National Heart Failure Audit Steering Group meeting minutes 23 January 2014, 13.30-15.30
advertisement

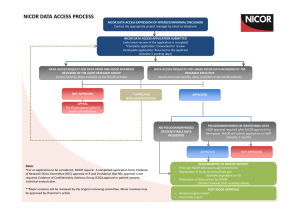
National Heart Failure Audit Steering Group meeting minutes 23 January 2014, 13.30-15.30 rd Boardroom, 3 floor 170 Tottenham Court Road, London W1T 7HA 1. Apologies and introductions 1.1 Present: Jackie Austin, Gemma Baldock-Apps, Janine Beezer, Dawn Lambert, Theresa McDonagh (chair), Polly Mitchell, Richard Mindham, Jim Moore, Julie Sanders, Kathy Simmonds. 1.2 In attendance: Morag Cunningham 1.3 Apologies: John Cleland, Gethin Ellis, Suzanna Hardman TM welcomed everyone to the first meeting of the Steering Group. MC, project coordinator of the CRM audit, was introduced to the group. She is in attendance as part of a NICOR scheme to share good practice and knowledge across audits. PM noted that HQIP no longer wishes to be represented at individual project level, and will henceforth attend NICOR-level meetings only. 2. NICOR update JS requested that a NICOR update is a standing item on Steering Group agendas. The UCL review has now been completed, and the final report will be discussed at the Professional Liaison Group prior to circulation. JS indicated that there is no cause for concern, and it highlighted issues that are already being addressed within NICOR. HQIP funding for the audits has been extended for two years. Currently each audit clinical lead and project manager, with others at NICOR, are going through the deliverables to amend and update them. Several new staff will be recruited at NICOR once the deliverables have been agreed for the contract extension: an audit and research manager to oversee all of the audit projects, a data manger to manage data extracts and cleaning – which will hopefully free up more analyst and developer time – and another analyst. The minimum data standard will be implemented from 2014/15 – this is to be discussed later in the meeting (item 5). NICOR will implement a policy for the detection and management of outliers in 2014/15, which will be broadly derived from the HQIP/Department of Health outlier policy. Confirmed that this would include data quality measures as well as clinical and outcome measures. Tm added that the audit will not publish hospital level mortality figures until an adequate risk model has been developed – the proposed timeline for this is October 2015. The HF risk model will not necessarily be adopted into NICE clinical standards – NICE will have to make this decision. However sharing hospital-level outcomes analysis publically may influence change anyway. NICOR has submitted an application for a PhD studentship, funded by industry/UCL. There is also an on-going project linking the diabetes audit data with NICOR audit data, to look at CVD outcomes in diabetics. John Deanfield (director of NICOR) has a five year programme grant from the BHF. NICOR will hold a PPE event on 8 May, with an aim to increase patient involvement in NICOR. Hope to get a better understanding of what information the public and patients want from NICOR, and how they want to access this information. NICOR’s PPE coordinator, Carol Porteous (c.porteous@ucl.ac.uk) is advertising for patients to attend, and has an advert in Heart Matters, the BHF magazine for cardiac patients, which goes out to around 300,000 people, and will also be advertised on the NICOR website. The event is aimed at patients, carers, relatives and interested lay people. TM noted the new structure of NICOR, and JS distributed a diagram of the NICOR governance structure. She explained that the audit originally grew out of the BSH, and 3. was adopted by the Information Centre and thus became a part of CCAD, which housed all of the cardiac audits. This moved into NICOR in 2011, and gave the opportunity for linkage of the existing datasets (MINAP, CRM, etc.). After the Leeds-related premature data release last year, NICOR has changed its governance structure. The audit steering group now feeds up into the Professional Liaison Group, chaired by Iain Simpson, on which TM and SH sit. The National Heart Failure Audit now has an Executive Group (strategic), a Steering Group (stakeholder engagement and audit development) and HALO (research and data sharing). NICOR will soon have an advisory board, the composition of which is still to be decided. This will allow the Professional Liaison Group to escalate issues above the NICOR Executive. Minutes of the last meeting and matters arising The minutes were accepted as an accurate record of the meeting. 