforce similar beliefs—a detached examination of the “facts” is simply not possible. These “facts” hold no special moral authority and need not be trusted in and of themselves. Their beliefs and those of the individuals and social institutions in which they have selected themselves have a moral authority as well. The balance that such women will likely seek is one that reduces their relative risk to acceptable limits. So, unless the consequences are dire, they will not reduce at all or choose to reduce only to three. We labeled such a resolution a Conceptionalist Frame. Finally, there are those for whom the demands of career and/or existing children constitute powerful elements in their constructed realities. For such women—and this includes many of the older patients we encountered—the essential balance that they seek is a more secular one, a Lifestyle Frame, one that emphasizes creating a family situation in which having a family can be balanced with working, though the commitment to working is less than the intense career commitment seen among Medical Frame patients. Such women will more than likely choose reduction to two or even one depending on the number of other children they have and the level of resources that the family has. Clinicians and their counseling staff need to be aware that, to women who have selected themselves into and/or been 328 trained to accept the legitimacy of rigorously determined statistics regarding relative risk (a Medical Frame), reduction choices can be straightforward; or at least they can appear to be relatively straightforward. This is usually not the case, however, for women who must forge a resolution among potentially incompatible elements, as for women who are struggling to reconcile the potentially oppositional elements of religious beliefs and involvement with risks associated with higher-level pregnancies (Conceptionalist Frame), or those who are struggling to reconcile the potentially conflicting identities of home and work (Lifestyle Frame). Clinics have different styles of dealing with the multisourced anxieties with which patients walk through the door. The results that we have presented suggest that there is no “one size fits all” way of counseling and supporting patients. We expect, however, that successful clinics will have developed ways of understanding better where patients are coming from and what types of information and support will help them the most. Summary Over the last two decades, MFPR has become a well-established and integral part of infertility therapy and the attempts to deal with sequelae of aggressive infertility management. In the mid 1980s, the risks and benefits of the procedure could only be estimated.10-14 We now have very clear and precise data on the risks and benefits as well as an understanding that the risks increase substantially with the starting and finishing number of fetuses in multifetal pregnancies. The collaborative loss rate numbers, ie, 4.5% for triplets, 8% for quadruplets, 11% for quintuplets, and 15% for sextuplets or more, seem reasonable ones to present to patients when the the procedure is performed by an experienced operator. Our own experience and anecdotal reports from other groups suggest that less experienced operators have worse outcomes. Pregnancy loss is not the only poor outcome. The other main issue with which to be concerned is very early preterm delivery and the profound consequences to such infants. Here again, there is an increasing rate of poor outcomes correlated with the starting number. The finishing numbers are also critical, with twins having the best viable pregnancy outcomes for cases starting with three or more. However, an emerging appreciation that singletons have prematurity rates less than twins is making the counseling far more complex. We continue to hope, however, that MFPR