MEDICAL LASERS: QUALITY CONTROL, SAFETY STANDARDS, AND REGULATIONS
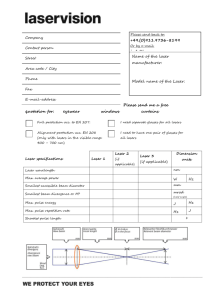
advertisement

AAPM REPORT NO. 73 MEDICAL LASERS: QUALITY CONTROL, SAFETY STANDARDS, AND REGULATIONS Joint Report Task Group No. 6 AAPM General Medical Physics Committee and American College of Medical Physics Suresh M. Brahmavar, Ph.D. Chairman, Medical Laser Task Group Fred Hetzel, Ph.D. Chairman, Photodynamic Therapy (PDT) Task Group October 2001 Published for the American Association of Physicists in Medicine and the American College of Medical Physics by Medical Physics Publishing DISCLAIMER: This publication is based on sources and information believed to be reliable, but the AAPM and the editors disclaim any warranty or liability based on or relating to the contents of this publication. The AAPM does not endorse any products, manufacturers, or suppliers. Nothing in this publication should be interpreted as implying such endorsement. International Standard Book Number: 1-888340-31-2 International Standard Serial Number: 0271-7344 Further copies of this report ($15 prepaid) may be obtained from: Medical Physics Publishing 4513 Vernon Blvd. Madison, WI 53705-4964 Telephone: 1-800-442-5778 or 608-262-4021 Fax: 608-265-2121 Email: mpp@medicalphysics.org Web site: www.medicalphysics.org 2001 by American Association of Physicists in Medicine, One Physics Ellipse, College Park, MD 20740-3846 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means (electronic, mechanical, photocopying, recording, or otherwise) without the prior written permission of the publisher. Published by Medical Physics Publishing 4513 Vernon Blvd., Madison, WI 53705-4964 Printed in the United States of America Task Group on Medical Lasers QC, Safety, Standards and Regulations Suresh M. Brahmavar, Ph.D. Chairman, Medical Lasers Baystate Health System Springfield, Massachusetts Fred Hetzel, Ph.D. Chairman, PDT Task Group Research & Development HealthOne Denver, Colorado Patrick Clark Director of Research & Development EpiCentre, Inc. Dallas, Texas Penny J. Smalley, R.N. Consultant 1444 W. Farwell Chicago, Illinois Cathy Miller, R.T.R. Assistant R.S.O. Baystate Health System Springfield, Massachusetts iii Robert Watkins, M.S. Senior Radiation Physicist Radiation Control Office Department of Public Health Boston, Massachusetts Leslie Pollard Medical Laser Safety Officer Minimal Invasive Surgical Team Director St. Joseph’s Hospital Asheville, North Carolina Vangie Paschall-Dennis Advanced Technologist Promina Gwinnet Health System Atlanta, Georgia Terry LaFrance, M.S. Senior Physicist Baystate Health System Springfield, Massachusetts iv Contents Preface .................................................................. vii Acknowledgments ................................................... viii I. Introduction .......................................................... 1 II. Need For A Laser Safety Program ............................. 3 III. Current Standards, Federal And State Regulations ............................................. Medical Laser Standards ............................................ Federal Regulations: FDA/CDRH/OSHA......................... State Regulations ..................................................... Non-Governmental Agencies: JCAHO........................... 7 7 8 9 9 Laser Bioeffects and Concepts Of Nominal Hazard Zone (NHZ), Maximum Permissible Exposure (MPE), Etc. ............................................... Classification of Lasers............................................... Common Lasers and Useful Definitions......................... Basic Biological Effects .............................................. Laser Tissue Interactions ............................................ Depth of Penetration ................................................ Nominal Hazard Zone (NHZ) ..................................... Maximum Permissible Exposure (MPE) ......................... Exposure Durations .................................................. 11 11 13 14 14 15 15 15 16 V. Operational Aspects of the Clinical Laser Program ...... Laser Committee ..................................................... Committee Membership ........................................... Committee Function ................................................ Basic Areas of Controls .............................................. 17 17 17 18 18 VI. Responsibility and Authority of the Laser Safety Officer (LSO) ................................................ Consultative Services ................................................ Regulations............................................................. Authority................................................................ Records ................................................................. Surveys and Inspections ............................................ Accidents ............................................................... Approval of Laser System Operation ............................ Other Related Responsibilities..................................... Deputy Laser Safety Officers....................................... 19 19 19 20 20 20 20 21 21 22 IV. v Contents VII. Quality Control and Radiation Safety ........................ A. Physical Inspection of Equipment and Accessories . B. Laser Safety................................................... C. Output Measurements and Quality Control ......... D. Education and Training ................................... E. Summary of Control Measures .......................... F. Clinical Laser Systems...................................... G. Equipment Testing/Clinical Use ......................... VIII. Laser Safety Procedures for Clinical Use IX. Useful Data and Tables ........................................... Table 1A NHZ Distances for Selected Surgical Lasers Without Delivery System Constraints ............. Table 1B Laser Criteria Used for NHZ Distance Calculations.............................................. Table 2 MPE Limits for Selected Surgical/ Medical Lasers........................................... Table 3 Control Measures for the HCLS..................... Table 4 Wavelength Effects for Various Lasers ............. Table 5 Laser Safety Training Program ...................... 35 X. Sample Forms ........................................................ Form #1 Laser Quality Assurance............................... Form #2 Quality Control of Medical Lasers .................. Form #3 Laser Log and Record ................................. Form #4 Laser Privilege Application Form.................... Form #5 Laser Operator Skills Validation ..................... Form #6AApplication for Registration of a Laser Facility... Form #6B Inventory of Class IIIB and IV Lasers ............... 41 41 42 43 44 46 47 48 XI. Operational Procedures .......................................... Procedure #1 Standards for Approval of Laser Use by Health Care Professionals ............................. Standards to Credential Physicians in Laser Therapy............................................. Standards to Credential Nurses in Laser Therapy... Credentials and Orientation for Laser Technicians . Procedure #2 Pre/Post-Operative Safety Checklist.......... Procedure #3 Practical “Rules of Thumb” for Laser Safety .............................................. Procedure #4 Non-Beam Hazards .............................. Procedure #5 Laser Safety Education Program .............. 49 XII. 23 24 25 27 28 28 28 28 .................... 31 35 35 36 37 38 39 49 50 52 53 54 55 58 60 Bibliography ......................................................... 63 vi Preface This document is historic for two major reasons. First, it represents the first jointly authorized publication by both American Association of Medical Physicists (AAPM) and American College of Medical Physics (ACMP). This document began as a 1991 ACMP report. In 1997 the General Medical Physics committee of AAPM invited Dr. Brahmavar, who authored the original report, to chair a task group to rewrite and update the document as an AAPM task group report. As it neared completion, there was a suggestion that perhaps ACMP would be interested in supporting the revised document. In the spring of 2000 it was independently approved by both organizations, each of which endorsed joint publication. This document is also historic because it addresses unique subject matter for the two Medical Physics organizations. One of the major objectives of the current AAPM General Medical Physics committee has been to bring medical physicists into the two organizations whose specialty or area of practice is not necessarily radiological physics (either diagnostic or therapeutic). This document on medical laser physics represents the first major, visible step in that direction. It also serves to establish AAPM and ACMP as the national organizations setting guidelines for this expanding area of Medical Physics. Fred W. Hetzel, Ph.D., J.D. Vice President HealthONE Alliance 1850 High Street Denver, CO 80218 vii Acknowledgments We would like to acknowledge with thanks the help, support, and special efforts of members of Task Group No. 6 on Medical Lasers, leadership of AAPM and ACMP, and Mary Kober of Baystate Medical Center, Springfield, MA, for excellent secretarial assistance given in preparing this final document for use by other medical physicists interested in safe use of medical lasers in patient care. We would also like to acknowledge the extensive use of resource materials from Rockwell Laser Industries, ANSI Standards and ACMP. Fred Hetzel, Ph.D. Chairman, AAPM PDT Task Group Suresh M. Brahmavar, Ph.D. Chairman, AAPM Medical Laser Task Group October 2000 viii I. Introduction The purpose of this document is to provide hospitals and the Joint Commission on Accreditation of Hospitals Organization (JCAHO) a guide prepared by medical physicists recommending tests and procedures for medical lasers to maintain a high level of quality care in a safe environment. The guidance for safe use of laser systems for diagnosis and therapy is intended for use by all health care personnel associated with laser systems’ operation (physicians, nurses, medical