2.2a: PM confirmed that NICOR can now release dates of death to hospitals. There are a number of different ways of doing this: i. Exports from the database to contain date/fact of death at a patient level (this means that hospitals can use this information in their own analysis and local-level research). ii. Online analysis giving crude in-hospital, 30-day and 1-year mortality for each hospital – appended to existing online reports. iii. Quarterly reports which give mortality figures for a three-month period. A number of points were raised, including: Potential data protection issues with including mortality data in every extract. It was suggested that there should be an option to include mortality data which has to be selected at point of export. PM noted that the PCI audit had a good export function which allows you to add elements to your extract in a modular way. JA suggested the reports (in whatever format) come with some caveats. Agreed that it needed to be clear that this was crude mortality. KS noted that her Trust (and others) were often a couple of months in arrears in terms of data collection, due to a need to pull noted. Explained that online analysis would run on all data in the system, so if there was no data for the last two months it would only cover the months for which there were records in the database. Action 1: PM to speak to Marion Standing about preparing examples of the three suggested ways of displaying mortality data, to be distributed around the steering group prior to the next meeting. 4. Steering Group Terms of Reference and membership The draft Terms of Reference document was reviewed and a few comments were made: ‘Stakeholder’ should be explicitly defined as encompassing clinicians, heart failure nurses and pharmacists, clinical audit staff, patients, NICOR staff. Not to include CCGs, clinical networks. NHS England etc., although representatives thereof can be invited if relevant to discussion. PM noted that RM had sent a series of comments by email, and many of his suggested changes would be made. TM asked whether the group needed someone with a specific remit for palliative care. KS noted that she had palliative care training as part of HFNS training. DL asked what it meant to say that the meetings were “not confidential”. PM confirmed that minutes were expected to be published online. It was agreed that a clause should be added to state that the Chair could censor information in published minutes in exceptional circumstances, for example where a particular hospital was being discussed as an outlier. It should always be stated in the published minutes where information had been censored and for what reason. 5. Minimum data standard update PM explained the NICOR requirement for a minimum data standard, which, in the future, will require submitted data to reach a certain level of data completeness and case ascertainment for hospital level data to be published in annual reports. The Project Board had previously decided to focus on completeness of individual records (e.g. each record having no missing or unknown values), which would allow more records to be included in risk models. This would ensure that the risk models being developed over the next year are as accurate as possible. Last year, of all relevant records for inclusion in the 1 year regression models (first admissions, survived to discharge) 40% were included in the model. On the basis of this it was agreed that the minimum data standard, to be implemented in 2014, should expect complete mandatory data – with no ‘unknown’ values – for 70% of all records submitted to the audit. Microsoft Word 97-2003 Document NHFA minimum data standard I was noted that it is not expected for hospitals to collect the non-core dataset, though this can be used for ‘deep dive’ audits, or local audit projects. 6. Annual report 2013/14 TM noted that the Executive Group had discussed the broad analysis plan for the 2013/14 annual report and had made a few initial suggestions: Descriptive analysis of demographics and prescribing rates/referral rates to remain similar to existing model, but to also include five year trends in prescribing rates. No increase in hospital level reporting apart from data quality information Aggregate mortality analysis section to be significantly reduced: o All cause in-hospital mortality o All cause 1-year mortality o Five year mortality trends Aggregate LOS and readmission analysis No mortality or readmission at hospital level or clinician level It was suggested that the clinical lead for each hospital could be names in association with case ascertainment/data quality information, as long as it was clear that this person was not necessarily responsible for the care of all heart failure patients in the hospital. Action 2: Annual report analysis plan to be developed and circulated prior to next Steering Group meeting. 