Palliative Care in Dementia: A European Nathan Davies , Steve Iliffe
p264
Palliative Care in Dementia: A European
View of the Models of Palliative Care
Nathan Davies
1
, Steve Iliffe
1
, Jill Manthorpe
2
and Sam Ahmedzai
3
1
UCL, Research Department of Primary Care and Population Health, Royal Free Campus, Rowland Hill St., London,
NW3 2PF
2
Social Care Workforce Research Unit, King's College London, Aldwych, London, UK
3
Department of Oncology, The Medical School, Beech Hill Road, Sheffield
Background
With an ageing population, people living with dementia is expected to continually rise to 81 million affected by
2040 1 and 115 million worldwide by 2050 2 . Generally, as the disease progresses, memory and other cognitive deficits become worse, together with a loss in mobility, self-care abilities, poor nutrition, and a breakdown of skin. In the final stages, it is common to have urinary tract infections, skin ulcers, pneumonia and many other complications. As a progressive and eventually fatal illness, a palliative care approach for dementia is generally accepted as the best option.
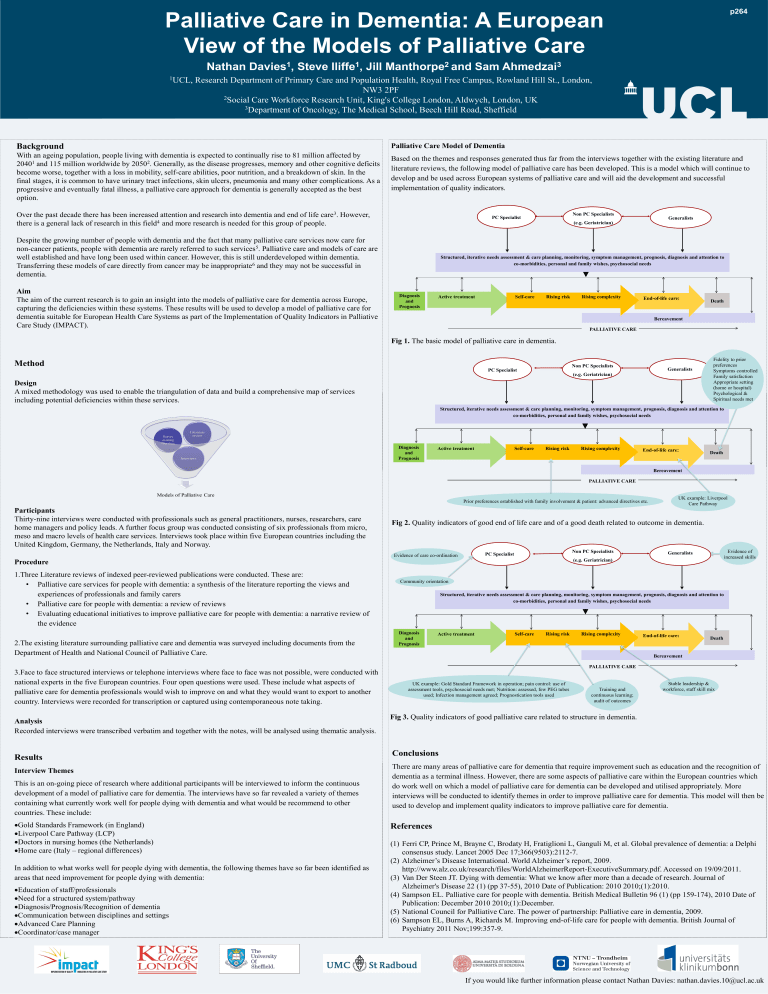
Palliative Care Model of Dementia
Based on the themes and responses generated thus far from the interviews together with the existing literature and literature reviews, the following model of palliative care has been developed. This is a model which will continue to develop and be used across European systems of palliative care and will aid the development and successful implementation of quality indicators.
Over the past decade there has been increased attention and research into dementia and end of life care 3 . However, there is a general lack of research in this field 4 and more research is needed for this group of people.
PC Specialist
Non PC Specialists
(e.g. Geriatrician)
Generalists
Despite the growing number of people with dementia and the fact that many palliative care services now care for non-cancer patients, people with dementia are rarely referred to such services 5 . Palliative care and models of care are well established and have long been used within cancer. However, this is still underdeveloped within dementia.
Transferring these models of care directly from cancer may be inappropriate 6 and they may not be successful in dementia.
Aim
The aim of the current research is to gain an insight into the models of palliative care for dementia across Europe, capturing the deficiencies within these systems. These results will be used to develop a model of palliative care for dementia suitable for European Health Care Systems as part of the Implementation of Quality Indicators in Palliative
Care Study (IMPACT).
Diagnosis and
Prognosis
Structured, iterative needs assessment & care planning, monitoring, symptom management, prognosis, diagnosis and attention to co-morbidities, personal and family wishes, psychosocial needs
Active treatment Self-care Rising risk Rising complexity
PALLIATIVE CARE
End-of-life care:
Bereavement
Death
Fig 1.