physicists), maintenance (engineers), and service (biomedical technicians). The suggested controls are based upon evaluation of potential hazards from laser radiation; unique problems related to operating rooms, outpatient clinics, and private medical offices; and exposure risks to patients and personnel. The control procedures are derived from ANSI Standards Z136.1 and Z136.3. Other resource materials are listed in the bibliography. A growing use of medical lasers is in the area of photodynamic therapy (PDT) where lasers provide a convenient source of intense, narrow bandwidth light. The safe use of the specialized lasers and fiber optics for PDT is to be addressed in a companion AAPM Task Group report and guidance document. Evaluation of medical laser safety and quality assurance (QA) should be performed under the direction of a qualified expert, in this case a medical physicist. Government agencies, independent advisory corporations, and professional societies have published definitions of a medical physicist and a qualified expert. A medical physicist is an individual with his/her principal education in physics with a minimum of a master’s degree plus 4 years of experience in medical physics or a Ph.D. degree with 3 years of experience in medical physics. A qualified expert in medical laser safety is an individual who has demonstrated to the satisfaction of the appropriate supervising or regulatory body that 1 Introduction he/she possesses sufficient knowledge, training, and experience to measure laser radiation, to evaluate safety techniques, and to advise regarding protection for laser radiation. Not all measurements have to be made by the medical physicist, but all measurements must be made under the immediate supervision of a qualified expert. The decision concerning which measurements are made by a physicist and which can be made by an engineer or a nurse under the supervision of the qualified expert must be made by the medical physicist who assumes sole responsibility for interpretation. 2 II. Need For A Laser Safety Program The term LASER is an acronym for Light Amplification by Stimulated Emission of Radiation. Lasers are special devices that produce light that is monochromatic, directional, and coherent. These special characteristics are utilized in designing laser devices that are used in industry and in medicine. Industry uses lasers to cut, weld, drill, mark, and fuse materials. Laser applications include the manufacture of integrated chips, precise alignment, and communications. Medical uses of lasers include surgery, dermatology, gynecology, cardiology, otology, ophthalmology, etc. Recent uses include angioplasty, photodynamic therapy (PDT), and diagnostic image processing. In the United States about 500,000 to 700,000 health care workers are involved in the use of medical lasers. The safety concerns in the use of medical lasers are related to operators, patients, and laser devices. The laser hazards are not limited only to the primary beam but also to nonbeam exposure of the environment. The total number of reported accidents for the period 1984 to 1996 is 339, and this number is growing every year. These data are displayed in diagrams 1 and 2. The major accident categories are: • Unanticipated eye exposure during alignment • Misaligned optics and upwardly directed beams • Available eye protection not used • Equipment malfunction • Improper methods of handling high voltage • Intentional exposure of unprotected personnel • Operators unfamiliar with laser equipment • Lack of protection for ancillary hazards • Improper storage of equipment following service • Failure to follow standard operating procedures (SOPs) • Accidental eye/skin exposure during use 3 Need For A Laser Safety Program Laser hazards involve exposure risks to the eye and skin, as well as fires, electrical system faults, and emission of fumes/toxic substances. Diagram 1. Laser Accident Summary: Incidents Reported (1964–1996) 4 Need For A Laser Safety Program Diagram 2. Laser Accident Summary: Breakdown of 330 Events by Type of Laser 5 Need For A Laser Safety Program 6 III. Current Standards, Federal And State Regulations Medical Laser Standards Medical Laser Standards include: • ANSI Z136.1 (2000): Safe Use of Lasers • ANSI Z136.3 (1996): Safe Use of Lasers in Health Care Facilities These standards provide guidance for the safe use of lasers for diagnostic and therapeutic applications in health care facilities. Lasers used in health care applications are incorporated into an apparatus that includes a delivery system to direct the output of the laser, a power supply with control and calibration functions, mechanical housing with interlocks, and associated fluids and gases required for the operation of the laser. This document pertains to the safe use of this entire apparatus, which is referred to as a Health Care Laser System (HCLS). The standard is intended for use by all persons associated with the installation, operation, maintenance, and service of HCLSs. These standards include engineering, procedural, and administrative controls necessary for the safety of patients and health care professionals. These controls are based upon: evaluation of potential hazards from laser radiation; unique problems related to operating rooms, outpatient clinics, mobile laser units, and private medical and dental offices; and exposure risks to patients and professional staff. Included in these standards are engineering and administrative controls, personnel protective equipment, and laser safety training. Suggestions for safe use of specific types of HCLSs and use of HCLSs in various subspecialties are included in the appendix of the ANSI standards. 7 Current Standards, Federal And State Regulations Federal Regulations: FDA/CDRH/OSHA The Federal Food and Drug Administration (FDA) Center for Devices and Radiological Health (CDRH) has the responsibility for implementing and enforcing the laws and regulations which apply to radiation-producing electronic products and medical devices. The details are contained in Code of Federal Regulations (CFR) Title 21, Parts 1040.10 and 1040.11, Medical Devices Act. Medical devices, including laser systems for medical applications, require clearance by the FDA in order to be introduced commercially in the United States. The clearance can follow the review of a premarket notification under section 510(k) of the Federal Food, Drug and Cosmetic Act (FFDCA) for a device that is substantially equivalent to a device that was in commercial distribution in the United States prior to May 1976 (enactment date of the Medical Device Amendments to the FFDCA), or to previously cleared devices. Clearance for other devices requires approval of an application for premarket approval. Clearances are device specific and for indications claimed in the cleared labeling. Clinical use of a device for indications that have not been cleared requires (additional) clearance or use of the device is considered “investigational.” The FFDCA does not prevent a physician from using a device in a manner that has not been approved. However, this investigational or off-label use generally requires approval of an investigational review board or ethics committee. Investigational use of a device for which approval for a new indication is desired by the manufacturer or distributor requires that there be: • An investigational protocol limited in scope and duration • Approval by an Investigational Review Board (IRB) 8 Current Standards, Federal And State Regulations • Approval by the FDA for investigations of devices of significant risk • Informed patient consent The Occupational Safety and Health Administration (OSHA) regulations for laser safety are contained in the documents related to Employee Safety and General Duty Clause. OSHA’s main interest is employee safety for personnel working in laser use areas. OSHA may arrive for inspection without notice or upon a complaint by an employee at the institution. The complaint may not be related to laser use. State Regulations Several states, including Arizona, Texas, Illinois, Georgia, Florida, Massachusetts, and Vermont, currently require registration of medical lasers. Arizona and Massachusetts have been most successful in formulating regulations for hospital laser use. The regulations cover use of class IIIB and IV medical lasers and require that the hospital: • Designate a Laser Safety Officer (LSO) with designated duties • Establish a laser use committee with duties and membership requirements • Report laser-related incidents or safety violations • Regularly inspect safety eyewear • Perform regular preventive maintenance • Conduct routine safety inspection of lasers • Follow pre-surgery and post-surgery checkups Non-Governmental Agencies: JCAHO To date, JCAHO has not provided a set of written criteria for laser use in a hospital setting. The JCAHO expectations are that hospital use of lasers is based on the ANSI standards. JCAHO’s interests lie in procedures, 9 Current Standards, Federal And State Regulations documentation, quality management, nursing care, and staff competency. In addition, the inspections include environmental aspects such as control zones, limited access, and personal protection devices. The Laser Safety Program must be integrated into the Hospital’s Safety Programs with a designated LSO, Laser Committee, etc. 10 IV. Laser Bioeffects And Concepts Of Nominal Hazard Zone (NHZ), Maximum Permissible Exposure (MPE), Etc. Classification of Lasers Lasers and products containing lasers must be classified according to the amount of radiation accessible during normal usage, not during periods of service or maintenance. The maximum output energy or power must be considered when determining the laser classification, even though normal operation may require less than maximum output. Laser classification relates to the potential for injury from the beam itself and not from related dangers such as electrical systems. A Class I rating for a laser can be obtained by assuring that an operator cannot have access to hazardous laser energy. This may be accomplished with very low power lasers that produce less than a hazardous amount