Communicating About Autism Decreasing Fears and Stresses Through Parent-Professional Partnerships
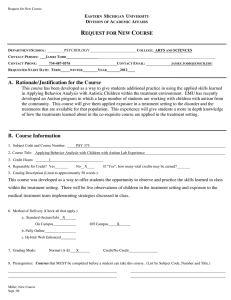
advertisement

Infants & Young Children Vol. 21, No. 4, pp. 256–271 c 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins Copyright Communicating About Autism Decreasing Fears and Stresses Through Parent-Professional Partnerships Larry A. Gray, MA; Emily R. Msall, MA; Michael E. Msall, MD There is increasing public and healthcare provider awareness about the early signs and developmental challenges of children with autistic spectrum disorders (ASDs). Healthcare professionals are guided by several major policy statements regarding the diagnosis and management of autism. There remain substantial gaps between these guidelines and families’ needs during the diagnostic process. This article provides a developmental and behavioral perspective for the professionals who desire to find guideposts in task of supporting families throughout the diagnostic process of autism. We illustrate the diversity of the ASDs using the International Classification of Functioning, Disability and Health Model and describe developmental and behavioral perspectives about the autism diagnostic process. Our overall goal is to enhance parent and professional collaboration in promoting the establishment of medical homes, accessing the highest quality developmental assessments, and implementing comprehensive supports for parents of children with ASDs. Key words: autistic spectrum disorders, counseling, family supports, functioning T HERE is increasing awareness about the early signs and developmental challenges of children with autistic spectrum disorders (ASDs) (Chakrabarti & Fombonne, 2001; Fombonne & Chakrabarti, 2001). Major pol- Author Affiliations: Sections of Developmental & Behavioral Pediatrics and Community Health Sciences, University of Chicago Comer Children’s Hospital, Chicago, Illinois (Dr Gray and Ms Msall); and Institute of Molecular Pediatrics and Kennedy Center on Mental Retardation and the LaRabida Children’s Hospital, Chicago, Illinois (Dr Msall). The authors acknowledge Dr Peter Smith, Melissa Gray, CPNP, and the University of Chicago Early Intervention Team who provided feedback and a creative team approach to advocating for quality care pathways and family supports. This article is dedicated to Charley Blondis who taught all of us the value of being an optimal family member of a sister with genetic and autistic spectrum challenges. His untimely death highlighted the gaps between a culture of violence and a community of caring. Corresponding Author: Larry A. Gray, MD, Section of Developmental & Behavioral Pediatrics, University of Chicago Comer Children’s Hospital, 950E 61st St, SSC Room 227, Chicago, IL 60637 (lag@uchicago.edu). 256 icy statements by the American Academy of Pediatrics and the National Academy of Sciences have provided a template for widely disseminated state-of-the-art strategies for diagnosis and management (Committee on Children With Disabilities, 2001a; National Research Council Committee on Educational Interventions for Children With Autism, 2001). However, there remain substantial gaps between these guidelines and families’ goals of feeling supported and accessing quality and comprehensive early childhood services (Anders & Gardner, 2003; Renty & Roeyers, 2006). The purpose of this article is to provide developmental and behavioral pediatric perspectives for healthcare professionals on ASDs with respect to communicating the developmental diagnosis, explaining medical advances to families, and providing ongoing family supports. We build on the International Classification of Functioning, Disability and Health (ICF) framework of enablement, functional assessment, and child and family wellbeing (World Health Organization, 2001). In approaching the developmental diagnosis of Communicating About Autism autism, we strive to begin a dialogue about the process of developmental diagnosis in the setting of a child’s strengths and challenges while addressing the complex hopes, fears, stressors, and typical lack of family supports. In addition, we discuss some of the strengths of a developmental diagnostic approach that emphasizes a spectrum of outcomes and possibilities as well as some of the pitfalls of a categorical diagnosis, particularly when families in desperation try complementary interventions that may have adverse effects. Our goal is not to review the complexity of accepted and/or alternative treatments, as this has been recently done by the National Academy of Sciences (National Research Council Committee on Educational Interventions for Children With Autism, 2001) and Hyman and Levy (2005), but to highlight how the primary care provider positively impacts the diagnostic process and how ongoing family supports can be provided as families negotiate the complexity of management in the birth-to-3 and early preschool years. In this way, we begin to develop both problemsolving strategies and approaches essential to optimizing health, development, and functional competencies. ADVANCES IN PEDIATRICS AND DEVELOPMENTAL MEDICINE Major advances in pediatrics, child development, and developmental neurosciences have enhanced our understanding of children with autism (Bristol, McIlvane, & Alexander, 1998). These advances have included the prevention of neurodevelopmental sequelae in children with phenylketonuria (PKU). PKU is an inborn error of metabolism whereby children fed milk or natural proteins develop autism and developmental disabilities. Through specialized nutritional interventions, requiring both metabolic formulas and biochemical monitoring, children are severely restricted in their natural protein intake. Children with PKU cannot drink cow or soy milk or eat cookies, crackers, hamburgers, ice cream, pizza, cheese, hot dogs, cold 257 cuts, or cake. The special protein formula provides the equivalent of a liver transplant and dialysis machine. In all 50 states, screening for PKU takes place in newborns whereby, after confirmatory biochemical analysis, a specialized biochemical formula is started. Major progress in immunizations has led to the near elimination of congenital rubella, measles encephalitis, and Haemophilus influenzae meningitis and resulting postinfectious developmental disabilities including ASDs (Fombonne & Chakrabarti, 2001; Goldston, Gruenberg, & Lewis, 1986; Halsey, 2001; Halsey, Hyman, & Conference Writing Panel, 2001). Prior to these vaccines, substantial numbers of children developed intellectual disability as well as neurological disorders. Neurodiagnostic advances have included the early detection of visual and hearing disorders, communicative and social developmental screening tools for evaluating parental initial concerns, and specific assessment scales for communication, play, social behaviors, and adaptive skills (Ozonoff, Rogers, & Hendren, 2003). Molecular genetic advances have included detection of fragile X syndrome, expanded banding karyotypes and FISH analysis for regional hot spots especially on chromosomes 15 and 7, and the genetic markers