Preoperative Hyperglycemia Increases Length of Stay after Major Orthopedic Surgery
advertisement

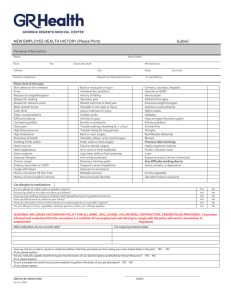
Preoperative Hyperglycemia Increases Length of Stay after Major Orthopedic Surgery Boris Mraovic, M.D., Jeffery I. Joseph, D.O., Brian R. Hipszer, M.S., Edward C. Pequignot, M.S., Inna Chervoneva. Ph.D. Department of Anesthesiology, Thomas Jefferson University, Philadelphia, PA Background: Methods: Results and Discussion: Reducing hospital length of stay (LOS) after major orthopedic surgery has gained popularity with surgeons, hospital administrators and third party payers. Admission hyperglycemia prolongs LOS in trauma parients. (1) Hyperglycemia has been reported to prolong LOS after ICU admission and CABG surgery.(2) However, it is unknown if increased blood glucose (BG) prolongs LOS after hip and knee surgery. After obtaining IRB approval, we retrospectively reviewed the medical records of patients undergoing elective total hip or total knee replacement from January 2001 to April 2006. Patients with incomplete records were excluded. Patients were divided into 3 groups based on preoperative BG levels: Normal <110 mg/dl, High 110-199 mg/dl and Very High ≥200 mg/dl. Data are reported as geometric mean with 95% confidence interval in parentheses unless otherwise noted. Effects of various risk factors on log transformed LOS were evaluated using robust regression and robust ANOVA. A p value of < 0.05 was considered statistically significant. Data from 7282 patients were included in the study. The median LOS was 3 days (range 1-58). Patients with Normal BG stayed on average 3.46 days (3.43, 3.49), High BG 3.62 days (3.56, 3.67) and Very High BG 4.05 days (3.80, 4.31). LOS was 8% (4, 12; p<0.001) longer in Very High group compared with Normal group. An 8% increase from the median LOS of 3 days translates into 5.8 hours. Age increased LOS by 2% (1, 2; p<0.001) per decade of life, BMI >40 kg/m2 by 4% (1, 6; p=0.002), duration of surgery >137 min by 19% (12, 20; p<0.001), bilateral knee surgery by 28% (27, 30; p<0.001) compared with unilateral knee surgery, knee surgery by 9% (8, 10; p<0.001) comparing with hip surgery. Patients with history of congestive hear failure had 6% (2, 10; p=0,004) longer LOS on average. Diabetes increased LOS by 4% (2, 5; p<0.001). Females had shorter LOS than males by 4% (3, 5; p<0.001) on average. Analysis confirms that the intention to decrease LOS was successful in our hospital. Compared to 2001, LOS was on average 9% (7, 11) shorter in 2002, 12% (10, 13) in 2003, 15% (14, 16) in 2004 and 16% (14, 17) in 2005/2006, p< 0.001. We investigate whether preoperative hyperglycemia ≥200 mg/dL (11.1 mmol/L) was associated with increased LOS after total hip and knee arthroplasty. Univariate analysis of length of stay after hip and knee surgery (n = 7282) Geometric means P values Percent increase of legth of stay (days) Female n=4090 (56.2%) 3.42 Male 3.31 n=3192 (43.8%) Age (yrs) (overall mean [SD]) 63.7 [12.2] <50 yrs 3.19 3.31 >60-70 yrs 3.39 >70-80 yrs 3.45 >80 yrs 3.56 Sex 0.96 (0.95, 0.97) <0.001* 30.1 [6. 