of energy. In the visible spectrum region this amounts to less than 0.4 microwatts of power. A laser may also be considered to be Class I if a more powerful laser is contained within an enclosure. Operators cannot be allowed to open this enclosure when the laser beam is present. During periods of service or maintenance, however, the higher power laser beam may be accessible. Class II lasers must be visible. The output power of these lasers must be low enough so that a person’s natural aversion to bright light will protect the eye. These lasers must produce less than 1 mW of visible, continuous wave (CW) light. Provided a person does not force himself to look into the beam, these lasers are relatively safe. They will not produce skin burns but are theoretically able to produce eye injuries if viewed for more than 0.25 seconds. A special classification also exists called Class IIA. These lasers are not allowed to produce more than Class 11 Laser Bioeffects And Concepts of NHZ, MPE, etc. I limits for relatively short periods of time. A Class IIA laser must be designed so that intentional viewing of the beam is not anticipated. A scanning laser, such as found in supermarkets, designed to read “barcodes” is a typical example of a Class IIA laser. Class III lasers may be divided into two subgroups. Class IIIA lasers are allowed to exceed the power limit of Class II by no more than five times. Thus a continuous wave (CW) visible Class IIIA laser has a maximum power of 5 mW. Often, these lasers will have an expanded beam diameter so that no more than 1 mW can enter a fully dilated pupil, which is 7 millimeters (mm). There are slight variations between the concepts of IIIA classification as per CDRH or ANSI. For instance, the ANSI standard allows some invisible lasers to be rated IIIA but the CDRH standard only allows visible lasers in this class. Class IIIB lasers may be either visible or invisible, but they cannot produce more than 500 mW of CW power. Class IIIB lasers produce enough power to result in an injury before a person could react. Both the eye and the skin can be injured if exposed to the direct beam (including mirror reflections) from Class IIIB lasers. Scattered energy (diffuse reflections) is not considered hazardous in most situations—unless the laser is operating near the upper power limit of Class IIIB and a diffuse target is viewed at close distances. Class IV lasers present the greatest potential hazard. Both the eye and skin can easily be injured. Not only is the direct beam hazardous but diffuse reflections can also produce injuries. The greatest number of control measures must be applied to ensure safety of Class IV lasers, which are capable of producing more than 500 mW of power. The Class IV lasers produce fire hazards and ocular and skin hazards when exposure to both the direct beam and the scattered beam occurs. 12 Laser Bioeffects And Concepts of NHZ, MPE, etc. Common Lasers and Useful Definitions Common lasers operate in specific areas of the spectrum. There are several common lasers that produce light in the visible portion of the spectrum. The argon, HeNe, and ruby are among the most popular visible light lasers. Other laser types such as Nd:YAG and GaAS diode lasers operate at a near infrared portion of the spectrum. This region is invisible to the eye but is close enough to the visible spectrum to act like visible light when it travels through most standard optical elements. The CO2 laser generates a wavelength that is very long compared to visible light. This wavelength is in the far infrared spectral region. Waves of this length do not transmit through glass components like lenses or prisms. Optical elements for far infrared energy are made of exotic materials such as zinc selenide. The excimer laser is a unique type of laser. It may use several different gases, which allows it to generate many different wavelengths in the ultraviolet portion of the spectrum. The active medium is a collection of atoms, molecules or ions that absorb energy from an outside source and generate laser light by stimulated emission. The active medium can consist of a solid, a liquid, a gas or a semi-conductor material. It is the active material in which the laser light is produced. This material determines many of the laser beam’s output characteristics, including its wavelength. The excitation mechanism is the input energy device. In solid-state lasers, this mechanism is an intense light source. Gas lasers receive input energy from a flow of electrical current through the active gas. 13 Laser Bioeffects And Concepts of NHZ, MPE, etc. The high reflectance mirror and the output coupler compose the feedback mechanism. These mirrors are specially designed for the laser wavelength and consist of coatings of vapor deposited on the substrate to form the reflective surfaces. Basic Biological Effects Wavelength Band Eye Skin UV-C (0.200–0.280 microns) Photokeratitis Erythema (sunburn) Skin cancer UV-B (0.280–0.315 microns) Accelerated skin aging Increased pigmentation UV-A (0.315–0.400 microns) Photochemical Cataract Pigment darkening Photosensitive reactions Skin burn Visible (0.400–0.780 microns) Photochemical and thermal retinal injury Photosensitive reactions Skin burn IR-A (0.780–1.40 microns) Cataract retinal burn Skin burn IR-B (1.40–3.00 microns) Corneal burn, aqueous flare, possibly cataract Skin burn IR-C (3.00–1000 microns) Corneal burn only Skin burn Laser Tissue Interactions Thermal • Caused by elevated temperature after absorption of laser energy • Nearly all wavelengths and exposure durations Photochemical • Caused by chemical reactions within body tissue after absorption of laser energy • Only with wavelength less than 0.550 µm • Dominant effect for exposure durations greater than 10 sec 14 Laser Bioeffects And Concepts of NHZ, MPE, etc. Shockwave (Acoustic) • An explosive effect when short pulses are absorbed on the retina • Pulse duration less than 10 µsec Depth of Penetration Laser Type Depth (mm) CO2 0.1 Holmium YAG 1.3 Argon 0.8 Nd:YAG 4.2 Nominal Hazard Zone (NHZ) The nominal hazard zone (NHZ) is the space within which the irradiance or radiant exposure exceeds the appropriate Maximum Permissible Exposure (MPE). If a person is within an area where the laser irradiance exceeds the MPE, a potential hazard exists and the person must apply appropriate protective control measures. According to the ANSI Z136.1 standard, there may be four different scenarios in which exposure may occur. Each situation has a formula to use for determining the NHZ. Maximum Permissible Exposure (MPE) MPE is the acronym for Maximum Permissible Exposure. As defined by ANSI Z136.1, “Standard for the Safe Use of Lasers,” the MPE is: The level of laser radiation to which a person may be exposed without hazardous effect or adverse biological changes in the eye or skin. 15 Laser Bioeffects And Concepts of NHZ, MPE, etc. Actual MPE values vary according to the laser wavelength and the exposure duration. Different values can be determined for intrabeam laser exposure, extended source laser exposure or exposure to the skin. Exposure Durations 30,000 sec Occupational 8-hour work day 600 sec Visible wavelengths used for alignment purposes 0.25 sec Normal eye aversion response to bright visible light 10 sec For normal maximum exposure time, infrared wavelengths due to natural body movement 24 hr Accumulate “on” time for ultraviolet wavelengths over 24 hours The above exposure times are required by ANSI Z136.1, “Standard for the Safe Use of Lasers” when determining the MPE for a laser hazard evaluation. In some situations the exposure duration is determined by the laser parameters, but in other situations the “informed judgment” of the laser safety officer may be relied on to determine potential exposure durations. 16 V. Operational Aspects Of The Clinical Laser Program The decision to use medical lasers in a health care facility should be followed by a commitment by the management to establish a viable Laser Safety Program for the institution. The Laser Safety Program should address the needs of the Clinical Laser Program (CLP) for the specific use of medical lasers. The elements of a successful laser safety program are establishment of a laser committee, committee membership, committee functions, and basic areas of controls for safe use of medical lasers. Laser Committee • Function • Promote “safe” laser use • Administer policies and procedures • Oversee credentialing process • Assist in equipment evaluation • Monitor quality assurance activities Committee Membership • Physician from each laser specialty • Administration • Laser Nurses, each area • Anesthesiology • Biomedical Engineering • Laser Safety Officer (LSO)/Medical Physicist 17 Operational Aspects Of The Clinical Laser Program Committee Function • Policies and Procedures • Credentialing • Coordinating on Laser Activity • Appoint a Laser Safety Officer (LSO) Basic Areas of Controls • Administrative Controls • Procedural Controls • Maintenance and Service • Establish Laser Controlled Areas 18 VI. Responsibility And Authority Of The Laser Safety Officer (LSO) The Laser Safety Officer (LSO), under the supervision of a Medical Physicist, will be responsible for the knowledgeable evaluation and control of laser hazards, and has the authority to monitor the use of laser equipment and to enforce regulations for the control of laser hazards. The Medical Physicist may also be designated the LSO. In the absence of a designated LSO, JCAHO considers the institutional Radiation Safety Officer (RSO) responsible for LSO functions. Consultative Services The LSO will provide consultative services for evaluation of laser hazards and controls for personnel training programs. Such evaluation will include electrical and other non-radiation hazards of lasers, but does not encompass performing such tasks, which are the appropriate domain of the laser service engineer. The LSO will provide consultative services for evaluation of laser environment and plume effects and in matters related to epidemiology and risk management. Regulations The LSO may establish and maintain adequate regulations for the control of laser hazards. Such regulations will meet compliance requirements of FDA/CDRH, ANSI Standards Z136.1 and Z136.3, and state regulations (e.g., Massachusetts Department of Public Health regulations 105 CMR 121). The LSO is also responsible for compliance with federal, state, and other regulations regarding laser installation, the laser safety program, and registration with appropriate regulatory agencies. 