for the Rett syndrome and the tuberous sclerosis complex. The former is an X-linked dominant disorder whereby the MECP mutation impacts on a girl’s ability to learn purposeful hand skills and communicative skills. The latter is an autosomal dominant neurogenetic syndrome with complex seizures, difficulty learning language, and social skills, and with more than half of the children meeting criteria for ASDs. Despite these molecular advances, most children with other neurodevelopmental disorders including autism cannot be given an exact etiologic explanation. Research networks have been established by National Institutes of Child Health and Human Development and the Centers for Disease Control and Prevention to understand the epidemiology, genetic and environmental 258 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 Table 1. Stressful myths and autism Myth Reality Myth Reality Myth Reality Myth Reality Myth Reality Myth Reality Myth Reality Autism is caused by immunization of vulnerable children. Children not immunized with rubella, measles, mumps, hemophilic influenza, pneumococcal, and pertussis vaccines have high rates of developmental disabilities including deafness, blindness, cerebral palsy, epilepsy, and autistic spectrum disorders. Autism is a mental illness. Autism is a developmental disability impacting on understanding and use of language, complex learning, and social communication Autism is caused by problems during labor and delivery. Prematurity and neonatal complications have not been scientifically linked to autism. Major known etiologies associated with autism include phenylketonuria, tuberous sclerosis, congenital rubella, fragile X syndrome, chromosomal disorders, and severe retinopathy of prematurity. Children with autism cannot learn. Children with autism have strengths in motor skills, fine motor manipulative skills, nonverbal intelligence, and basic adaptive skills. There is a range of communicative, cognitive, and complex adaptive abilities. All children with autism learn. Autism is caused by poor parenting. Autism is a neurobiological disorder whereby brain systems integrating language, complex learning, and social communication are underdeveloped. Experimental alternative medical treatments involving specialized diets, megavitamins, and natural therapies can cure autism. Autism is not caused by food, allergies, or malabsorption. The best treatments for autism are special education programs that build on a child’s strengths, provide family supports, and comprehensively address communicative, learning, and behavior challenges. Children with autism with gastrointestinal concerns should receive competent pediatric care. There is no role for pediatric medicine for children with autism. All children require a medical home that monitors growth and development, identifies sensory, neurological, and health conditions that can interfere with progress, helps set comprehensive goals that optimize adaptive functioning, and advocates for proactive community programs that provide quality family supports. etiologies, and developmental processes involved in children with autism (TagerFlusberg, Joseph, & Folstein, 2001). In addition, clinical research networks of multidisciplinary professionals and specialized university-affiliated centers of excellence have developed to explore advances in psychopharmacology, communicative and developmental interventions, and alternative medicine treatments (Arnold et al., 2000; Levy & Hyman, 2002; Rogers, 1998). This systemic collaboration offers the promise for scientific advances, but has not quieted several common misconceptions that exist regarding children with autism. Table 1 provides a list of some of the most frequent myths and the evidence-based reality that defines sources of family uncertainty. There is also another major myth that there is an explosive epidemic of autism due to childhood immunizations (Nelson & Bauman, 2003; Murch et al., 2004; Offit & Jew, 2003). This leads to both suspicion of medicine and failure to understand that the preponderance of evidence supports the benefit of immunizations for the prevention of illness in children with autism and preventing both autism and severe disabilities in young children. For example, without rubella vaccine, the United States would experience Communicating About Autism epidemics of congenital rubella. Prior to this vaccine, as many as 11 000 fetal deaths and 2000 neonatal deaths occurred because of congenital rubella. In addition, more than 20 000 newborns were affected with the congenital rubella syndrome (Goldston et al., 1986). The sequelae of this syndrome include blindness in 10%, deafness in 50%, autism in 25%, as well as mental retardation, epilepsy, and cerebral palsy (Chess, 1978). Rubella vaccination prevents these epidemics. Prior to measles vaccine, significant numbers of children died from measles pneumonia and measles encephalitis. In 1923, more than 10 000 deaths were reported in 1 year because of measles. Between 1950 and 1962, almost 500 children per year died of measles (Goldston et al., 1986). In 1982, after a decade of immunization control efforts, there were 2 deaths. Approximately 1 in 1000 children with measles develops measles encephalitis and more than 50% have devastating long-term sequelae including autism (Benda, 1952). In an era where the promise of neuroscience has not yet brought new restorative treatments, immunizations are the best way to prevent both autism and other developmental disabilities. 259 ing, toileting, and bathing. In older children, these tasks include reading, preparing meals, shopping, and washing clothes. Participation means involvement in community life, such as relationships with peers, going to school, and recreational activities. The ICF model accounts for contextual factors in a child’s life, including environmental and personal factors. Environmental factors include policy, social and physical facilitators and barriers, positive and negative attitudes of others, legal protections, and discriminatory practices. Personal factors include age, gender, interests, and sense of self-efficacy. A variety of preschool scenarios using the ICF model are illustrated in Table 2 for preschool children with ASD. These scenarios include a 1-year-old girl with infantile spasms secondary to tuberous sclerosis complex, 2-yearold boy who is nonverbal with autism, a 3-year-old girl with blindness and developmental regression, and a 4-year-old boy with fragile X syndrome, challenging behaviors, and autism. The ICF model explicitly measures functional strengths, social role activity, community participation, and environmental facilitators. A MODEL FOR ASSESSING ENABLEMENT AMONG CHILDREN WITH ASDs THE SPECTRUM OF AUTISM AND RELATED PERVASIVE DEVELOPMENTAL DISORDERS The World Health Organization (2001) proposed a strengths- and supports-based model framework for describing individuals with disability. The ICF model describes a child’s health and well-being in terms of 4 components: (1) body structures, (2) body functions, (3) activities, and (4) participation. Body structures