2] Age per decade 1.01 (1.01, 1.01) <0.001* BMI 1.00 (1.00, 1.00) 0.311 ASA PS 2+4/1+2 1.01 (1.00, 1.02) 0.003* Hip/Knee 0.97 (0.93, 1.01) 0.126 Primary/Revisions 0.96 (0.94, 0.97) <0.001* Bilateral/Unilateral Knee 1.15 (1.14, 1.17) <0.001* OR Time (min) 1.00 (1.00, 1.00)) <0.001* Year of surgery 0.96 (0.96, 0.96) <0.001* High/Normal 1.00 (0.99, 1.01) 0.593 Very High/Normal 1.03 (1.00, 1.07) 0.031 * Arrhythmia 1.02 (1.00, 1.04) 0.024* CAD 1.01 (1.00, 1.02) 0.032* CHF 1.01 (0.98, 1.04) 0.537 Valve Disease 1.00 (0.98, 1.01) 0.683 Pulmonary 0.99 (0.98, 1.01) 0.316 Endocrinological 1.00 (0.99, 1.01) 0.665 Diabetes 0.96 (0.90, 1.02) 0.214 Hematological 1.01 (0.99, 1.02) 0.488 Sleep Apnea 1.01 (0.99, 1.03) 0.367 Stroke 1.00 (0.98, 1.02) 0.933 Hypertension 1.00 (0.99, 1.01) 0.741 Dislipidemia 1.00 (0.99, 1.01) 0.443 Malignancy 1.00 (0.98, 1.02) 0.930 BMI (kg/m ) (overall mean [SD]) <25 kg/m2 3.34 25-30 ≥ kg/m2 3.33 30-40 ≥ kg/m2 3.41 ≥ 40 kg/m2 3.49 ASA PS 1+2 3.33 2+4 3.43 30 Knee n=3203 (44.0%) 3.54 Hip n=4079 (56.0%) 3.25 Revisions n=811 (11.1%) 3.56 Primary 3.36 n=6471 (88.9%) Bilateral Knee n=735 (10.1%) Unilateral Knee n=2468 (33.9%) OR Time (min) mean [SD] 4.14 25 0.026 <0.001* <0.001* <0.001* 117 [44] 3.17 86-107 3.21 108-136 3.38 >137 3.81 Year of surgery <0.001* 2002 3.49 2003 3.37 2004 3.24 5 0 3.27 <0.001* Normal (<110) 3.34 High (111-199) 3.44 Very High (≥200) 3.79 Arrhythmia n=439 (6.0%) 3.53 0.112 CAD n=1091 (15.0%) 3.49 0.014* n=149 (2.1%) 3.91 0.004* n= 677 (9.3%) 3.39 0.229 Pulmonary n=1231 (16.9%) 3.43 0.249 Endocrinological n=918 (12.6%) 3.48 0.004* Diabetes n= 862 (11.8%) 3.52 <0.001* Hematological n=390 (5.4%) 3.45 0.081 Sleep Apnea n=392 (5.4%) 3.42 0.817 Stroke n=299 (4.1%) 3.50 0.217 Hypertension n=3874 (53.2%) 3.43 <0.001* Dislipidemia n=1370 (18.8%) 3.37 0.162 Malignancy n=491 (6.7%) 3.44 0.040 GI n=1944 (26.7%) 3.42 0.061 Liver disease n=01 (2.8%) 3.39 0.980 Rheumatoid Art n=210 (2.9%) 3.38 0.858 DVT n=258 (3.5%) 3.47 0.040* Renal n= 23 (0.32%) 3.56 0.757 UTI n=75 (1.03%) 3.37 0.531 Transfusions n=1357 (18.6%) 3.74 <0.001* * Statistically significant p<0.05 7 .7 3 .7 3 .5 3.78 Preoperative Glucose (mg/dL) Dx Preoperative Glucose 9 .3 5 .6 <0.001* 2005 15 10 Female/Male Surgery: 1 8 .9 20 Bilateral Knee P values (95% CI) 3.29 < 86 2001 Ratio of Geometric means 2 8 .2 <0.001* Surgery: CHF Multivariate analysis of length of stay after hip and knee <0.001* >50-60 yrs 2 Valve 35 <0.001 Percentage (%) Sex OR Time >137 min Knee Glucose ≥200 mg/dL CHF Diabetes BMI≥40 kg/m2 * Statistically significant p<0.05 Conclusion: References: Our data suggests that history of CHF is an independent risk factor for developing PE after major orthopedic surgery. Identifying patients with history of CHF could be helpful in the risk stratification for the thromboprophylaxis after total hip and knee surgery. 1. Sung J et al. Admission Hyperglycemia Is Predictive of Outcome in Critically Ill Trauma Patients. J Trauma. 2005;59:80-83. 2. Lazar HL and al. Tight Glycemic Control in Diabetic Coronary Artery Bypass Graft Patients Improves A prospective, randomized, controlled trial is required to determine whether optimizing CHF treatment prior to surgery would decrease the incidence of PE in this clinical setting. Perioperative Outcomes and Decreases Recurrent Ischemic Events. Disclosure: This research was conducted with support from the Investigator-Initiated Study Program of LifeScan, Inc.