19 Responsibility and Authority Of The LSO Authority The LSO will have the authority to suspend, restrict or terminate the operation of a laser or laser system if he/she deems that laser hazard controls are inadequate. Records The LSO will ensure that the necessary records required by applicable government regulations are maintained. The LSO will ensure that applicable medical surveillance examinations have been scheduled and performed, that appropriate training has been provided, and that appropriate documentation has been completed and submitted to the appropriate administrative office. Surveys and Inspections The LSO will survey by inspection, as considered necessary, all areas where laser equipment is used. The LSO will also accompany regulatory agency laser equipment inspectors, such as those representing OSHA, FDA/CDRH, state agencies, etc., and document any discrepancies noted. The LSO will ensure that corrective action is taken where required. Accidents On notification of a known or suspected accident resulting from operation of a laser, the LSO will investigate the accident and initiate appropriate action. This may include the preparation of reports to applicable agencies. It is recommended that AAPM, ACMP, FDA or Laser Institute of America (LIA) establish a device/incident reporting system for medical lasers. This system could also serve as a clearinghouse for manufacturer/user information. 20 Responsibility and Authority Of The LSO Approval of Laser System Operation Approval of a laser or laser system for operation will be given only if the LSO is satisfied that laser hazard control measures are adequate. These include special operating procedures for maintenance and service operations within enclosed systems and operational procedures for Class IIIB and IV systems. The procedures will include adequate consideration to assure safety from electrical, mechanical, procedural, and laser hazards. Other Related Responsibilities • Evaluate possible hazards and institute appropriate control measures and training • Ensure evaluation of the Nominal Hazard Zone (NHZ) for each laser system • Evaluate a pre-op and post-op safety checklist for each laser procedure • Establish guidelines for safety eyewear and other safety equipment and assure proper selection and usage for each laser system • Ensure all lasers are used according to hospital standards • Monitor quality control procedures and conduct radiation safety audits • Establish Maximum Permissible Exposure (MPE) for personnel compliance standards for health care personnel • Establish training guidelines, personnel categories, and credentials for operators and users of medical lasers. Refer to Procedure #1 21 Responsibility and Authority Of The LSO Deputy Laser Safety Officers If necessary, Deputy Laser Safety Officers will be appointed by management in consultation with the LSO. The Deputy Laser Safety Officer (e.g., Laser Nurse) will perform the functions of the LSO when the latter is not available. 22 VII. Quality Control And Radiation Safety The Quality Control (QC) and Radiation Safety (RS) tests as recommended by all the standards are presented in the format of the ACMP document published in 1991, “Radiation Control and QA of Medical Laser Systems.” The parameters include basic QC and service tests, reasons for conducting such tests, references to the ANSI standard sections, and reasonable frequency of such tests. These parameters are included to help resolve some of the concerns involved in clinical use of medical laser systems. The appropriate tables and sample copies of forms for use are referenced and included in later sections of this report. The measurements and evaluations described in this protocol are intended for annual or otherwise routine surveys. They are considered the minimum acceptable for a properly managed medical laser service. Similarly, the method of testing a particular parameter is not specified. For some measurements and tests other equally effective methods are available. The choice is left to the professional judgment of the qualified expert. 23 Quality Control And Radiation Safety PARAMETER REASON CRITERIA/FREQUENCY A. PHYSICAL INSPECTION OF EQUIPMENT AND ACCESSORIES 1. ELECTRICAL AND COOLING 2. 3. a. Mechanical and electrical integrity of plugs, wires and outlet. b. Check water hoses for leaks and wear. Visual inspection of equipment to determine mechanical malfunction or electrical hazard which may lead to improper operation of equipment or hazard to patients or personnel. Before each use. Good safety practice Each day of use CHEMICAL AND SMOKE a. Check gas tanks, valves and fittings for leaks. b. Insure tanks are not creating an obstacle. " " c. Do not expose tanks to Temp. above 125 degrees F. " " d. Cylinder valves must be closed when not in use. " " e. Smoke evacuation system must be employed when applicable. " " f. Gas tanks must be properly secured. " " WARNING SIGNS Proper labeling by Laser-Type a. Post on Doors. b. Post on Lasers. Warn personnel and protect staff. " Each case. " 4. EYEWEAR a. Labeled OD and wavelength. b. Periodic cleaning and inspection. c. Check for cracking, discoloration, leaks. d. Ensure proper eyewear used with type of Laser-In-Use. Visual inspection to insure integrity of eyewear, to confirm adequate number are available, and to confirm that appropriate wavelength filters are used. ANSI Z136.1, 4.2.2-4. As determined by the institution or LSO. Visual inspection to insure integrity of eyewear, to confirm adequate number are available, and to confirm that appropriate wavelength filters are used. ANSI Z136.1, 4.6. As determined by the institution. 24 Quality Control And Radiation Safety PARAMETER REASON CRITERIA/FREQUENCY a. Check for light leaks. To prevent unwanted exposure to personnel and patient. Before each use. b. Check that filter is in optical chain/microscope. When necessary to protect surgeon. Each use. Electrical Safety. ANSI Z136.3, 7.2. 5. FILTERS AND OPTICS B. LASER SAFETY 1. ELECTRICAL HAZARDS a. All HCLS shall be installed & operated in conformity with the National Electrical Code (NFPA70), OSHA, JCAHO, and Related State & Local laws and regulations. b. Interlocks and removable protective housing. c. Audits, i.e., damaged cords & cables, not properly grounded equipment, not returned to original operating condition, proper training, etc. " ANSI Z136.1, 4.3.2. To avoid electrical shock. ANSI Z136.3, 7.2. 2. COMBUSTION HAZARDS a. Saturate gauze, drapes, tape, etc., with normal saline. Dry materials are highly flammable when irradiated by laser beam. Each use, depending on laser in use. b. Use with non-combustible materials. Insure ventilation techniques, shielding with wet substrates. To avoid potential for release of chemical vapors and to avoid burns. ANSI Z136.3, 7.5.1. c. Use caution with flammable anesthetic gases. Low combustion gas (Helox) mixtures. To avoid explosion. ANSI Z136.3, 7.5.1. d. Rooms should be equipped with a portable fire extinguisher in keeping with NFPA or state and local building codes. For Emergency Use. ANSI Z136.3, 7.5. e. Use non-flammable endotracheal tubes, FDA approved tubes and tube wrapping. Protect inflated cuff with wet cotton towelettes. To prevent laser penetration and/or ignition of tube. ANSI Z136.3, 7.5.1. f. Test all “Laser Safe” products in use. To prevent fires, explosion and ignition of products used. Each new batch. To ensure that personnel exposures are within safety limits. ANSI Z136.3, See Tables 1A, 1B. 3. NOMINAL HAZARD ZONES a. Establish and post limits of NHZ. 25 Quality Control And Radiation Safety PARAMETER b. 4. Consideration given to room design, proper ventilation, exhaust, windows & viewing areas. REASON CRITERIA/FREQUENCY Highly reflective areas limited. ANSI Z136.3, 7.10. To avoid laser damage to personnel. ANSI Z136.1, Tables 5, 6, 7; ANSI Z136.1.8; ANSI Z136.3, See Table A2. MAXIMUM PERMISSIBLE EXPOSURE a. Establish and post MPE times. 5. PERSONNEL SAFETY a. Eye protection mandatory for Class IIIB and IV lasers, Collateral & Plasma Radiation. To filter out harmful, often invisible laser energy. ANSI Z136.1, 4.6 / Each case. b. Laser warning signs should be posted outside room where laser is being used. Prevents personnel from entering room without wearing protective glasses. ANSI Z136.1, 4.7 / Each case. c. Ventilation of airborne contaminants and plume control. Protects personnel from inhaling noxious fumes. ANSI Z136.3, 7.4 / When necessary. d. Cover windows with non-reflective material. To avoid inadvertent exposure to direct or scattered laser radiation. When necessary. e. Permit only experienced personnel to operate laser; use key switch for security. Insures use of laser by experienced and approved staff. ANSI Z136.3, 5 Institutional-Policy and Procedures. f. Eliminate unnecessary specular (mirror-like) surfaces. Prevents accidental exposure to laser radiation. ANSI Z136.3, 5 Institutional-Policy and Procedures. g. Medical surveillance: Baseline eye examinations; Class IIIB and IV. Protects institution. ANSI Z136.3, 6 / Determined by LSO and Institutional Health Service. h. Further information of value to examination by attending physician. For follow up. ANSI Z136.1 / (2000) Appendix E. 6. PATIENT SAFETY a. Eye protection for Class IIIB and IV lasers mandatory. Method approved by LSO. Prevents damaging exposure to patient’s eyes. ANSI Z136.3, 4.4.4. b. Use moistened eye pads over taped eyes. Reduces accidental skin burns and exposure. Depending on laser in use. Every patient when applicable. c. Surgical field covered with wet towels. Reduces accidental skin burns and ignition of drapes. Policy/Procedures. d. Reflective objects must have a dull, non-reflective finish or be draped. Avoid reflecting potentially harmful laser beam. Policy/Procedures. 