are anatomical parts of the body, such as organs and limbs, as well as structures of the nervous, sensory, and musculoskeletal systems. Body functions are the physiological functions of body systems, such as digestion and respiration, and also include psychological functions such as attending, remembering, and thinking. Activities are tasks done by children, including learning, communicating, walking, carrying, feeding, dress- Over the past 50 years, autism has been diagnosed using different labels and criteria. We currently support the term “ASD” to encompass the formal categorical diagnoses of autistic disorder, pervasive developmental disorder—not otherwise specified (PDDNOS), and Asperger’s syndrome. Currently, the 2 standardized criteria for diagnosing these ASDs, DSM-IV and ICD-10, are similar (Volkmar & Pauls, 2003). Core diagnostic features include impairments in communication and social interaction coupled with restrictive and stereotyped patterns of behavior, interests, and activities. Onset is in the preschool years, with delays in language understanding and use, delays in joint attention and nonverbal skills, symbolic play 2-y-old boy with autism Mother has to take off from work frequently because of child’s seizures Health maintenance organization will not allow magnetic resonance imaging or referral to a pediatric epilepsy center No out-of-home day care available for child with frequent seizures Contextual factors: Environmental barriers Unsteady in sitting, unable to crawl Fragmentation between early interventionists and explicit deliverables to enhance communication. Lack of full-day extended 3-y-old quality programs Failure to have communications strategies for nonverbal children Loves swimming with father at YMCA Unable to go to relatives “Presumed” miswiring of neurological systems involved in language, development, and complex behavioral regulation Recurrent seizures Cognitive, communicative, and neurobehavioral dysfunction. No seizures, no evidence of fragile X syndrome Lack of developmental progress, Difficulty with receptive and unable to walk or talk expressive language transitions, repetitive play, dietary rigidity Transfers toys, rolls, laughs Loves playground and music activities Infantile spasms at 6 mo, tuberous sclerosis complex 1-y-old girl with seizures and autism Participation: Age appropriate roles, chores, hobbies, and sports Societal limitations: Attitudinal, legal, policy, and architectural barriers Functional strengths: Performing activities such as running, dressing, communicating, playing Disability: Difficulty performing activities typical for peers Functional challenges: Difficulty performing an activity Impairment: Loss of organ structure or function Pathophysiology: Molecular or biochemical mechanisms interfering with cellular function Dimension: Definition Table 2. Dimensions of functioning and participation Church members request that child be kept at home during services Lack of respite services and weekend supports Special education supports, low-vision aides, bilateral ankle-foot orthoses, intense behavior management program Horseback riding Visual, cognitive, communicative, and neurobehavioral dysfunctions Difficulty with running, restricted visual fields, nonverbal, self-injurious behavior Climbing 750 g, 26-wk completed gestation, and severe retinopathy of prematurity 3-y-old girl with autism and visual disability Denied life insurance policy Because mother works outside the home, she cannot attend genetic support groups YMCA playgroup Quality preschool services and behavioral management Cartoon watching, loves Thomas the Tank Difficulty with activity, eye contact Fragile X syndrome diagnosed at age 4 Initially with hypotonia and communication delays 4-y-old boy with autism 260 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 Communicating About Autism difficulties (ie, pretend play), and difficulty with social interactions with parents and peers. Although current reviews mandate a medical evaluation for autism (Committee on Children With Disabilities, 2001b; Filipek et al., 2000), many children do not have an associated or causative medical condition (Fombonne, 1999). The medical differential diagnosis of autism includes global developmental delay, developmental language disorders (DLDs), and severe sensori-neural hearing impairments. There are also many rare neurogenetic disorders that impact on higher cortical functions including abstraction, problem solving, understanding viewpoints of others, information processing, and regulation of attention (eg, too short, too long, too inflexible) (Rapin, 1997). In addition, among a subset of children with language regression, a specific epilepsy pattern is present and called the Landau-Kleffner syndrome (Rapin & Katzman, 1998). Some uncommon medical etiologies associated with autism include untreated PKU, tuberous sclerosis complex, retinopathy of prematurity, congenital cytomegalovirus infection, and fragile X, Lesch Nyhan, and Moebius syndromes. In addition, several genetic disorders such as Down, PraderWilli, Angelman, and Williams syndromes and Duchenne muscular dystrophy have higher risks for ASDs. The lesson is not that all children with Down syndrome or Duchenne muscular dystrophy manifest behaviors consistent with ASD, but that among individuals with developmental and genetic vulnerability (ie, Down syndrome or Duchenne muscular dystrophy), higher rates of classical autism are found than the population prevalence of 1 to 2 per 1000 (Yeargin-Allsopp et al., 2003) and the ASD prevalence of 4 to 6 per 1000 (Szatmari, 2003; Yeargin-Allsopp et al., 2003). EPIDEMIOLOGY OF PRESCHOOL CHILDHOOD DISABILITIES There are improved tools for early recognition and increased awareness of the preschool presentation of children with ASDs. With 261 expanded definitions of the autistic spectrum, there are more individuals who do not have the classical comorbidities of mental retardation/intellectual disability. By including Asperger’s disorder in the autism spectrum, there is increased awareness of the social skill and motor coordination impairments that impact on school-aged children with learning disorders. Lastly, including preschool children with challenging behaviors and communicative and attention disorders as children with autistic spectrum disorder (PDD-NOS) substantially increases the number of children eligible for accommodations (504 Plans) and special education services (individualized education programs). Thus, to understand the changing epidemiology of preschool communicative, developmental, and neurobehavioral disorders, one must understand the background prevalence of communicative and cognitive disorders in early childhood. Communicative impairments associated with developmental disabilities can be classified in terms of severity (high, low) and prevalence (high, low) (Accardo, 2007). Impairments with high severity and low prevalence include classical (Kanner’s) autism (1–2 per 1000) and significant intellectual disabilities (IQ < 50–55) with a prevalence of 5 per 1000. Those with low severity and high prevalence