Digestive System B
advertisement

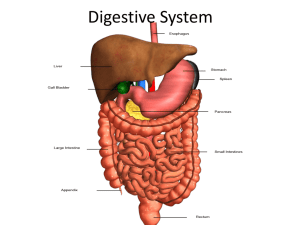
Digestive System B Tunics of the Abdominal GI Tract Figure 26.9 Mucosa There are three components to this deepest layer: • superficial epithelium • an underlying areolar connective tissue, called the lamina propria • a thin layer of smooth muscle, called the muscularis mucosae Submucosa Components include: • • • • lymphatic ducts mucin-secreting glands blood vessels Nerves The nerves and their associated ganglia are referred to as the submucosal nerve plexus (Meissner plexus) Muscularis • Two layers of smooth muscle: • • • Two exceptions: • • • inner circular layer—constricts the lumen and forms sphincters outer longitudinal layer—shorten the tube esophagus has a mix of both smooth and skeletal muscle stomach contains three layers of smooth muscle Nerve fibers and associated ganglia between the two layers of muscles is called the myenteric nerve plexus (Auerbach plexus) Tunics of the Abdominal GI Tract Figure 26.9 Adventitia or Serosa • Outermost layer • Areolar connective tissue with collagen and elastic fibers Blood Supply Three unpaired arteries supply the abdominal GI tract: • celiac trunk • superior mesenteric artery • inferior mesenteric artery Lymphatic Vessels and Structures • Lacteals are present in villi of the small intestines. • Lymph ducts transport lymph to the cisterna chyli, which drains into the thoracic duct. • Lymphatic structures called MALT (mucosa-associated lymphatic tissue) are found in the small intestine and appendix. These aggregate nodules are called Peyer patches. Nerves Both autonomic and sensory; the three autonomic plexuses follow the distribution of the unpaired artery of the same name: • celiac plexus • superior mesenteric plexus • inferior mesenteric plexus Esophagus • A tubular passageway that conducts ingested materials from the pharynx to the stomach. • Passes through an opening in the diaphragm called the esophageal hiatus as it connects to the stomach. • Approximately 25 cm long coursing anterior to the vertebral bodies • About 1.5 cm is in abdomen prior to changing into the stomach Esophagus Figure 26.1 Esophagus Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Mucosa Stratified squamous epithelium Muscularis mucosae Submucosa Muscularis Mucosa Lamina propria Adventitia LM 11x (a) Esophagus, transverse section Muscularis mucosae LM 65x (b) Esophageal mucosa a: © Alfred Pasieka/Peter Arnold; b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Figure 26.10 Esophageal Sphincters The esophagus has two sphincters: • Superior esophageal sphincter—at the junction of the pharynx and the esophagus; closes during inhalation preventing air from entering the GI tract • Inferior esophageal sphincter—at the junction of the esophagus and the stomach; along with the esophageal opening of the diaphragm, prevents materials from regurgitating from the stomach into the esophagus Phases of Swallowing There are three phases of swallowing: • voluntary phase • pharyngeal phase • esophageal phase Phases of Swallowing Figure 26.11 Stomach • Upper left quadrant of abdomen • It continues the mechanical and chemical digestion of the bolus • The bolus eventually is processed into a pastelike soup called chyme • Possesses three layers of muscle to aid in the mechanical processing of ingested materials Regions of the Stomach • The stomach is composed of four regions: • • • • • • cardia fundus body pyloris The inferior border of the stomach is the greater curvature and the superior border is the inferior curvature. The internal surface of the stomach is thrown into folds called gastric folds (rugae). Structure of Stomach Figure 26.12 Gastric Folds Structure of Stomach Figure 26.12 Wall of the Stomach • Lined by simple columnar epithelium although little absorption occurs in the stomach • Stomach lining is indented by numerous depressions called gastric pits Gastric Pits Figure 26.13 Gastric Secretions • Along and at the base of the gastric pits are the openings of gastric glands that secrete products into the stomach. Figure 26.13 Gastric Gland Five types of secretory cells form the gastric epithelium: 1. Surface mucous cells 2. Mucous neck cells 3. Parietal cells 4. Chief cells: PEPSIN 5. Enteroendocrine cells: GASTRIN Gastric Gland Figure 26.13 Small Intestine • Finishes the chemical digestion process and is responsible for absorbing most of the nutrients • Ingested materials spend at least 12 hours in the small intestine as chemical digestion and absorption are completed • About 6 meters (20 feet) long in an unembalmed cadaver but much shorter in a living individual due to muscle tone Small Intestine Consists of three specific segments (from proximal to distal from the stomach): • duodenum—25 cm (10 