26 Quality Control And Radiation Safety PARAMETER REASON CRITERIA/FREQUENCY e. Smoke evacuation system & wall suction are the two major types of local exhaust ventilation. To prevent patient and medical staff from inhaling noxious fumes. Reduces LGAC levels. ANSI Z136.3, 7.3.2 & 7.3.2.1 / Depending on laser in use. f. Know emergency action for fire. To prevent panic, insure quick and knowledgeable response. Every patient when applicable. g. Be familiar with management of endotracheal fire. To prevent panic, insure quick and knowledgeable response. Part of Disaster Plan. C. OUTPUT MEASUREMENTS AND QUALITY CONTROL 1. MEASUREMENTS a. Output (power/energy measurements). To insure proper power/energy is delivered. Accuracy ±20% / Monthly. b. Accuracy of exposure. To insure timing accuracy. See Sample Form #1 or Form #2. 2. CLEANING a. Mirror. To insure proper output. As necessary. b. Surface ends and types of Fiber Optics. To allow proper delivery. As necessary. c. Smoke Evacuation Filter. For safety of personnel and patient. As necessary. Visual inspections to determine mechanical malfunctions which may lead to improper operation of equipment or hazard to patients or personnel. Monthly – See Sample Form #1 or Form #2. 3. INSPECTIONS a. Eyewear. b. Electrical. Daily. c. Signs. Daily. d. Laser Use Logs. " Daily. e. Safety Interlocks. " Daily. 4. ALIGNMENT a. Mirror. To allow proper power delivery. Each Use. b. Beam. To allow proper power delivery. Each Use. c. Coincidence of Aiming. To insure accurate radiation delivery of laser. Each Use. 27 Quality Control And Radiation Safety PARAMETER REASON CRITERIA/FREQUENCY To insure effective and safe delivery of appropriate laser therapy. To insure effective and safe delivery of appropriate laser therapy. Daily/laser dependent. 5. LASER OPERATOR CHECKLIST a. Pre-op/Post-op. b. SOPs. c. Daily start-up. " d. Laser user log. " See Sample Procedure #2. " See Sample Form #3. D. EDUCATION AND TRAINING 1. DEVELOP A TRAINING PROGRAM a. Education. b. Didactic Training. c. Practical Experience. d. Criteria to Credential Laser User. ANSI Z136.3, 5 / (1996). Appendix D, Tables D1, D2. To insure that staff is properly trained in laser use and safety, e.g., Health Care Professionals, Laser Technicians, Service Engineers, etc. As determined by institution using laser. See Sample Procedure #1. See sample Form #4. 2. LSO RESPONSIBILITIES To insure compliance and radiation safety. ANSI Z136.3, 1.3 / (1996). E. SUMMARY OF CONTROL MEASURES To insure Administrative, Engineering Preventative Maintenance, Clinical, Radiation Safety and Operation Controls. ANSI Z136.3 / (1996) and ANSI Z136.1 / (2000). For major use in treatment of lesions in Gynecology, Neurosurgery, General Surgery, Dermatology, Urology, Opthalmology, Gastroenterology, and Otolaryngology. ANSI Z136.3 / (1996) Appendix B gives a detailed survey of clinical operations. F. CLINICAL LASER SYSTEMS CO2, Argon, Nd-YAG, Dye Laser Eximer, solid state, etc. Continuous or pulsed exposure to be grouped by laser type. G. EQUIPMENT TESTING/ CLINICAL USE 1. Laser must be in normal working order. Patient and Operator Safety. Before each use. 2. The focusing lens of colposcope (in GYN applications) and lens of the laser attachment must have the same focal length. To avoid uncontrollable damage to target tissue causing blistering and extension of heat coagulation zone. Before each use. 3. Ensure proper coupling of an articulated arm to the micromanipulator of the colposcope. Misalignment in coupling may misdirect an active laser beam towards anesthetists, nursing staff or patient. Before each use. 28 Quality Control And Radiation Safety PARAMETER REASON CRITERIA/FREQUENCY 4. All foot pedal controls should be covered. Operator should remove foot from shutter control pedal and put laser in standby when not actually using laser. To prevent accidental laser exposure. Policy/Procedures. 5. When using a laser hand-piece in a sterile field, a sterile stockinette should be taped at least 4 cm above aperture of the laser hand-piece. To prevent slippage into the beam and ignition of the sterile covering. Policy/Procedures. 6. Ensure anodized or matte-finish surgical instruments are used when laser is present. To reduce potential for damage to the eye by scattered energy from visible and infrared lasers. Check before each use. 7. Only quartz or diffusely reflective metal should be placed behind adhesions which are to be severed by lasers. Glass rods should not be used. The thermal stress may cause breakage of glass rods and fragments may be lost in the cavity. Policy/Procedures. 8. Ensure use of eye protection of adequate optical density and that it is designed for wavelength of the laser used. To prevent damage to the cornea, lens, or retina (depending on wavelength). Before each use. 9. Effective Fume and Plume control either by suction or special devices is imperative. To eliminate offensive odors and cellular debris, vapors, etc., thus providing greater visibility for increased precision. Also to prevent dispersion of neoplastic debris. Before each use. 10. Carbon must be removed from the treated surfaces by suction or irrigation. To prevent initiation of a foreign body giant-cell reaction due to excess carbon deposits and fire. Policy/Procedures. 11. Ensure that lasers are used at highest controllable power settings and are highly maneuverable. To avoid lateral thermal damage to the surrounding tissues. Carbonized impact sites must not be lasered repeatedly. Impact sites must be wiped clean of carbon. Policy/Procedures. 12. Masks should be worn by all personnel. Proper plume control devices should be used. To avoid inhalation of biologically active material. Policy/Procedures. 13. Do not prepare operating field with volatile agents or drape with dry towels or paper. To prevent a flash fire when laser beam strikes a volatile area of the operating field. Policy/Procedures. 14. Avoid high-frequency ventilation system when operating through microscope. Motion of the surgical field makes target focusing difficult. ANSI Z136.3 / (1996) Policy/Procedures. 15. Non-explosive anesthetics and localized ventilation techniques are mandatory for digestive and endotracheal operations. Methane gas in the digestive tract or oxygen concentration in the aerodigestive tract poses danger of an explosion. ANSI Z136.3 / (1996) Policy/Procedures. 29 Quality Control And Radiation Safety PARAMETER REASON CRITERIA/FREQUENCY 16. Thorough understanding of biological tissue and interaction of different laser wavelengths of laser system is essential. Thermal mechanism (vaporization, photocoagulation), mechanical and nonthermal effects and photochemical reactions are possible. ANSI Z136.3 / (1996) See Table 4. 17. Alignment of CO2 and Nd:YAG laser beam with coaxial HeNe aiming laser much be checked in each case. Focusing and coaxial orientation can be checked with beam aimed at wet tongue depressor. Policy/Procedures. 18. Do not use a laser with the articulated arm unattached or disconnected from a micro-manipulator or other attachment. Laser beam can be directed accidentally toward personnel or patient. See Procedure #3. 19. Eye protection for operating personnel must be appropriate for each laser wavelength and beam intensity. Examples: - For CO2 laser, clear plastic goggles or glasses with side shields. To absorb reflected energy and protect the cornea or retina of the eyes. Policy/Procedures. 20. Eye protection for the patient is necessary; metal and acrylic eye shields for laser treatment over eyelid area; moistened eye pads placed over taped eyes, overlaid with a wet sponge for use of a laser near the eyes; in addition, for Nd-YAG laser therapy, aluminum foil layered over the eyes. To protect the patient’s eyes from damage. Policy/Procedures. 21. Endotracheal tubes of red rubber with aluminum wrap for CO2 laser in the aerodigestive tract, PVC endotracheal tube for Nd-YAG laser. To avoid burning of the patient’s endotracheal passage. Policy/Procedures. 22. Windows should be covered when using a Nd-YAG laser. To protect personnel from laser light reflected from the windows. Policy/Procedures. - For Argon laser, amber tinted goggles will permit viewing of Argon wavelengths. - For Nd-YAG lasers, goggles specifically designed for 1.06 µm wavelengths are necessary. - With rigid and flexible bronchoscopes, wavelength specific filters protect the surgeon’s eyes. - Do not look directly at the laser beam of a HeNe laser. 30 VIII. Laser Safety Procedures (LSP) For Clinical Use The Laser Safety Procedures (LSP) are given for practical and easy use in routine operations. The LSP #1 through #8 are grouped to include all aspects of use of medical lasers in health care facilities. The LSPs serve as a quick reference guide to develop and implement a Laser Safety Program that will comply with recommendations of existing standards. LSP #1 - All persons should be aware of area of use and controlled access to these areas must be maintained. • The nominal hazard zone (NHZ) should be identified to prevent unintentional exposure to laser beam • The NHZ should be occupied by authorized personnel • Personnel in NHZ should be aware of all laser safety precautions • Regulation laser signs should be placed in all entrances to warn on-lookers of potential hazard • Doors in NHZ should remain closed and windows covered LSP #2 - Everyone in NHZ should wear appropriate eyewear approved by LSO. • The protective eyewear should be appropriate to wavelength used and labeled with appropriate Optical Density • Patient’s eyes and eyelids should be protected by wet eyepads, laser protective eyewear, eyeshields, etc. LSP #3 - Exposure to smoke plume generated during Laser Surgery should be reduced by implementing a variety of engineering controls. • High filtration surgical masks • Wall suction units with in-line filters • Smoke evacuator units 31 Laser Safety Procedures (LSP) For Clinical Use • Smoke plume has mutogenic and carcinogenic potential. There is also an unidentified potential for bacterial and viral contamination LSP #4 - All persons in laser treatment area should be protected from laser beam exposures to their skin and other non-targeted tissues. • Exposed