Applying visual models for priority setting CAMHS EBPU UCL & Anna Freud Centre
advertisement

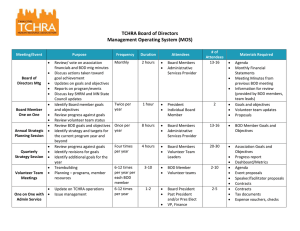
Applying visual models for priority setting CAMHS EBPU UCL & Anna Freud Centre 7 July 2013 Gwyn Bevan Department of Management SyMPOSE Systems Modelling for Performance Optimisation & Service Equity Mara Airoldi Gilberto Montibeller Alec Morton Chiara de Poli Samantha Roberts Laura Schang Jenifer Smith http://www2.lse.ac.uk/management/research/initiatives/sympose/home.aspx Applying visual models for priority setting Cost-effectiveness analysis (CEA) & Burden of Disease (BoD) Cost-effective impact on BOD? Making horse & rabbit stew taste good Visual model from early Research into Operations Visual model from early Research into Operations Merchantmen F(area) Defence F(perimeter) Lord Blackett Head of Physics Department of Imperial College (1953 -63) Nobel Prize in Physics 1948 ‘most versatile & best loved physicist of his generation’ Value for Money (VfM) Triangles Value Population benefit Benefit / person Numbers who benefit costs Prioritisation by marginal analysis: biggest bang / buck QALYs A B C Order by slope of line VfM = QALY/cost 1. A 2. B 3. C 4. D D Costs A theory of priority setting against budget constraint? QALYs E D C A B Size of triangle matters Budget constraint DA Costs Cost-effectiveness analysis (CEA) & Burden of Disease (BoD) CEA Health gain in Quality-Adjusted Life Years (QALYs) Set priorities in terms of cost / QALY Ignores scale & transaction costs of making changes BoD Years of life lost (YLLs) Years lived with a Disability (YLDs) Ignores what is ‘avoidable’ & costs Does reduction of BoD in DALYs = health gain in QALYs? ΔQALYs QoL 1 .8 30*.5 = 15 .5 QALYs gained QoL 0.8 drops dead age 35 Intervention 30 years QoL 0.5 0 35 65 age ΔDALYs 30*.5 = 15 DALYs avoided QoL 1 .8 BoD .5 QoL 0.8 drops dead age 35 Intervention 30 years QoL 0.5 0 35 65 85 age DALY methods of estimation Current BoD? Fixed reference age (e.g. 85) arbitrary no benefit treating over 85s YLLs from life tables better ΔDALYs? Life tables bizarre results ΔDALYs not ΔQALYs Fixed reference age ΔDALYs = ΔQALYs Visual Models of Health Gain Average DALY / QALY loss per person Observed BoD Average QALY gain per person Population Avoidable BoD benefit Numbers (‘000s ) Applying visual models for priority setting Burden of Disease (BoD) & Costeffectiveness analysis (CEA) Cost-effective impact on BOD? Making horse & rabbit stew taste good Cost-effective & BoD? stroke treatment Massive annual BoD deaths + disability = 0.5m QALYs lost ‘must dos’ (highly cost-effective) Stroke Unit: 54% 100% Thrombolysis: 9% < 3 hours onset Achieve ‘must dos’: BoD from stroke? Cost-effective & BoD? Average QALY loss/person QALYs Costeffective Costs BoD? Numbers Impact on BoD from stroke (England) 5 Average QALY*/ person 4 3 2 1 Stroke units (6%) 10 Thrombolysis (0.4%) 50 Numbers (‘000s ) 110 Treatment & prevention of stroke in Isle of Wight Stroke unit 50% 100% Thrombolysis 9% patients < 3 hours stroke onset Prescribed first-line antihypertensive BP(55)> 55 years BP(140/90): blood pressure > 140/90 Na2 sodium content in bread & cereals Impact on BoD from stroke (IoW) Mean QALY gain 'Avoidable' DALYs 4.00 Na2 3.50 3.00 BP (55) BP(140/90) 2.50 Stroke units 2.00 1.50 1.00 0.50 0 10 20 Thrombolysis 30 40 50 60 70 80 Numbers Applying visual models for priority setting Burden of Disease (BoD) & Costeffectiveness analysis (CEA) Cost-effective impact on BOD? Making horse & rabbit stew taste good Horse & rabbit stew: take one horse & one rabbit Sheffield PCT: eating disorders Two one day meetings 20 participants Data-pack each service: Benefits How many? How much? Inequalities? Costs? PCT managers Providers managers Patients and carers Public rep Clinicians Assessing QoL for mild eating disorders around anchors Benefit / person (QoL): intensive residential care Stay Worsen same (QoL = (QoL = 0.05) 0.1) Little improve ment (QoL = 0.12) Become Recover moderate Average (QoL = (QoL = QoL 1) 0.5) After 1 year, if admitted 0% 25% 0% 33% 42% 0.61 After 1 year, if not admitted 10% 30% 50% 10% 0% 0.15 Benefit = 0.46 Quality-Adjusted Life Years (QALYs) / person Intensive residential care Value Population benefit = 7.36 Benefit / person = 0.46 Numbers who benefit = 16 costs Good or poor VfM? Population health gain Poor VfM Good VfM -ve VfM Costs VfM triangles pathway for treatment of eating disorders Value ? Residential intensive care 80% costs & 13% benefits Costs VfM for eating disorders Lower budget More benefit Star tool – launched May 2013 To download: http://www.health.org.uk/areas-of-work/star/ Applying visual models for priority setting Thank you!