7. Web development and dataset implementation The web-based version of the audit application has now been developed and is in the process of being rolled out. Marion Standing has started work on the dataset revision, which will be rolled out in April. All development work is going to plan. 8. Primary care linkage update JM and PM have continued to discuss the proposed linkage of NHFA data to primary care data in Gloucestershire. The aim is to link National Heart Failure Audit data from the Gloucestershire Hospitals Trust to data collected by the community-based heart failure service in Gloucestershire, which has conducted an extensive audit over the past few years. This will be used as a stepping stone to linking to regional primary care data in Gloucestershire more generally – using the HF linkage as a proof of concept. Once problem that has been identified is a lack of primary care data in the audit from the two secondary care sites in Gloucestershire. JM has spoken to the cardiologists in the Trust, who are engaging a SpR to take the lead on this project and ensure that adequate data is uploaded to the audit. JM has also spoken to the Gloucestershire CCG about using QOF data for the second stage of the linkage, and it seems that this will be possible. JM has a meeting set up to discuss the information governance implications of this project. Next step is to decide what analysis will be completed, so that a data sharing application can be submitted to HALO. Suggested that JC is involved in this. Action 3: PM to organise meeting with JM and relevant people in Gloucestershire secondary and primary care services to discuss primary care linkage analysis. 9. Research update TM gave an update from HALO on the research activity of the audit: Two papers based on 2012/13 audit analysis – one led by JC looking at three year trends, and once led by TM addressing the benefit of specialist care when severity of disease and other confounding factors have been adjusted for. A project from the George Centre in Oxford, led by Kazem Rahimi, which addresses how much of the variation in care between hospitals is attributable to aspects of the hospital organisation itself as opposed to patients and the treatment they receive. Propensity analysis with Ian Ford as analyst, which will examine the effects of specialist care, whilst trying to eliminate all possible confounding factors by matching patients based on their relevant clinical and demographic characteristics. Analysis for Novartis relating to their serelaxin trials was completed by Aminat at the end of 2013. TM has written an abstract relating to this analysis for the ESC HFA meeting. Hoped that the research fellows at King’s and Hull who collected the data will produce a research paper each relating to the data. MAPP-HF project is on-going – aim of this project is to firstly look at the definition and prevalence of heart failure across an existing linked dataset of CPRD (primary care), MINAP (myocardial infarction), ONS (mortality) and HES (hospital admissions). Following this, it would investigate heart failure in a linked dataset as above, plus all of the other NICOR audits. The project aims to track the patient journey across primary and secondary care, and to look at missed opportunities for prevention in primary care. A PhD student and a post-doctoral fellow have been identified to carry out the analysis for this project. ESC guideline tool for patient management, which would be a module attached to the audit, notifying the person entering data of the best clinical management for the patient in question, based on details entered. The ESC want to pilot a tool in several sites across Europe. JB noted that in Sunderland they use a clinical audit tool called Zynx, developed in the US, which prompts the next step of treatment. 10. AOB New prospective methodology: PM explained that a series of pilot sites were needed to test a new, prospective methodology, wherein patients were identified by their symptoms and signs of HF on admission, and results of diagnostic tests. Pilot will run in the second quarter of the 2014/15 audit year (i.e. July-September). KS, DL, GBA and JB all expressed interest in participating, and said they would discuss with their clinical leads. KS noted an increase in the number of patients coded with heart failure over the last year. TM confirmed that this rise had been seen nationally. Action 4: PM to organise meeting to discuss new methodology and determine inclusion criteria. Dates and times of next meetings: • Thursday 3 April, 13.00-15.00 • Thursday 3 July, 13.00-15.00 Action Points # 1 Action PM to speak to Marion Standing about preparing examples of the three suggested way of displaying mortality data, to be distributed around the steering group prior to the next meeting. Annual report analysis plan to be developed and circulated prior to next Steering Group meeting. Owner PM, MS 3 PM to organise meeting to discuss primary care linkage analysis. PM 4 PM to organise meeting to discuss new methodology and determine inclusion criteria. PM 2 PM, TM Completed?