The basic model of palliative care in dementia.
Method
Design
A mixed methodology was used to enable the triangulation of data and build a comprehensive map of services including potential deficiencies within these services.
PC Specialist
Non PC Specialists
(e.g. Geriatrician)
Generalists
Fidelity to prior preferences
Symptoms controlled
Family satisfaction
Appropriate setting
(home or hospital)
Psychological &
Spiritual needs met
Structured, iterative needs assessment & care planning, monitoring, symptom management, prognosis, diagnosis and attention to co-morbidities, personal and family wishes, psychosocial needs
Diagnosis and
Prognosis
Active treatment Self-care Rising risk Rising complexity
End-of-life care:
Death
Bereavement
PALLIATIVE CARE
Prior preferences established with family involvement & patient: advanced directives etc.
UK example: Liverpool
Care Pathway
Participants
Thirty-nine interviews were conducted with professionals such as general practitioners, nurses, researchers, care home managers and policy leads. A further focus group was conducted consisting of six professionals from micro, meso and macro levels of health care services. Interviews took place within five European countries including the
United Kingdom, Germany, the Netherlands, Italy and Norway.
Fig 2.
Quality indicators of good end of life care and of a good death related to outcome in dementia.
Procedure
1.Three Literature reviews of indexed peer-reviewed publications were conducted. These are:
•
Palliative care services for people with dementia: a synthesis of the literature reporting the views and experiences of professionals and family carers
•
Palliative care for people with dementia: a review of reviews
•
Evaluating educational initiatives to improve palliative care for people with dementia: a narrative review of the evidence
Evidence of care co-ordination
PC Specialist
Non PC Specialists
(e.g. Geriatrician)
Generalists
Community orientation
Structured, iterative needs assessment & care planning, monitoring, symptom management, prognosis, diagnosis and attention to co-morbidities, personal and family wishes, psychosocial needs
2.The existing literature surrounding palliative care and dementia was surveyed including documents from the
Department of Health and National Council of Palliative Care.
Diagnosis and
Prognosis
Active treatment Self-care Rising risk Rising complexity
PALLIATIVE CARE
3.Face to face structured interviews or telephone interviews where face to face was not possible, were conducted with national experts in the five European countries. Four open questions were used. These include what aspects of palliative care for dementia professionals would wish to improve on and what they would want to export to another country. Interviews were recorded for transcription or captured using contemporaneous note taking.
UK example: Gold Standard Framework in operation; pain control: use of assessment tools, psychosocial needs met; Nutrition: assessed, few PEG tubes used; Infection management agreed; Prognostication tools used
Training and continuous learning; audit of outcomes
Fig 3.
Quality indicators of good palliative care related to structure in dementia.
Analysis
Recorded interviews were transcribed verbatim and together with the notes, will be analysed using thematic analysis.
End-of-life care:
Bereavement
Death
Stable leadership & workforce, staff skill mix
Evidence of increased skills
Results
Interview Themes
This is an on-going piece of research where additional participants will be interviewed to inform the continuous development of a model of palliative care for dementia. The interviews have so far revealed a variety of themes containing what currently work well for people dying with dementia and what would be recommend to other countries. These include:
Gold Standards Framework (in England)
Liverpool Care Pathway (LCP)
Doctors in nursing homes (the Netherlands)
Home care (Italy – regional differences)
In addition to what works well for people dying with dementia, the following themes have so far been identified as areas that need improvement for people dying with dementia:
Education of staff/professionals
Need for a structured system/pathway
Diagnosis/Prognosis/Recognition of dementia
Communication between disciplines and settings
Advanced Care Planning
Coordinator/case manager
Conclusions
There are many areas of palliative care for dementia that require improvement such as education and the recognition of dementia as a terminal illness. However, there are some aspects of palliative care within the European countries which do work well on which a model of palliative care for dementia can be developed and utilised appropriately. More interviews will be conducted to identify themes in order to improve palliative care for dementia. This model will then be used to develop and implement quality indicators to improve palliative care for dementia.
References
(1) Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet 2005 Dec 17;366(9503):2112-7.
(2) Alzheimer’s Disease International. World Alzheimer’s report, 2009. http://www.alz.co.uk/research/files/WorldAlzheimerReport-ExecutiveSummary.pdf. Accessed on 19/09/2011.
(3) Van Der Steen JT. Dying with dementia: What we know after more than a decade of research. Journal of
Alzheimer's Disease 22 (1) (pp 37-55), 2010 Date of Publication: 2010 2010;(1):2010.
(4) Sampson EL. Palliative care for people with dementia. British Medical Bulletin 96 (1) (pp 159-174), 2010 Date of
Publication: December 2010 2010;(1):December.
(5) National Council for Palliative Care. The power of partnership: Palliative care in dementia, 2009.
(6) Sampson EL, Burns A, Richards M. Improving end-of-life care for people with dementia. British Journal of
Psychiatry 2011 Nov;199:357-9.