will become obsolete as better control of ovulation agents and assisted reproductive technologies make multifetal pregnancies uncommon. References 1. Martin JA, Hamilton BE, Ventura SJ, et al: Births: final data for 2001. National Vital Statistics Reports (vol 51 no 2). Hyattville, MD, National Center for Health Statistics, 2002 2. Evans MI, Rodeck CH, Stewart KS, et al: Multiple gestation: genetic issues, selective termination, and fetal reduction, in Gleisher N, Buttino L Jr, Elkayam U, et al (eds): Principles and Practices of Medical Therapy in Pregnancy (ed 3). Norwalk, CT, Appleton and Lange Publishing, 1998, pp 235-242 M.I. Evans and D.W. Britt 3. Evans MI, Ayoub MA, Shalhoub AG, et al: Spontaneous abortions in couples declining multifetal pregnancy reduction. Fetal Diagn Ther 17:343-346, 2002 4. Keith LG, Blickstein I (eds): Triplet Pregnancies. London, Parthenon Press, 2002 5. Luke B, Brown MB, Nugent C, et al: Risks factors for adverse outcomes in spontaneous versus assisted conception twin pregnancies. Fertil Steril 81:315-319, 2004 6. Anwar HN, Ihab MU, Johnny BR, et al: Pregnancy outcomes in spontaneous twins versus twins who were conceived through in vitro fertilization. Am J Obstet Gynecol 189:513-518, 2003 7. Evans MI, Dommergues M, Wapner RJ, et al: Efficacy of transabdominal multifetal pregnancy reduction: collaborative experience among the world’s largest centers. Obstet Gynecol 82:61-67, 1993 8. Toner JP: Progress we can be proud of: U.S. trends in assisted reproduction over the first 20 years. Fertil Steril 78:943-950, 2002 9. Wright VC, Schieve LA, Reynolds MA, et al: Assisted reproductive technology surveillance: United States, 2001. MMWR Surveill Summ 53:1-20, 2004 10. 2002 Assisted Reproductive Technology Success Rates. National Summary and Fertility Clinic Reports. Centers for Disease Control. December 2004. US Govt Printing Office 11. Evans MI, Berkowitz R, Wapner R, et al: Multifetal pregnancy reduction (MFPR): improved outcomes with increased experience. Am J Obstet Gynecol 184:97-103, 2001 12. Adashi EY, Barri PN, Berkowitz R, et al: Infertility therapy-assisted multiple pregnancies (births): an on-going epidemic. Reprod Med 7:515-542, 2003 13. Evans MI, Fletcher JC: Multifetal pregnancy reduction, in Reece EA, Hobbins JC, Mahoney MJ, Petrie R (eds): Medicine of the Fetus and Its Mother. Philadelphia, PA, Lippincott Harper Publishing, 1992, pp 1345-1362 14. Evans MI, Littman L, St Louis L, et al: Evolving patterns of iatrogenic multifetal pregnancy generation: implications for aggressiveness of infertility treatments. Am J Obstet Gynecol 172:1750-1753, 1995 15. Tabsh KM, Theroux NL: Genetic amniocentesis following multifetal pregnancy reduction twins: assessing the risk. Prenat Diagn 15:221223, 1995 16. McLean LK, Evans MI, Carpenter RJ, et al: Genetic amniocentesis (AMN) following multifetal pregnancy reduction (MFPR) does not increase the risk of pregnancy loss. Prenat Diagn 18:186-188, 1998 17. Brambati B, Tului L, Baldi M, et al: Genetic analysis prior to selective termination in multiple pregnancy: technical aspects and clinical outcome. Hum Reprod 10:818-825, 1995 18. Evans MI, Henry GP, Miller WA, et al: International, collaborative assessment of 146,000 prenatal karyotypes: expected limitations if only chromosome-specific probes and fluorescent in situ hybridization were used. Hum Reprod 14:1213-1216, 1999 19. Homer J, Bhatt S, Huang B, et al: Residual risk for cytogenetic abnormalities after prenatal diagnosis by interphase fluorescence in situ hybridizatio (FISH). Prenat Diagn 23:556-571, 2003 20. Greene RA, Wapner J, Evans MI: Amniocentesis and choironic villu sampling in triplet pregnancy, in Keith LG, Blickstein I, Oleszcuk JJ (eds): Triplet Pregnancy. London, Parthenon Publishing Group, 2005, pp 73-84 21. Zadori J, Kozinszky Z, Orvos H, et al: The