tissues around the operative site should be protected with saline-saturated fire/flame retardant materials • Anodized, dull, non-reflective or matte-finished instruments should be near the laser site • When a fiber is used to deliver laser energy through an endoscope, the end fiber must extend beyond the end of the endoscope. Most flexible fiber-optic endoscope sheaths are flammable and are easily damaged by heat LSP #5 - All persons in laser treatment area should be protected from flammability hazards associated with laser usage. • Fire is one of the significant hazards of laser use • The intense heat of laser beams can ignite combustible/flammable solids, liquids, and gases • Free flow of high oxygen can lead to rapid spread of flames • Fire extinguishers and water/saline should be immediately available • Endotracheal tubes used in patient’s airway should have protection to minimize fire hazard. Standard endotracheal tubes are combustible LSP #6 - All personnel should be protected from electrical hazards associated with laser use. • Visual inspection of laser equipment should be done after setup for use 32 Laser Safety Procedures (LSP) For Clinical Use • Laser service and preventive maintenance should be documented. LSO should review records and approve equipment use after service LSP #7 - Personnel working in NHZ should demonstrate competency commensurate with their responsibilities. • Surgeons, laser operator (nurse), LSO or designee, biomedical technician, and other health care personnel • Education and training programs should be specific to laser systems and procedure used in the facility • Personnel should be required to demonstrate periodically and to complete competency checklist for new laser systems and accessories before use LSP #8 - Policies and procedures for laser safety should be developed with regard to individual practice settings, acceptable standards, and federal and state regulations. • Policies and procedures should be reviewed periodically, revised as necessary, and readily available to personnel • Establish guidelines for Quality Assessment • Laser Safety Committee and structure • Administrative and Procedural Controls • Education and Training Programs • Medical Surveillance and Safety Audits • Laser Service and Maintenance 33 IX. Useful Data And Tables Table 1A NHZ Distances for Selected Surgical Lasers Without Delivery System Constraints MPE Exposure Time Criteria(s) Diffuse* NHZ (m) Laser with Lens** CW Visible*** 400–700 nm 0.25 None 3.6 500 CW Nd:YAG 1064 nm 10 0.79 6.37 500 CW CO2 10,600 nm 10 0.18 2.38 178 1–20 ⋅ 10-9 None 0.45 226 Laser Type Q-SW Nd:YAG 1064 nm Laser without Lens * It is assumed that worst-case reflection (ρ = 1) and worst-case viewing angle (cos θ = 1) prevail, viewing distance >20 cm. ** Distance from focus. *** HeNe, Argon, dye, etc. Table1B Laser Criteria Used for NHZ Distance Calculations Laser Parameter Wavelength (nm) CW Visible 400–700 CW Nd:YAG 1064 CW CO2 10,600 Q-SW* Nd:YAG 1064 Beam power (W) 5 100 100 -- Beam energy (mJ) -- -- -- 2 Beam divergence (mrad) 1 2 2 1 Beam size at aperture (mm) 2 2 20 25 Beam size at lens (mm) 3 6.3 30 25 Lens focal length (mm) 200 25.4 -- 5.1 × 10 1.0 × 10 -- MPE (µW / cm2) @ 0.25 s 2.5 × 103 -- -- -- MPE (µJ / cm2) @ 1–20 ns -- -- -- 5 2 MPE (µW / cm ) @ 10 s 200 3 * Typical for ophthalmological use. 35 50 5 Useful Data And Tables Table 2 MPE Limits for Selected Surgical/Medical Lasers Laser Type Exposure Time (seconds) 10** 600*** MPE (mW · cm −2) --- Wavelength (nm) 0.25* ArF 193 -- XeCl 308 -- -- -- 0.0013 XeF 351 -- -- -- 0.0333 Argon 514 2.5 -- 0.0167 0.001 Krypton 530 568 647 2.5 2.5 2.5 -- 0.0167 0.031 0.363 0.001 0.00186 0.0285 Dye Laser (a) 630 2.5 -- 0.263 0.0158 He-Ne 633 2.5 -- 0.293 0.0176 GaAs (CW) 840 -- 1.9 0.69 0.610 Q-switched (b) 1064 -- 0.017 0.0061 0.0023 Nd:YAG (CW) 1064 -- 5.1 1.82 1.6 Nd:YAG (CW) 1330 -- 40 14.5 13 10,600 -- 100 100 100 30,000**** 0.0001 (diode) Nd:YAG CO2 (a) Argon laser pumped Rhodamine 6-G dye laser used in PDT therapy. (b) Repetitively pulsed @ 11 Hz, 12 ns pulses. * Aversion response time. ** Unintentional viewing at wavelengths greater than 700 nm, with no visible component. *** Intentional viewing of diffuse reflections from small sources (less than αmin). **** Cumulative exposure, 8-hour working day. 36 Useful Data And Tables Table 3 Control Measures for the HCLS (American National Standard Z136.3 – 1996) 1 3b 4 Research (4.1.1) X X Administrative Controls (4.2) X X Laser Use Committee (5.1) X X Maintenance and Service (4.2.1) X X Standard Operating Procedures (4.2.2) X X Authorized Personnel (4.2.3) X X Equipment Controls (4.3) X X Guarded Switch (4.3.1) X X Beam Delivery Disconnect Safety Features (4.3.2) X X HCLS Warning Labels (4.3.3) 2a 2 3a X X X X X Service and Repair of HCLS (4.3.4) X X X X X X Modification of HCLS (4.3.5) X X X X X X X X Quality Control and Safety Audits (4.3.6) • HCLS Output Calibration (4.5.1.1) Area Posting Sign (4.4.2.1) Environment in which Laser is Used (4.4.1) ** ** • • X X • • X X ** ** ** ** X X Laser Treatment Controlled Area (4.4.2) Optical Fiber Surgical Probes (4.4.3) ** ** Alignment Procedures (4.5.1) ** ** ** ** X X X X X-NHZ X-NHZ X X X-NHZ X-NHZ Patient Eye Protection (4.4.4) Service Personnel (4.5.2) X X X X Protective Eyewear (4.6.2) Protective Clothing (4.6.4) ** Warning Signs / Labels (4.7) Explosion and Fire Hazards (7.5) Legend: X X-NHZ • ** ** ** ** ** ** •/X •/X •/X •/X •/X X - Shall - Shall within the NHZ - Should - LSO shall establish alternate controls 37 Useful Data And Tables Table 4 Wavelength Effects for Various Lasers Laser Type Wavelength (nm) Mechanism Skin Tissue Affected Cornea Lens Retina ArF (Pulsed) 193 Photodissociative X X XeCl (Pulsed) 308 Thermal/Photodisruptive X X (a) (a) He-Cd (CW) 325 Thermal/Photodisruptive X X X X XeF (Pulsed) 351 Thermal/Photodisruptive X X X Argon (CW) 488 – 514 Thermal/Photodisruptive X (b) (KTP) (Pulsed) 532 Thermal/Photodisruptive X X He-Ne (CW) 633 Thermal X 780 – 950 Thermal X Doubled Nd:YAG GaAs (Pulsed) (diode) Nd:YAG (Pulsed) Thermal/Photoacoustic X 1064, 1330 Thermal X X Erbium:YAG (Pulsed) 1540 Thermal X X Holmium:YAG (Pulsed) 2100 Thermal X X 2730 Thermal X X 2940 Thermal X X 10,600 Thermal X X Nd:YAG (CW) 1064 X Hydrogen Fluoride (Pulsed) Erbium:YAG (Pulsed) CO2 (CW) (a) Simultaneous cornea/lens/retinal effects observed in some biological studies. (b) Photochemical effects dominate for long term exposures of retina (exposure times >10 sec.). 38 X X Useful Data And Tables Table 5 Laser Safety Training Program MD RN Tech Service LSO 1) Laser Physics/Biological Effects X X X X X 2) System Components/Delivery Devices/ X X X X X Instrumentation 3) Federal, State, Local Regulations X X X X X 4) ANSI Z136.3 Standards X X X X X 5) Institutional Policy/Procedures X X X X X 6) Hazard Classification X X 7) Access to Laser Key 8) Medical Surveillance 9) X X X X X Documentation/Incident Reporting X X 10) Anesthesia Hazards/Controls X X X 11) Personal Protective Equipment X X X 12) Patient Protection X X X 13) Operational Skills Workshops X X X 14) Procedure for Safety Audits X X X X X X X X X 39 X. Sample Forms 40 FORM #1 BAYSTATE HEALTH SYSTEM BAYSTATE MEDICAL CENTER LASER QUALITY ASSURANCE DEPT: _________________________________________________________ LASER: _______________________________________________________________ DATE: _________________________________________________________ INSPECTED BY: ___________________________________________________ MONTHLY INSPECTION BEAM ALIGNMENT (DAILY) INTERLOCKS SIGNS - DOORS SIGNS - SYSTEMS OUTPUT (SEE POWER MEASUREMENTS) LASER LOG (EACH CASE) MIRROR CLEANING (AS NEEDED) SMOKE EVACUATOR USED (AS NEEDED) SMOKE EVACUATOR CLEANED (AS NEEDED) EYEWEAR AVAILABLE COVER WINDOWS (WHERE NECESSARY) VISUAL CHECK (ELECTRICAL) LASER POWER MEASUREMENTS WATTS SET WATTS MEASURED %DIFFERENCE Medical Physicist: ______________________________________________________________ OR Laser Safety Officer: ____________________________________________________________ 41 FORM #2 QUALITY CONTROL OF MEDICAL LASERS DEPT. ___________________________________________________ LASER __________________________________________________ DATE ___________________________________________________ BEAM ALIGNMENT (DAILY) INTERLOCKS SIGNS OUTPUT CALIBRATION (POWER/ENERGY/MEASUREMENT) LASER LOG MIRROR CLEANING/ALIGNMENT (AS NEEDED) FIBER OPTICS CLEANING SMOKE EVACUATOR CLEANING SAFETY DOORS SIGNS SYSTEMS EYEWEAR 1. LABELED W/O.D. AND WAVELENGTH (MONTHLY) 2. INSPECTION (MONTHLY) a. CRAZING, CRACKING, DISCOLORATION b. CHECK FRAME c. CHECK FOR LIGHT LEAKS COVER WINDOWS AND RESTRICT ENTRY WHERE NECESSARY ELECTRICAL AND H20 HAZARDS/VISUAL CHECK LEAKS/FRAYED WIRES (DAILY) SMOKE EVACUATOR IN USE WHEN NECESSARY PATIENT PROTECTION TESTING LASER SAFETY ACCESSORIES IN O.R. 42 MONTHLY QUALITY CONTROL AND LASER INSPECTION INSPECTED BY: _________________ FORM #3 LASER LOG AND RECORD Place pt. label here DATE: yes o no o Type of anesthesia _______________________ Microscope used: MDA __________________________________ Microscope lens _______________ min GRNA _________________________________ Free hand yes o no o n/a o Anesthesia Resident ______________________ Scanner: yes o no o n/a o Laser Nurse _____________________________ Fiber used: yes o # _____ n/a o Circ. Nurse _____________________________ Scrub Nurse ____________________________ Laser time activated ______________________ Other Personnel _________________________ Laser time deactivated ____________________ _______________________________________ Laser mode(s) used _______________________ _______________________________________ Watts used _____________________________ Laser Type _____________________________ Total joules _____________________________ Serial # ________________________________ Total pulses _____________________________ Diagnosis ______________________________ Time sec. ______________________________ Procedure ______________________________ _______________________________________ Windows Covered yes o n/a o Eye protection used on patient: 1. Saline moistened eye pads taped in place o 2. Aluminum foil over eye pads taped in place o 3. Green tinted