include mild intellectual disabilities (30 per 1000), language disorders (100 per 1000), and learning disabilities (70–100 per 1000). It is because of these latter categories that as many as 20% of school-aged children may qualify for special education accommodations. Mild intellectual disabilities are defined as an IQ of 55 to 70, with adaptive skills more than 2 SDs below the mean, and are often detected in kindergarten and early elementary grades. These children are independent in communication skills and all activities of daily living. Reading and writing skills usually advance to a fifth-grade level before leveling off. Children with moderate intellectual disabilities ultimately have IQs of 40 to 55 and present with preschool language delay that later is diagnosed as a more complicated disability. These children are 262 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 Table 3. Language skills among children with communicative disordersa Single wordsd Phrasese Intelligibility 1-Step commandse Developmental language disorder High-functioning autistic disorderb Low-functioning autistic disorderc 18 (8.3) 27.2 (9.4) 30 (10.8) 23.4 (9.4) 17 (10.5) 29 (11.7) 29 (12.3) 33 (12.5) 20.4 (13.1) 36 (16.3) 30.6 (17.2) 37.4 (14.7) a Values represent age in months with (SD). IQ > 80. c Nonverbal IQ < 80. d Significant difference between groups P < .05. e Significant difference between groups P < .001. b Nonverbal independent in all activities of daily living and eventually able to communicate basic needs to a caregiver. The major sequelae of this group of disorders are difficulty in complex academics, especially in reading paragraphs and writing book reports. A key question is: What are the differences in diagnosis and developmental outcomes among children with cognitive, language, and ASDs? Rapin led a multisite multidisciplinary project whose purpose was to investigate the neurobiologic basis of ASD and related communication disorders, provide a basis for rational interventions, and improve the training of professionals who educate and care for these children (Rapin & Autism and Language Disorders Nosology Project, 1996). The cohort involved 487 children aged 3 to 7 years. Developmental language disorder (DLD) was present in 41%, ASDs were present in 36%, and intellectual disability without autism was present in 23%. The children were further divided into high-functioning autistic disorders (HADs; n = 51) and low-functioning autistic disorders (LADs; n = 125). The highfunctioning group had nonverbal IQs greater than 80, whereas the low-functioning group had nonverbal IQs lower than 80. All children received a comprehensive assessment of neuropsychologic processes including language, nonverbal intelligence, adaptive behaviors, academic abilities, and neuromotor skills. Detailed histories of prenatal, perinatal, and postnatal events; childhood illnesses; family illnesses; developmental milestones; and growth, physical, and expanded neurologic examinations were noted. Several findings were reported. The presence of developmental disabilities in parents and siblings was generally not a significant predictor for DLDs or ASDs. However, in families where one child had an ASD, there was an increased risk for other children to have either DLDs or intellectual disability. In a smaller number of families with one child with ASD, there was a second child with this disorder. Neonatal problems were generally not predictive of ASD or significantly different between the DLD and the ASD. With respect to early developmental milestones, no child with a DLD or an ASD was a late walker, defined as not walking independently at age 18 months. Late walking was present in 25% of children with global developmental delay. Difficulty with pretend play at 36 months occurred in 25% of children with DLDs, 49% of children with global developmental delay, and 71% of children with ASDs. By age 4, only 5% of children with DLDs could not engage in pretend play whereas 1 in 6 (>15%) of high-functioning children with autistic disorders and 1 in 6 children with global developmental delays continued to struggle with these play skills. Table 3 illustrates that delays in communicating in phrases and following 1-step Communicating About Autism commands significantly differentiated children with ASD from children with DLD. These findings also highlight why concerns about communicating in words and phrases and following requests without gestures are key first signs for the early recognition of autism. Overall, children with DLDs performed better in both receptive and expressive language skills than children with ASD and low nonverbal intelligence. These findings also suggest that enhancing communication skills is one of the key requirements for preschool interventions. Rapin concluded that most prenatal, perinatal, and postnatal events did not differentiate between DLDs, high-functioning ASD, autism with intellectual disability, and mental retardation. Developmentally, 31% of the intellectual disability group and 56% of the autism group with nonverbal IQ less than 80 had significantly low IQ scores (IQ < 50). This study replicated findings from the multicenter Collaborative Perinatal Project that perinatal events do not play a strong causative role in autism, intellectual disability, and DLDs (Nelson, 1991). A DEVELOPMENTAL AND BEHAVIORAL PERSPECTIVE The role of healthcare professionals Autism and ASDs have received a lion’s share of public and media attention. There is also increased recognition that has contributed to higher clinical and administrative prevalence rates over the past 2 decades. Although families and research scientists may differ on the root-causal pathways for this increase in prevalence (Baird et al., 2000; Fombonne, 2003) of children either diagnosed or currently receiving specialized treatment for ASDs, it is timely that the primary healthcare professional assumes a leadership role in guiding and supporting families during the early diagnostic process. Primary healthcare professionals, however, face several obstacles. First, they are increasingly called upon to screen for autism and other developmental disorders as part of the “well child” visits without adequate 263 infrastructure for time and reimbursement considerations (Dosreis, Weiner, Johnson, & Newschaffer, 2006). Second, although national initiatives at the Center for Disease Control and Prevention (Autism Information Center) and policy statements (Committee on Children With Disabilities, 2001b; Filipek et al., 2000) have recommended specific autism screening tools and diagnostic standards (ICD 10, DSM IV), so far very few publications have addressed the effectiveness of the implementation of these strategies. Finally, because there is no laboratory or blood test for autism, the diagnosis remains open for subjective interpretation of even formal diagnostic standards. However, consensus exists that expert clinical judgment is more reliable than algorithm diagnosis in the youngest of children (Charman & Baird, 2002). These factors separately or in combination all serve to add obstacles and