inches) • jejunum—2.5 m (7.5 feet) • ileum—3.6 m (10.8 feet) Small Intestine Figure 26.14 Duodenum • C-shaped • Upper right quadrant • Becomes continuous with jejunum at the duodenojejunal flexure (midline) • The major duodenal papilla is the site where bile and pancreatic secretions enter the duodenum Jejunum • Middle portion of the small intestine • Primary region for chemical digestion and nutrient absorption Ileum • Last segment of the small intestine • Distal end terminates at the ileocecal valve, a sphincter that controls the entry of materials into the large intestine Histology of the Small Intestine • Internally, the mucosal and submucosal tunics are thrown into folds called the circular folds (plicae circularis). • Microscopic fingerlike projections called villi can be seen on the surface of the circular folds. • Microscopic fingerlike projections called microvilli can be seen on the surface of the villi. Histology of the Small Intestine Figure 26.15 Histology of the Small Intestine Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Simple columnar epithelium with microvilli (absorbs nutrients) Circular folds Mucosa Submucosa Muscularis Inner circular layer Outer longitudinal layer Capillary network Goblet cells Lacteal Enteroendocrine cells (secrete hormones) Circular fold Serosa (a) Intestinal gland Lymphatic nodule Intestinal villi Muscularis mucosae Venule Lymph vessel Arteriole Submucosa (c) Intestinal villus Inner circular layer Muscularis Outer longitudinal layer Serosa (b) Section of small intestine Simple columnar cell Intestinal lumen Microvilli Villi Simple columnar epithelium Intestinal lumen Lamina propria TEM 18,000x (e) Microvilli Goblet cells LM 70x Figure 26.15 (d) Intestinal villi d: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser; e: © Dr. Lee Peachey Small Intestine Large Intestine • The large intestine forms a three-sided perimeter around the centrally located small intestine • Diameter is 6.5 cm vs. 2.5 cm of the small intestine, thus the name large intestine • Absorbs fluids and ions and compacts undigestible wastes and solidifies them into feces • Stores the feces until defecation (expulsion of the feces) Large Intestine The large intestine is comprised of the following structures: • cecum • ascending colon • transverse colon • descending colon • sigmoid colon • rectum • anal canal Large Intestine Figure 26.16 Cecum • • • First part of large intestine Blind sac located in lower right quadrant of abdomen Ileocecal valve represents junction between small intestine and large intestine Large Intestine Figure 26.16 Ascending Colon • Originates at the ileocecal valve and ascends right side of abdomen • As it approaches the inferior border of the liver, it makes a 90-degree turn toward the left side of the abdominal cavity; this bend in the colon is called the right colic flexure (hepatic flexure) Large Intestine Figure 26.16 Transverse Colon • Originates at the right colic flexure and approaches the spleen in the upper left abdominal quadrant • Suspended by the transverse mesocolon • It makes a 90-degree turn inferiorly at the spleen; this bend in the colon is called the left colic flexure (splenic flexure) Large Intestine Figure 26.16 Descending Colon • Originates at the left colic flexure • Found along the left side of the abdomen • Makes contact with iliac fossa and terminates into the sigmoid colon Large Intestine Figure 26.16 Sigmoid Colon • Its shape resembles the letter S • Turns inferomedially and is suspended by the sigmoid mesentery • Terminates as the rectum Large Intestine Figure 26.16 Rectum • Muscular tube that readily expands to store accumulated fecal material prior to defecation • Three thick, transverse folds of the rectum, called rectal valves, ensure that fecal material is retained during the passage of gas • The rectum terminates at the anal canal Large Intestine Figure 26.16 Anal Canal • Terminal few centimeters of the large intestine • Passes through an opening in the levator ani muscles of the pelvic floor • Anal columns line the internal surface of the anal canal • Anal sinuses secrete mucin for lubrication during defecation • Internal and external anal sphincters open and close the anal canal during defecation Anal Canal Figure 26.16 Histology of the Large Intestine • Lined with simple columnar epithelium and goblet cells, which secrete mucin to lubricate the fecal material Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Goblet cells Opening to intestinal gland Opening to intestinal gland Simple columnar epithelium Goblet cells Simple columnar epithelium Mucosa Intestinal gland Intestinal gland Lamina propria Submucosa Lymphatic nodule Muscularis mucosae Muscularis Muscularis mucosae Inner circular layer of muscularis Figure 26.17 Serosa (or