Yag laser glasses o 4. Clear plastic CO2 laser glasses o Laser mouth guard used on patient yes o no o n/a o Comments:________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ 43 FORM #4 LASER PRIVILEGE APPLICATION FORM Category: Physicians 1. Name: ______________________________________________________________________ 2. Department: _________________________________________________________________ 3. Address: ____________________________________________________________________ 4. Date: _______________________________________________________________________ 5. Laser Training: _______________________________________________________________ _______________________________________________________________ A. Courses: Name: ___________________________________________________________________ Date: ____________________________________________________________________ Location: _________________________________________________________________ Hours - Didactic (8 hours minimum): __________________________________________ Hands On (4 hours minimum): _________________________________________ (Attach supplemental sheets if necessary) Please enclose certification from laser courses B. Residency Fellowship Laser Experience (if applicable): Institution: ________________________________________________________________ Department: _______________________________________________________________ Department Chairman: ______________________________________________________ (Enclose letter from department chairman regarding laser proficiency. See general guidelines) 44 LASER PRIVILEGE APPLICATION FORM-PAGE 2 C. Other (e.g., Preceptorship etc. – explain) _______________________________________________________________ _______________________________________________________________ _______________________________________________________________ 6. Type of Laser: 6. _______ CO2 7. _______ Nd Yag 8. _______ Dye 9. _______ Argon 7. Prior case experience as primary laser therapist (please enclose copies of operative note reports with patient name removed to preserve confidentiality): Laser Wavelength or Type of Laser Procedure Complications DATE: (e.g., CO2, Argon, Dye, Yag) 1. ________________________________________________________________________ 2. ________________________________________________________________________ 3. ________________________________________________________________________ 4. ________________________________________________________________________ 5. ________________________________________________________________________ FOR LASER COMMITTEE ONLY 8. Institution Preceptorship Cases: Preceptor: Laser Wavelength or Type of Laser Procedure Complications DATE: (e.g., CO2, Argon, Dye, Yag) 1. ________________________________________________________________________ 2. ________________________________________________________________________ 3. ________________________________________________________________________ 4. ________________________________________________________________________ 5. ________________________________________________________________________ 45 FORM #5 LASER OPERATOR SKILLS VALIDATION 1. Applicant has read policies and procedures. ___________ 2. Certificate of attendance at an approved course of not less than ________CEUs, has been submitted. ___________ 3. Passed the baseline eye exam. ___________ 4. Attended equipment in service by LSO. ___________ 5. Knows security procedure for obtaining keys. ___________ 6. Follows safety precautions while setting up the room and assembly equipment. ___________ 7. Knows how to assemble laser delivery systems, and accessory equipment. ___________ 8. Can perform daily maintenance procedures. ___________ 9. Operates control panel properly: power settings ___________ time exposure ___________ standby/ready ___________ emergency off ___________ shutter ___________ 10. Test fires / calibrates laser output. ___________ 11. Assembles, checks, operates smoke evacuator system. ___________ 12. Positions laser, footpedal, and delivery systems. ___________ 13. Completes all documentation. ___________ 14. Knows proper methods for cleaning and storing. ___________ 15. Demonstrates ability to monitor a laser safe room. ___________ 46 FORM #6A COMMONWEALTH OF MASSACHUSETTS DEPARTMENT OF PUBLIC HEALTH RADIATION CONTROL PROGRAM APPLICATION FOR REGISTRATION OF A LASER FACILITY NOTE: Registration is required only for facilities using ANSI Class 3b or 4 lasers. FACILITY NAME: ___________________________________________________________________ ADDRESS: _____________________________________________________________________ CITY: __________________________ STATE: ____________ ZIP CODE: __________ FACILITY TELEPHONE NUMBER: _______________________________________________ NAME OF THE CONTACT PERSON AT THE FACILITY REGARDING THE USE OF THE LASER(S): _________________________________________ TITLE: ___________________ TELEPHONE NUMBER: ________________________________________________________ NAME OF THE LASER SAFETY OFFICER (LSO): _______________________________________ ADDRESS OF THE LSO, IF OTHER THAN THAT OF THE FACILITY: ADDRESS: ___________________________________________________________________ ___________________________________________________________________ CITY: __________________________ STATE: ____________ ZIP CODE: __________ RSO TELEPHONE NUMBER: ___________________________________________ NATURE OF THE LASER FACILITY’S LASER USE: o industrial processing o optical fiber communication systems o industrial research o education o entertainment (i.e., laser light show) o health care o manufacturer of lasers or laser containing products Please complete and attach an INVENTORY OF ANSI CLASS 3b and 4 LASERS Form I, ________________________________(as the facility owner or the designee for the owner) certify that the above named facility is complying with the applicable requirements of the American National Standards Institute Z136 Guidelines and 105 CMR 121.000. SIGNATURE and DATE: ______________________________________________________________ 47 48 Laser Manufacturer Laser Model Laser Serial Number o 3b o 4 o 3b o 4 o 3b o 4 o 3b o 4 o 3b o 4 (check one) ANSI Z136.1 Laser Class Laser Medium Describe the Application for Which the Laser is Being Used. FACILITY: _____________________________________________________________DATE: ___________________________ INVENTORY OF ANSI CLASS 3b AND 4 LASERS FORM #6B XI. Operational Procedures Procedure #1 - Standards for Approval of Laser Use by Health Care Professionals Education V. Licensed physicians, registered nurses*, certified technologists or allied health science professionals with Bachelors degrees in physical sciences or engineering. *Note: Specific credentials for human use of lasers for different categories will be established by the Laser Safety Committee. Copies of present requirements used at Baystate Medical Center, Inc., are enclosed. e.g. , Categories: Physicians Nurses Laser Technicians Knowledge and Didactic Training 1. Fundamentals of laser radiation 2. Bioeffects of laser radiation 3. Relations of specular and diffuse relations 4. Laser standards and regulations 5. Radiation and non-radiation hazards 6. Safety policies and control procedures 7. Medical surveillance and ancillary problems Practical Experience 8. Document at least four (4) to six (6) hours of “hands-on” experience in use and operation of lasers 49 Operational Procedures Policy/Category: Standards to Credential Physicians in Laser Therapy Purpose 1. To establish a criterion for delineation of privileges for laser therapy. 2. To assure safe use of laser therapy both for patients and health care personnel. Recommendations 1. All physicians utilizing the laser must be recommended by the Laser Committee for use of specific wavelengths and type of laser. 2. The Laser Committee shall forward its recommendations to the appropriate department chairman concerning approval of application for laser privileges. 3. The following are general guidelines established by the Laser Committee for the use of all lasers. In addition, the various departments/divisions shall establish their own guidelines, which shall have been submitted to the Laser Committee for approval. New applicants would be required to fulfill both the general and the more specific requirements. General Guidelines A. Laser training courses must be taken including at least 8 hours didactic lectures—documentation is required. B. At least 4 hours of direct hands-on experience with lasers either in the laboratory or in human therapy must be documented. 50 Operational Procedures C. The laser operator must have performed a minimum of 3 cases utilizing a specific wavelength and type of laser in an assistant or primary role prior to the granting of specific laser privileges. Documentation is required. D. Physicians trained in laser therapy while in residency or fellowship should have a letter from the department chairman stating that the applicant has met the above requirements and has a proficiency in laser therapy. E. There shall be a preceptorship required for all physicians applying for specific wavelength and type of laser privileges. The exception will be recommendation #5 (see below). F. Privileges and permission to use laser systems are subject to laser safety and quality control procedures established by the Radiation Safety Committee to meet regulatory compliance requirements and national standards. 4. Physicians utilizing a particular laser for the first time in human therapy at the institution shall have a physician from the institution previously credentialed in that particular therapy present at the first 3 cases in a preceptorship role. This preceptor shall then make recommendations to the Laser Committee regarding the applicant’s proficiency with regard to laser therapy. 5. New laser technology and therapy shall not be discouraged at the institution. In the event that no physician in the institution is clinically experienced in the specific new technology or application, that physician will be considered for the recommendation of privilege after review by the Laser Committee providing adequate education is documented. 