confuse the role pediatricians and primary care providers play in the diagnosis and management of ASDs (Committee on Children With Disabilities, 2001b). PRINCIPLES OF THE DIAGNOSTIC ASSESSMENT Primary care providers can find guideposts in this changing landscape by beginning with the ICF strength-based framework and reviewing the principles of the early childhood diagnostic assessment. One goal of this review is to provide a bridge for the primary care provider as the information about the prevalence, diagnosis, and optimal management of ASDs evolves. Four converging factors regarding the diagnosis of ASD highlights the importance of this review. Improved ability to diagnose ASDs at earlier ages (Lord, 1995; Moore & Goodson, 2003) is linked with pressure to meet early intervention or school-based special education eligibility requirements and fueled by emerging information about the effectiveness of early identification and treatment (Lovaas, 1987; McEachin, Smith, & Lovaas, 1993; Sheinkopf & Siegel, 1998). However, at the same time, there is emerging and conflicting 264 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 Table 4. Principles of an ICF aligned developmental assessmenta 1. An integrated and functional model of child development—one that informs how best to help an individual child—must be central to any assessment and provide a strengths-based framework for the integration of gathered data. 2. Multiple sources of information about the child’s strengths and weaknesses (past and present) must be solicited during the assessment. 3. The assessment should have a predictable sequence that plays to the child’s strengths and taps his or her weaknesses. This process begins first by building alliances and a relationship with parents, obtaining a strength-based developmental history, observing child in optimal play, and functionally assessing areas of weakness. 4. To achieve optimal performance, the child must participate only in an assessment with his or her most trusted caregivers. 5. The timing of child development and the factors that affect the variation of this timing should be well known by the multidisciplinary assessment team. 6. An optimal assessment should identify the child’s strengths and weaknesses that the child brings to the next developmental challenge and form the basis for potential intervention efforts if needed. 8. An optimal assessment should not upset the child or place the child in a deficit-dominated or vulnerable position. a Adapted from Greenspan and Meisels (1996). information about the long-term stability and sensitivity of this early diagnostic process (Charman et al., 2005; Zwaigenbaum et al., 2006). It is not known which of these factors plays the dominant influence in the unmet needs experienced by children with ASD. Our clinical experience has often reminded us that the primary healthcare provider is frequently the first to identify and respond to a family’s developmental concern, and it is critical they understand and play a central role in overseeing the family’s successful negotiation of the evaluation process. Equally important, the primary healthcare provider plays an integrative and educational role for the family after the diagnostic assessment is completed and when follow-up with the referral source is limited. Based on the work of Meisels and the Zero to Three Work Group on Developmental Assessment, the principles of an optimal developmental assessment that best serve the family and primary care provider have been summarized in Table 4 (Greenspan & Meisels, 1996; Meisels & Atkins-Burnett, 2000; Meisels & Shonkoff, 1990; Shonkoff & Meisels, 2000). The best practice components of a developmental assessment for young child with delays in communication, social skills, and developmental competencies should first contain multiple sources of information about the child’s developmental progress and functional capacities. This requires that not only the parents but also the healthcare provider’s and, possibly, the day care provider’s concerns and description of the child’s strengths and weaknesses be part of the diagnostic process. A primary healthcare provider should be alarmed on behalf of the family when the referral diagnostician does not solicit or accommodate the developmental history and primary care perspective of the child from the previous well child visits in the diagnostic assessment. Second, primary healthcare providers shoulder the responsibility for increased mandates for developmental screening for ASD (Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, & Medical Home Initiatives for Children With Special Needs Project Advisory Committee, 2006). This responsibility and role increases Communicating About Autism the primary care provider’s part in the developmental assessment process because collaborative and sequential assessments are central to any high-quality autism early identification, assessment, and family support management program. Third, as primary care providers and systems of care become increasing adept in providing a medical home for children with ASD and other special healthcare needs, they need to join with the parents in identifying the child’s current competencies and strengths as well as the skills the child needs to develop to continue with his or her developmental progression. Providing tips for “surviving your child’s developmental assessment” (Seven Tips for Surviving Your Child’s Developmental Assessment assessed at http://www. zerotothree.org/site/PageServer?pagename= ter screen tips) is one way the primary care provider can remain connected to parents as they embark on the developmental diagnostic process for their child and strive to manage the child’s lifelong condition after the diagnostic assessment. Finally, the ultimate goal of developmental and diagnostic assessments appropriate for the ICF strength-based model and the medical home is that no parents will suddenly face as part of the diagnostic process the reality of uncovering a problem that they did not suspected. When primary care fulfills its ideal role, parents are heard and supported up to, during, and after any referral multidisciplinary assessment. In addition, the primary care provider plays an important role for the parents who have difficulty in relating the initial behavioral or developmental concerns with the outcome of a diagnosis of ASD. Keeping the child and the child’s behavior as the central focus of the parent’s concern and the focus of the diagnostic process helps parents recognize their child’s personhood in the diagnosis process. The primary care provider’s facilitation of parental observations after the diagnostic process and understanding the terms of the diagnosis of ASD is an invaluable support as parents adjust their internal view of their child (Baird et al., 2000). 