incidence of major birth defects following in vitro fertilization. J Assist Reprod Genet 20:131132, 2003 22. Pinborg A, Loft A, Schmidt L, et al: Morbidity in a Danish national cohort of 472 IVF/ICSI twins, 1132 non-IVF/ICSI twins and 634 IVF/ ICSI singletons: health-related and social implications for the children and their families. Hum Reprod 18:1234-1243, 2003 23. Place I, Englert Y: A prospective longitudinal study of the physical, psychomotor, and intellectual development of singleton children up to 5 years who were conceived by intracytoplasmic sperm injection compared with children conceived spontaneously and by in vitro fertilization. Fertil Steril 80:1388-1397, 2003 24. Retzloff MG, Hornstein MD: Is intracytoplasmic sperm injection safe? Fertil Steril 80:851-859, 2003 Fetal reduction 25. Kurinczuk JJ: Safety issues in assisted reproduction technology. From theory to reality: just what are the data telling us about ICSI offspring health and future fertility and should we be concerned? Hum Reprod 18:925-931, 2003 26. Tournaye H: ICSI: a technique too far? Int J Androl 26:63-69, 2003 27. Dumez Y, Oury JF: Method for first trimester selective abortion in multiple pregnancy. Contrib Gynecol Obstet 15:50, 1986 28. Evans MI, Fletcher JC, Zador IE, et al: Selective first trimester termination in octuplet and quadruplet pregnancies: clinical and ethical issues. Obstet Gynecol 71:289-296, 1988 29. Berkowitz RL, Lynch L, Chitkara U, et al: Selective reduction of multiple pregnancies in the first trimester. N Engl J Med. 318:1043, 1988 30. Wapner RJ, Davis GH, Johnson A: Selective reduction of multifetal pregnancies. Lancet 335:90-93, 1990 31. Timor-Tritsch IE, Peisner DB, Monteagudo A, et al: Multifetal pregnancy reduction by transvaginal puncture: evaluation of the technique used in 134 cases. Am J Obstet Gynecol 168:799-804, 1993 32. Torok O, Lapinski R, Salafia CM, et al: Multifetal pregnancy reduction is not associated with an increased risk of intrauterine growth restriction, except for very high order multiples. Am J Obstet Gynecol 179: 221-225, 1998 33. Jackson RA, Gibson KA, Wu YU, et al: Perinatal outcomes in singletons following in vitro fertilization: a meta analysis. Obstet Gynecol 103: 551-563, 2004 34. Yaron Y, Bryant-Greenwood PK, Dave N, et al: Multifetal pregnancy reduction (MFPR) of triplets to twins: comparison with non-reduced triplets and twins. Am J Obstet Gynecol 180:1268-1271, 1999 35. Antsaklis A, Souka AP, Daskalakis G, et al: Embryo reduction versus expectant management in triplet pregnancies. J Matern Fetal Neonatal Med 16:219-222, 2004 36. Luke B, Brown MD, Nugent C, et al: Risk factors for adverse outcomes in spontaneous versus assisted conception in twin pregnancies. Fertil Steril 81:315-319, 2004 37. Kozinsky Z, Zadori J, Ovros H, et al: Obstetric and neonatal risk of pregnancies after assisted reproductive technology: a matched control study. Acta Obstet Gynecol Scand 82:850-856, 2003 38. McDonald S, Murphy K, Beyene J, et al: Perinatal outcomes of in vitro fertilization twins: a systematic review and meta analysis. Am J Obstet Gynecol 193:141-152, 2005 39. Leondires MP, Ernst SD, Miller BT, et al: Triplets: outcomes of expectant management versus multifetal reduction for 127 pregnancies. Am J Obstet Gynecol 72:257-260, 1999 40. Lipitz S, Shulman A, Achiron R, et al: A comparative study of multifetal pregnancy reduction from triplets to twins in the first versus early second trimesters after detailed fetal screening. Ultrasound Obstet Gynecol 18:35-38, 2001 41. Angel JL, Kalter CS, Morales WJ, et al: Aggressive prerinatal care for high-order multiple gestations: does good perinatal outcome justify aggressive assisted reproductive techniques? Am J Obstet Gynecol 181: 253-259, 1999 42. Sepulveda W, Munoz H, Alcalde JL: Conjoined twins in a triplet pregnancy: early prenatal