adventitia) Nerves (a) Large intestine tunics Arteriole Venule Outer longitudinal layer of muscularis (tenia coli) LM 80x (b) Large intestine mucosa and submucosa b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Muscular Wall of Large Intestine • Longitudinal muscle is incomplete, forming bundles called teniae coli • They bunch up the large intestines into many sacs, collectively called haustra • Extending off the external surface of the haustra are lobules of fat called omental appendices or epiploic appendages Large Intestine Figure 26.16 Accessory Digestive Organs Includes the following organs: • liver • gall bladder • pancreas • biliary apparatus Liver • • Located in right quadrant of abdomen Comprised of four incompletely separated lobes: • • • • right lobe left lobe caudate lobe quadrate lobe Liver Figure 26.18 Liver Along the inferior surface of the liver, several structures collectively make the shape of the letter H: • inferior vena cava and ligamentum venosum form the inferior vertical parts • gall bladder and round ligament form the superior vertical parts • porta hepatis represents the horizontal crossbar; this is where the blood vessels (hepatic portal vein and hepatic artery proper) and lymphatic vessels, bile ducts, and nerves enter and leave the liver Liver Figure 26.18 Histology of the Liver Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Hepatic sinusoid Central vein Hepatocytes Bile canaliculi Hepatic lobule Reticuloendothelial cell Central vein Hepatic sinusoid Bile canaliculi Hepatocyte Portal triad Branch of bile duct (a) Hepatic lobules Branch of hepatic portal vein Branch of hepatic artery Portal triad Branch of bile duct Branch of hepatic portal vein Hepatic sinusoid Branch of hepatic artery Hepatocytes (b) Hepatocytes and sinusoids LM 220x (c) Portal triad Figure 26.19 c: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Gall Bladder • Embedded on the inferior surface of the liver • Functions to collect and concentrate bile • The cystic duct connects the gall bladder to the common bile duct Gall Bladder Figure 26.18 Pancreas • Has both endocrine (Chapter 20) and exocrine functions • Exocrine functions involve secreting digestive enzymes and bicarbonate, collectively called pancreatic juices, into the duodenum via the pancreatic duct into the duodenum Pancreas Figure 26.20 Biliary Apparatus • Network of thin ducts that transport bile from liver and gall bladder to duodenum • Function of the gall bladder is storage (not production) of bile Biliary Apparatus • Left and right lobes of the liver drain bile into the left and right hepatic ducts. • Left and right hepatic ducts merge to form the common hepatic duct. • The cystic duct and the common hepatic duct merge to form the common bile duct. • The common hepatic duct and the main pancreatic duct enter the duodenum through the hepatopancreatic ampulla. Bilia ry App arat us Figure 26.21 Development of the Digestive System Foregut Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Ventral mesentery Esophagus Dorsal mesentery Gallbladder (cystic bud) Liver Falciform ligament Liver buds Cystic bud Foregut Vitelline duct Ventral pancreatic bud Dorsal pancreatic bud Vitelline duct Midgut Lesser curvature of stomach Greater curvature of stomach Dorsal pancreatic bud Ventral pancreatic bud Primary intestinal loop Hindgut (a) Week 4: Liver, gallbladder, and pancreatic buds develop (b) Week 5: Greater and lesser curvatures of stomach form Direction of stomach rotation Gallbladder Falciform ligament Falciform ligament Esophagus Liver Liver Greater omentum Lesser omentum Gallbladder Direction of duodenum rotation Ventral pancreatic bud Direction of pancreas, bile duct rotation Figure 26.22 Stomach Common bile duct Pancreas Dorsal pancreatic bud (c) Weeks 6–7: Rotation of stomach, pancreatic buds Duodenum (d) Week 8: Postnatal position of organs attained Development of the Digestive System Midgut Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Ventral mesentery Liver Dorsal mesentery Vitelline duct Stomach Primary intestinal loop (midgut) Descending abdominal aorta Dorsal mesentery Cranial loop Caudal loop 90° counterclockwise Superior rotation mesenteric artery (b) Week 6: Herniation of loop; 90º counterclockwise rotation Caudal loop (forms much of large intestine) Direction of rotation 180º counterclockwise Vitelline duct Caudal loop Cranial loop Hindgut (a) Week 5: Primary intestinal loop forms Ventral mesentery Duodenum Transverse colon Colon Cranial loop (forms most of small intestine) Small intestine Ascending colon Descending colon (c) Weeks 10–11: Retraction of intestines back into abdominal cavity; 180º counterclockwise rotation Cecum Sigmoid colon Appendix Figure 26.23 (d) Postnatal position Rectum Primitive Gut Tube