265 Even when parents perceive the initial diagnosis of ASD as unwarranted and premature, primary care providers can adopt the “working diagnosis” perspective and join with the family to refine the diagnosis over time. It is in this context that the National Academy of Science recommendations are most pertinent. This committee recommended that all children with any ASD, regardless of label or level of severity, be eligible for special education services that comprehensively address social, cognitive, communicative, and learning skills. The therapeutic nature of this supported diagnostic process for parents should not be underestimated (Parker & Zuckerman, 1990) because it allows the introduction of structured services and for the priority of early intervention services to address communication and social skill challenges without driving parents to risky and unproven alternative treatment (Hyman & Levy, 2005). CAUTION ABOUT NONTRADITIONAL THERAPIES Parents of children with autism are barraged with promises of miracle cures, drug therapies, and nontraditional therapies to cure their child (Nickel, 1996; Tanguay, 2000). Many times, caregivers are willing to try anything to help their child. Nonethical promoters of nonscientific therapies use common ploys to seduce desperate parents into trying their treatments. Some common approaches include exploiting the natural fear of disease, preying on the uncertainty about traditional medical care, promising painless and natural treatments, and claiming miraculous scientific breakthrough and developmental cures. One promise of a scientific breakthrough was the use of secretin to cure autism. A case study was reported in the literature that 1 dose of intravenous secretin costing more than $1000 successfully eliminated symptoms in a child with autism (Horvath et al., 1998). Several scientific studies have been conducted since the original case study. One undertaken by Coniglio et al. (2001) involved children aged 3 to 10 years diagnosed 266 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 using DSM-IV criteria for autism. The goal was to determine whether a single dose of intravenously administered secretin could improve communication and socialization skills in children with autism. Subjects were randomly divided into treatment and placebo groups. The Childhood Autism Rating Scale and Preschool Language Scale–3 (PLS-3) were administered at baseline, 3 weeks, and 6 weeks after treatment. In addition, caretakers completed the Parent Perception Survey and the Gilliam Autistic Rating Scale and were asked several study-specific questions including “Do you believe your child received secretin? Have you noticed any changes in your child’s symptoms?” Results showed that children who did not receive secretin made more communicative, behavioral, and developmental progress using these standardized outcome measures. In another study, Sandler et al. (1999) randomly assigned 60 children aged 3 to 14 years to either a single treatment secretin group or a placebo control group. DSM-IV criteria were used to diagnose autism (Sandler et al., 1999). If autism criteria were not met, PDD was diagnosed. Subjects were administered the Childhood Autism Rating Scale and the Autism Behavior Checklist at baseline and at a 4-week follow-up. Again, the children assigned to the placebo treatment improved on these behavioral measures more than the secretin group. To date, there have been several other secretin trials involving more than 700 children with autism (Dunn-Geier et al., 2000; Lightdale et al., 2001; Owley & Steele, 1999; Roberts et al., 2001). In no trial was secretin a miracle cure. However, in all trials, improvement occurred over time in all children with ASDs, thus demonstrating that all children with ASDs learn. Despite the lack of evidence for secretin’s therapeutic use and even after being presented the study’s negative results, parents continued to ask the study doctors for ongoing secretin treatment. Primary care professionals need to embrace the passion parents demonstrate in their search for supports to their afflicted child. Rather than a punitive remark or avoiding a discussion about an alternative treatment, primary healthcare professionals can play a positive role by providing families valuable information to evaluate any alternative treatment. We have found some useful Web sites and handouts to offer to families when contemplating the complex issue of and risks associated with alternative treatments. 1. http://www.asatonline.org/ (Association for Science in Autism Treatment, n.d.) 2. http://www.autismresearchnetwork.org/ AN/default.aspx (National Institutes of Health Autism Research Network, 2007) 3. Parent handouts have been developed by The Autism Program. These include: a. Current Interventions in Autism— A Brief Analysis at http://www. theautismprogram.org/autismtreat ments.asp (The Autism Program, n.d.-a) b. Tips for Working With Children With Autism Spectrum Disorders at http://www.theautismprogram. org/tips.asp (The Autism Program, n.d.-d) c. Top 10 Things to Remember When Working With Children With Autism Spectrum Disorders at http://www.theautismprogram.org/ top10.asp (The Autism Program, n.d.-e) d. Tips for Daily Life—Visiting the Dentist at http://www. theautismprogram.org/dentist.asp (The Autism Program, n.d.-b) e. Tips for Daily Life—Toilet Training at http://www.theautismprogram. org/toilet.asp (The Autism Program, n.d.-c) ADMINISTRATIVE AND FUNDING REALITIES The primary healthcare provider, as the central figure in the medical home and because of his or her unique training, interest, and commitment, is perfectly positioned to Communicating About Autism understand and support the special family circumstances that each family brings with a child who has developmental differences. Unfortunately, Medicaid and private party payers do not value this expertise or commitment with their reimbursement schemes. Primary healthcare providers, pediatricians, and nurse practitioners and family practice specifically are best positioned to involve family members in planning the evaluation of a child’s development. They also foster respectful communication between parents, referrals to subspecialty physicians, and allied healthcare and educational professionals. Helping families integrate the different pieces of an assessment for ASDs (genetics, hearing, neurologic, and educational) is one valuable mandate of the medical home. The American Academy of Pediatrics, and its national medical home initiative (American Academy of Pediatrics: The National Center of Medical Home Initiatives for Children With Special Needs, n.d.), has advocated a model of primary care delivery that keeps the primary healthcare professional central to the process of identification, family understanding, professional referrals, and diagnostic assessment for children with developmental differences. At the same time, this initiatives at the American Academy of Pediatrics endeavors to find political and legal avenues to address the negative financial setbacks that most primary care providers risk when they choose to maintain this central role for their patients and families. The American Academy of Pediatrics has a toolkit as well as updated brochures to enhance the primary care provider’s skills (see www.aap.org). In addition, the National Medical Home Autism Initiative at the University of Wisconsin and