diagnosis with three-dimensional ultrasound and review of the literature. Ultrasound Obstet Gynecol 22:199-204, 2003 43. Francois K, Sears C, Wilson R, et al: Twelve year experience of triplet pregnancies at a single institution. Am J Obstet Gynecol 185:S112, 2001 44. Blickstein I: How and why are triplets disadvantaged compared to twins. Best Pract Res Clin Obstet Gynecol 18:631-644, 2004 45. Yakin K, Kahraman S, Comert S: Three blastocyst stage embryo transfer resulting in a quintuplet pregnancy. Hum Reprod 16:782-784, 2001 329 46. Task Force of American College of Obstetricians and Gynecologists. Neonatal encephalopathy and cerebral palsy: defining the pathogensis and pathophysiology. Washington DC, ACOG, 2003 47. Petterson B, Nelson K, Watson L, et al: Twins, triplets, and cerebral palsy in births in Western Australia in the 1980s. Br Med J 307:12391243, 1993 48. Pharoah PO, Cooke T: Cerebral palsy and multiple births. Arch Dis Child Fetal Neonatal Ed 75:F174-F177, 1996 49. Dimitiiou G, Pharoah PO, Nicolaides KH, et el: Cerebral Palsy in triplet pregnancies with and without iatrogenic reduction. Eur J Pediatr 163: 449-451, 2004 50. Evans MI, Kaufman MI, Urban AJ, et al: Fetal reduction from twins to a singleton: a reasonable consideration. Obstet Gynecol 104:102-109, 2004 51. Templeton A: The multiple gestation epidemic: the role of the assisted reproductive technologies. Am J Obstet Gynecol 190:894-898, 2004 52. Kalra SK, Milad MP, Klock SC, et al: Infertility patients and their partners: differences in the desire for twin gestations. Obstet Gynecol 102: 152-155, 2003 53. St. John EB, Nelson KG, Oliver SP, et al: Cost of Neonatal care according to gestational age at birth and survival status. Am J Obstet Gynecol 182:170-175, 2000 54. Cuevas KD, Silver DR, Brooten D, et al: The cost of prematurity: hospital charges at birth and frequency of rehospitalizations and acute care vistis over the first year of life: a comparision by gestational age and birth weight. Am J Nurs 105:56-64, 2005 55. Marlow N, Wolke D, Bracewell MA, et al: Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 352:9-19, 2005 56. Hack M, Taylor HG, Drotar D, et al: Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low birth weights in the 1990s. JAMA 294:318-325, 2005 57. Britt DW, Risinger ST, Mans M, et al: Devastation and relief: conflicting meanings in discovering fetal anomalies. Ultrasound Obstet Gynecol 20:1-5, 2002 58. Britt DW, Risinger ST, Mans M, et al: Anxiety among women who have undergone fertility therapy and who are considering MFPR: trends and scenarios. J Matern Fetal Neonatal Med 13: 271-278, 2003 59. Britt DW, Evans WJ, Mehta SS, et al: Framing the decision: determinants of how women considering MFPR as a pregnancy-management strategy frame their moral dilemma. Fetal Diagn Ther 19:232-240, 2004 60. Redelmeier DA, Rozin P, Kahneman D: Understanding patients’ decisions: cognitive and emotional perspectives. JAMA 270:72-76, 1993 61. Chapman GB, Elstein AS: Cognitive processes and biases in medical decision making, in Chapman GB, Sonnenberg FA (eds): Decision Making in Health Care: Theory, Psychology and Applications. New York, NY, Cambridge University Press, 2000, pp 183-210 62. Steginga SK, Occhipinti S: The application of the heuristic-systematic processing model to treatment decision making about prostate cancer. Med Decis Making 24:573-583, 2004 63. Hamm RM: Theory about heuristic strategies based on verbal protocol analysis: the emperor needs a shave. Med Decis Making 24:681-686, 2004 64. Britt DW, Campbell EQ: Assessing the linkage of norms, environments and deviance. Social Forces 56:532-549, 1977 65. Britt DW, Evans MI: Sharing and risk of negative reactions: preliminary examination of four alternative strategies used by patients facing a fetal reduction. Fertility and Sterility 84:523 (Suppl 1)