Caroline Wolverson York St John University |
advertisement
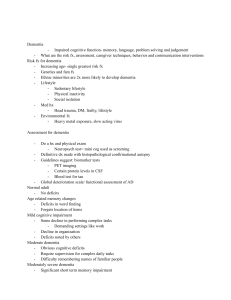
Caroline Wolverson York St John University | www.yorksj.ac.uk Setting the Scene: Health & Social Care services for older people in England York St John University | www.yorksj.ac.uk Health & Social care in England • National Health Service – free access to health care at point of delivery: this means everyone can register with a General Practitioner to access a primary health care service • Social care: People entitles to assessment of need & provision of services • Recent change in Government wanting to introduce competition & commercialism which some would say is at the expense of collaboration • More pressure on staff to demonstrate improved outcomes with less funding Previously Health 3rd sector – private & voluntary organisations Social services Changing to Health 3rd sector Social services Older People’s services in the UK • In 2008 the number of people over 65 was greater than those under 16 in the UK for the first time ever • People over 65 make up 16% of the population but account for 43% of the total National Health Service budget & take up 65% of acute hospital beds Services dictated by Government Policy for example: • National guidelines delivered at local level • National Service Framework for Older People (2001) • National Dementia Strategy (2009) • National Institute for Clinical Excellence(2006) Dementia Guidelines • No Health Without Mental Health (2011) The Focus of the Rhetoric • Choice • Personalisation: personal health & social care budgets • Partnership working • Improving public health: prevention of ill health & Health Promotion • Independence, wellbeing & quality of life & active ageing • Person-centred care • Early diagnosis for people with dementia • Reablement services The reality for older people • There are some excellent services which have been implemented over the last 10 years • However, older people are still marginalised & experience discrimination (frequent reports particularly on standard of nursing & residential home care) • Lack of co-ordination between services & pressure as to which agency funds services – is it a health or social care need? • Government concept of ‘The Big Society’ Occupational therapy with older people • Often not specific older people’s services – particularly in physical health settings • Challenge of implementing ‘Best Practice’ within service constraints • Recognition of multi-disciplinary approach - Few services consist only of OT’s • More skills sharing amongst different professions, for examples, OT’s monitoring blood pressure, physios & nurses providing basic equipment • Increase in generic working, particularly in mental health services Key Roles • Assessment of need in relation to occupational performance • Provision of services to assist in maintaining daily routines, maintaining & good health (NICE 2008) • Reablement & rehabilitation • Education/ training of care staff (COT/ NAPA (2007)‘Activity provision: benchmarking good practice in care homes’) • Education of carers • Maintaining quality of life & wellbeing: promoting an active lifestyle (Public Health Agenda) • Maintaining opportunity for choice & decision making • Prevention of admission to hospital or reducing hospital stay (intermediate care services) • Supporting independent living (Independent Living agenda 2010) • Building the evidence base to support non-pharmacological interventions to support people with dementia • Falls prevention programme