51 Operational Procedures 6. Any experimental or research protocols involving the laser shall be prospectively reviewed by the Laser Committee. Recommendations shall be forwarded to the appropriate committee or chairman. Note: Other categories included are: Nurses Laser Technicians Policy/Category: Standards to Credential Nurses in Laser Therapy Credentialing of Nurses 1. All institutional nursing staff assisting physicians in laser therapy must complete the nursing orientation program. 2. Clinical laser workshops include: a. Four hours of didactic lectures b. Two hours of hands-on laboratory experience The Role of Laser Nurses 1. Laser nurses should be fully knowledgeable about the operation handling and minor troubleshooting concerning the laser. 2. Nurses should be responsible to ensure that laser safety standards are carried out (e.g., traffic control, safety goggle usage, ventilation, etc.). 3. Laser nurses should not be the primary circulating nurse for the procedure, but should physically stay in close proximity to the laser during use. 4. Laser nurses should evaluate the function and carry out pre-op tests prior to each procedure. 52 Operational Procedures 5. The laser nurse should keep the laser in stand-by mode while not in operation. Policy/Category: Credentials and Orientation for Laser Technicians* Approval • All institutional laser technicians must be approved by the Laser Committee Requirements for approval 1. Attendance at Laser Training Course offered for clinical use of medical lasers. Course should include: Refer to Procedure #1 Eight hours didactic per wavelength, including basic laser physics, soft tissue interaction and safety. 2. Two hours “Hands-On” laboratory experience with a laser credentialed physician or qualified laser technician. 3. Basic knowledge of anatomy. 4. Basic knowledge of sterile technique and procedures for the Laboratory and Operating Room. Orientation • Laser technicians must be oriented to basic troubleshooting and design features of the laser systems by laser distributors or manufacturing companies. *Note: Service engineers and maintenance personnel are included in this category. 53 Operational Procedures Procedure #2 - Pre/Post-Operative Safety Checklist 1. Physician certified by hospital for wavelength laser used. Laser nurse/technician available to operate laser controls. Laser key obtained. 2. Doors to room closed. 3. Laser signs on doors. 4. Protective eyewear available. 5. Basin of saline available and location of fire extinguisher known. 6. Absences of flammable solutions or preps. 7. Wet sponges used to protect surrounding tissue where indicated. Patient’s eyes protected. 8. Specially designed instrumentation available (non-reflective metals, titanium, rhodium or quartz) where indicated. 9. When performing airway surgery, appropriate endotracheal tubes used, if indicated, and O2 concentration maintained at 30-40%, or lower. 10. When working around the anus, if bowel prep has not been done, rectum packed with wet sponge. 11. Smoke evacuator used as needed. 12. Maintain Laser Safety Log. 13. When laser not in use, put in “STANDBY MODE.” If laser is to be left unattended, it must be turned off. 14. The laser beam shall NEVER be directed at personnel. 54 Operational Procedures Procedure #3 - Practical “Rules of Thumb” for Laser Safety Some good procedures to follow in the use of surgical lasers are: 1. Draping the immediate area of the surgical incision with wet towels (i.e., sterile solution) rather than dry towels to avoid towel combustion. 2. In determining proper beam focus, exposure time, and power level, never aim laser at a target without an absorptive backstop. 3. Be aware that there can be a difference between the power output indicated on the laser system meter and power delivered into the tissues. 4. The use of focusing guides, which not only assist the surgeon in keeping the focal spot on the tissue but also reduce the chance of hazardous specular reflection. In this regard, one of the best safety design strategies is the use of a short-focal length lens in the beam delivery system. 5. Exclusion of combustible anesthetic gases from laser surgical procedures. 6. Be very careful of moving or hitting the laser. It is a very sensitive system and easy to misalign optical components. To avoid disturbing the alignment, one could have all laser surgical units “dedicated” to a given operating room. 7. A positive action switch, either a hand trigger squeeze switch or fool switch, to ensure rapid shut-off in case of emergency. 8. Prohibition of misuse by unauthorized personnel with a key switch. (Such a key switch master control is required by CDRH federal laser standard.) 55 Operational Procedures 9. Develop and distribute Standard Operating Procedures (SOP) for use with lasers. 10. Keep records of laser type, serial number, wavelength, output power, beam diameter, divergency, and all inspection dates in one central permanent place. 11. The beam exit port should be located and clearly marked. 12. All connectors of fiber optics cables to laser output must be designed to terminate laser emission when the cable is removed. 13. The use of fiber optics light guide with a high numerical aperture will produce a rapidly diverging beam and, therefore, reduce the distance (range) wherein a hazardous exposure may occur. 14. Quite often, surgeons have available a fire-resistant target such as alumina or silicon-carbide firebrick to focus a hand-held laser “scalpel.” This target assists in developing a “feel” for the equipment and gives a visible adjustment of the beam’s focal spot. Metallic surfaces are unacceptable for this purpose. 15. All operating room personnel and any other observers must wear appropriate eye protection for the type of laser being used. 16. Be aware that once the beam is on, it continues to be absorbed by matter. Whenever the laser beam is “on” it can do damage to other tissues. The surgeon must always aim the beam at a safe fire resistant target when not in use. 17. Highly reflective surgical instruments are not recommended. 56 Operational Procedures 18. In order to minimize the observers in the surgical room, it is highly recommended that signs such as “Laser Surgery In Progress” and a danger sign be affixed to the outside of the door leading into the operating room. 57 Operational Procedures Procedure #4 - Non-Beam Hazards Purpose • To recognize and effectively deal with a variety of potential non-beam hazards which may be present during laser procedures. Policy • Non-beam hazards are the purview of safety and industrial hygiene personnel, who will effect the appropriate hazard evaluation and control. Procedure • Fire 1. Never use alcohol in the operative field. Fibers may be rinsed in hydrogen peroxide or saline intraoperatively. 2. Never place a hot fiber directly on paper drapes. Wait until tip is cool before contact is made with flammable material. 3. Use fire-retardant drapes, damp packs or pads. Fill pelvic cavity with Ringer’s saline or other appropriate solution during surgery. 4. Put laser system in standby mode when procedure is interrupted or terminated. 5. Avoid high levels of oxygen in the operative field. 6. Avoid laser beam exposure of the sheaths of flexible fiber endoscopes, since many of the sheaths are flammable. 58 Operational Procedures • Plume Management 1. Remove laser-generated airborne contaminants from the energy impact site to reduce the transmission of potentially hazardous particulates. 2. Position smoke evacuator in the operating room whenever plume is anticipated. 3. Check operation of the plume management system prior to the beginning of the case. 4. Check the plume filter monitor, and if needed, install a clean filter. 5. In-line filters, with minimum 0.3 µm filtration, will be placed between wall suction and the fluid canister for: a. Suction line not connected to evacuator. b. Cases producing minimal plume. c. Failure of evacuator before or during operation. 6. Distal collection port must be no more than 2 cm from impact site, when practical. 7. All tubing, connectors, adapters, and wands will be changed per case, and disposed of according to biohazard procedures. • Electrical Shock 1. During Service or maintenance, precautions must be taken against electrical shock, which may be fatal. 2. HCLS lasers shall be installed and operated in conformity with the National Electrical Code. 59 Operational Procedures Procedure #5 - Laser Safety Education Program The Laser • Physics and biological effects • Components of the laser system, delivery devices and instrumentation • Overview of clinical applications Administrative Controls • Laser Committee • Role of the LSO • Development of policies/procedures • Documentation methods • Regulations, standards, and recommended professional practices • Certification criteria and skills validation • Medical Surveillance Perioperative Safety • Controlled access • Eye protection • Reflection hazards • Flammability hazards and draping 60 Operational Procedures • Electrical safety • Management of plume • Management of anesthesia in airway surgery • Equipment testing, aligning and troubleshooting 61 XII. Bibliography ACMP Report VI. “Radiation Control and QA of Medical Laser Systems.” American College of Medical Physics, 11250 Roger Bacon Drive, Reston, VA 20190-4390 (1991). ANSI Z136.1, “Safe Use of Lasers.” American National Standards Institute, Inc., 1430 Broadway, New York, NY 10018 (2000). ANSI Z136.3, “Safe Use of Lasers in Health Care Facilities.” American National Standards Institute, Inc., 1430 Broadway, New York, NY 10018 (1996). Control of Laser Radiation, 105 CMR 121.00. Commonwealth of Massachusetts, Boston, Massachusetts (1997). “Guide for Control of Laser Hazards.” American Conference of Government Industrial Hygienists, 1330 Kemper Meadow Drive, Cincinnati, OH 45240 (1981). Laser Safety Guides and Reference Materials, Laser Institute of America, 12424 Research Parkway, Suite 125, Orlando, FL, 32826. Laser Safety Training Programs and Videos, Rockwell Laser Industries, P.O. Box 43010, 7754 Camargo Road, Cincinnati, OH 45443. Medical Devices Act, Code of Federal Regulations, Title 21, Part 1040. Washington, DC. 63