the Maternal and Child Health Bureau (MCHB) is evidence, in part, of the way national organizations and federal agencies are promoting and providing technical assistance to pediatric healthcare providers who desire to work with other partners in the community to serve children with autism (Fig. 1). Adopting the ICF model with a strengthsand supports-based framework for describing 267 preschool children with ASD is a perfect match for primary healthcare professionals. In collaboration with the larger community of providers, the key goal is to provide comprehensive coordinated and compassionate care for children and families faced with the challenges of ASDs. Building on the ICF framework of enablement, primary care providers will have the structure to communicate with sensitivity and mutual respect information about the developmental diagnosis, explain current medical understanding of autism to families, and provide ongoing family support. Only then will families have the confidence to increase their requests to primary care providers for guidance about the range of traditional and nontraditional autistic-specific treatments available. In addition, this framework allows the physician to prioritize interventions that promote child functioning and enhance family well-being. The blending of the ICF framework within the primary care structure of the medical home can serve to reveal the added value of decreasing fears and stresses through efficient parent-professional partnerships. This added value reflects the teamwork of professional and nonprofessional office staff toward family-centered care management and enhanced communication. These models also recognize the wide range of differences in challenges families of children with autism face and the increased time and effort required for the ongoing monitoring of the child’s progress and family adaptation. CONCLUSION The major need for families is to feel that their primary healthcare professional listens to their concerns and understands the multithreaded information required for a diagnostic assessment. Parents also need to be continually supported in accessing comprehensive systems of early intervention and preschool education on behalf of their child. It is most important to view ASD as a developmental disorder whereby interventions to enhance 268 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 Figure 1. National Medical Home Autism Initiative: Key functions and partners (Waisman Center, 2006). communication, promote adaptive skills, and build on the child’s strengths occur. It is a dangerous practice to assume that there is a magic bullet that will dramatically cause the child to be suddenly typical. Unfortunately, the complexity of human language and the developmental neurobiology of autism do no allow for cures with injections of miracle drugs or nutrition supplements (Coury & Nash, 2003; Ozonoff et al., 2003; Volkmar & Pauls, 2003). Instead, ASD allows us to understand how all children can benefit from comprehensive and quality supports that enhance communication, adaptive skills, and functional independence at home and in the community. If the parent or the child experience challenges that are too demanding or out of control, they will not understand the current behavior and educational technologies that can make a difference (Rogers, 1998; Siegel, 1996, 2003; Smith, Eikeseth, Klevstrand, & Lovaas, 1997; Wetherby & Prizant, 2000; Wing, 2001). The role of the physician is not to be an expert on all educational practices but to know the hard task of parenting children who are motorically able but communicatively challenged and behaviorally unpredictable. Attention to family stresses and daily management supports can make a difference at home, school, and in the community. In this way families can undertake the multidimensional management strategies that promote functional, communicative, social, and adaptive skills. They then can celebrate with professionals the strengths of their child’s unique way of experiencing the world and set goals that promote steps to independence, and when challenges persist, know they will not be abandoned. Communicating About Autism 269 REFERENCES Accardo, P. J. (2007). Developmental disabilities in infancy and childhood (3rd ed.). Baltimore: P.H. Brookes. American Academy of Pediatrics: The National Center of Medical Home Initiatives for Children With Special Needs. Retrieved July 10, 2007, from http://www.medicalhomeinfo.org/ Anders, T. F., Gardner, C., Jr., & Gardner, S. E. (2003). Professional-parent collaboration—The M.I.N.D. Institute Model. In: S. Ozonoff, S. J. Rogers, & R. L. Hendren (Eds.), Autism spectrum disorders—A research review for practitioners (pp. 227–238). Washington, DC: American Psychiatric Publishing Inc. Arnold, L. E., Aman, M. G., Martin, A., Collier-Crespin, A., Vitiello, B., Tierney, E., et al. (2000). Assessment in multisite randomized clinical trials of patients with autistic disorder: The Autism RUPP Network. Journal of Autism and Developmental Disorders, 30(2), 99– 111. Association for Science in Autism Treatment. (n.d.). Retrieved July 16, 2007 http://www.asatonline.org Baird, G., Charman, T., Baron-Cohen, S., Cox, A., Swettenham, J., Wheelwright, S., et al. (2000). A screening instrument for autism at 18 months of age: A 6-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 39(6), 694–702. Benda, C. E. (1952). Developmental disorders of mentation and cerebral palsies. New York: Grune & Stratton. Bristol, M., McIlvane, W. J., & Alexander, D. (1998). Autism research: Current context and future direction. Mental Retardation and Developmental Disabilities Research Reviews, 4(2), 61–64. Chakrabarti, S., & Fombonne, E. (2001). Pervasive developmental disorders in preschool children. The Journal of the American Medical Association, 285(24), 3093–3099. Comment in: The Journal of the American Medical Association, 2001 June 27;285(24):3141–3142; PMID: 11427145. Charman, T., & Baird, G. (2002). Practitioner review: Diagnosis of autism spectrum disorder in 2- and 3year-old children. Journal of Child Psychology and Psychiatry, 43(3), 289–305. Charman, T., Taylor, E., Drew, A., Cockerill, H., Brown, J.-A., & Baird, G. (2005). Outcome at 7 years of children diagnosed with autism at age 2: Predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry, 46(5), 500– 513. Chess, S. (1978). Behavioral consequences of congenital rubella. St. Louis: CV Mosby. Committee on Children With Disabilities. (2001a). The pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics, 107(5), 1221–1226. Committee on Children With Disabilities. (2001b). Technical report: The pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics, 107(5), E85. Coniglio, S. J., Lewis, J. D., Lang, C., Burns, T. G., SubhaniSiddique, R., Weintraub, A., et al. (2001). A randomized, double-blind, placebo-controlled trial of singledose intravenous secretin as treatment for children with autism. Journal of Pediatrics, 138(5), 649– 655. Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, & Medical Home Initiatives for Children With Special Needs Project Advisory Committee. (2006). Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics, 118(1), 405–420. Coury, D. L., & Nash, P. L. (2003). Epidemiology and etiology of autistic spectrum disorders difficult to determine. Pediatric Annals, 32(10), 696–700. Dosreis, S. P. D., Weiner, C. L. B. S., Johnson, L., & Newschaffer, C. J. P. D. (2006). Autism spectrum disorder screening and management practices among general pediatric providers. Journal of Developmental & Behavioral Pediatrics, 27(2), S88–S94. Dunn-Geier, J., Ho, H. H., Auersperg, E., Doyle, D., Eaves, L., Matsuba, C., et al. (2000). Effect of secretin on children with autism: A randomized controlled trial. Developmental Medicine & Child Neurology, 42(12), 796–802. Filipek, P. A., Accardo, P. J., Ashwal, S., Baranek, G. T., Cook, E. H., Jr., Dawson, G., et al. (2000). Practice parameter: Screening and diagnosis of autism: Report of the quality standards subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology, 55(4), 468–479. Fombonne, E. (1999). The epidemiology of autism: A review. Psychological Medicine, 29(4), 769–786. Fombonne, E. (2003). Epidemiological surveys of autism and other pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders, 33(4), 365–382. Fombonne, E., & Chakrabarti, S. (2001). No evidence for a new variant of measles-mumps-rubella-induced autism. Pediatrics, 108(4), E58. Goldston, S. E., Gruenberg, E. M., & Lewis, C. (1986). Vaccinating against brain syndromes: The campaign against measles and rubella. New York: Oxford University Press. Greenspan, S., & Meisels, S. (1996). Toward a new vision for the developmental assessment of infants and young children. In: S. Meisels & E. Fenichel (Eds.), New visions for the developmental 270 INFANTS & YOUNG CHILDREN/OCTOBER–DECEMBER 2008 assessment of infants and young children (pp. 11–26). Washington, DC: Zero to Three. Halsey, N. A. (2001). Safety of combination vaccines: Perception versus reality. Pediatric Infectious Disease Journal, 20(11 Suppl.), S40–S44. Halsey, N. A., Hyman, S. L., & Conference Writing Panel. (2001). Measles-mumps-rubella vaccine and autistic spectrum disorder: Report from the New Challenges in Childhood Immunizations Conference convened in Oak Brook, Illinois, June 12–13, 2000. Pediatrics, 107(5), E84. Horvath, K., Stefanatos, G., Sokolski, K. N., Wachtel, R., Nabors, L., & Tildon, J. T. (1998). Improved social and language skills after secretin administration in patients with autistic spectrum disorders. Journal of the Association for Academic Minority Physicians, 9(1), 9–15. Hyman, S. L., & Levy, S. E. (2005). Introduction: Novel therapies in developmental disabilities—Hope, reason, and evidence. Mental Retardation and Developmental Disabilities Research Reviews, 11(2), 107–109. Levy, S. E., & Hyman, S. L. (2002). Alternative/ complementary approaches to treatment of children with autistic spectrum disorders. Infants & Young Children, 14(3), 33–42. Lightdale, J. R., Hayer, C., Duer, A., Lind-White, C., Jenkins, S., Siegel, B., et al. (2001). Effects of intravenous secretin on language and behavior of children with autism and gastrointestinal symptoms: A singleblinded, open-label pilot study. Pediatrics, 108(5), E90. Lord, C. (1995). Follow-up of two-year-olds referred for possible autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 36(8), 1365– 1382. Lovaas, O. I. (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 55(1), 3–9. McEachin, J. J., Smith, T., & Lovaas, O. I. (1993). Long-term outcome for children with autism who received early intensive behavioral treatment. American Journal of Mental Retardation, 97(4), 359–72; discussion 373– 391. Meisels, S. J., & Atkins-Burnett, S. (2000). The elements of early childhood assessment. In J. P. Shonkoff & S. J. Meisels (Eds.), Handbook of early childhood intervention (pp. 231–257). New York: Cambridge University Press. Meisels, S. J., & Shonkoff, J. P. (1990). Handbook of early childhood intervention. New York: Cambridge University Press. Moore, V., & Goodson, S. (2003). How well does early diagnosis of autism stand the test of time? Followup study of children assessed for autism at age 2 and development of an early diagnostic service. Autism, 7(1), 47–63. Murch, S. H., Anthony, A., Casson, D. H., Malik, M., Berelowitz, M., Dhillon, A. P., et al. (2004). Retraction of an interpretation. Lancet, 363(9411), 750. National Institutes of Health Autism Research Network. (2007). Retrieved July 16, 2007, from http:// www.autismresearchnetwork.org/AN/default.aspx National Research Council Committee on Educational Interventions for Children With Autism. (2001). Educating children with autism. Washington, DC: National Academies Press. Nelson, K. B. (1991). Prenatal and perinatal factors in the etiology of autism. Elk Grove Village, IL: American Academy of Pediatrics. Nelson, K. B., & Bauman, M. L. (2003). Thimerosal and autism? Pediatrics, 111(3), 674–679. Nickel, R. E. (1996). Controversial therapies for young children with developmental disabilities. Infants & Young Children, 8(4), 29–40. Offit, P. A., & Jew, R. K. (2003). Addressing parents’ concerns: Do vaccines contain harmful preservatives, adjuvants, additives, or residuals? Pediatrics, 112(6), 1394–1401. Owley, T., & Steele, E. (1999). A double-blind, placebocontrolled trial of secretin for the treatment of autistic disorder. Medical General, 6, E2. Ozonoff, S., Rogers, S. J., & Hendren, R. L. (2003). Autism spectrum disorders: A research review for practitioners. Washington, DC: American Psychiatric Publishing Inc. Parker, S., & Zuckerman, B. (1990). Therapeutic aspects of the assessment process. In S. J. Meisels (Ed.), Handbook of early childhood intervention (pp. 350–370). New York: Cambridge University Press. Rapin, I. (1997). Autism. The New England Journal of Medicine, 337(2), 97–104. See comment in: The New England Journal of Medicine. 1997 November 20;337(21):1555–1556; author reply 1556–1557; PMID: 9380125. Rapin, I., & Autism and Language Disorders Nosology Project. (1996). Preschool children with inadequate communication: Developmental language disorder, autism, low IQ. London: MacKeith. Rapin, I., & Katzman, R. (1998). Neurobiology of autism. Annals of Neurology, 43(1), 7–14. Renty, J., & Roeyers, H. (2006). Satisfaction with formal support and education for children with autism spectrum disorder: The voices of the parents. Child: Care, Health and Development, 32(3), 371–385. Roberts, W., Weaver, L., Brian, J., Bryson, S., Emelianova, S., Griffiths, A. M., et al. (2001). Repeated doses of porcine secretin in the treatment of autism: A randomized, placebo-controlled trial. Pediatrics, 107(5), E71. See comment in: Evidence-Based Mental Health. 2002 February;5(1):22; PMID: 11915825. Rogers, S. J. (1998). Neuropsychology of autism in young children and its implications for early intervention. Mental Retardation and Developmental Disabilities Research Reviews, 4(2), 104–112. Communicating About Autism Sandler, A. D., Sutton, K. A., DeWeese, J., Girardi, M. A., Sheppard, V., & Bodfish, J. W. (1999). Lack of benefit of a single dose of synthetic human secretin in the treatment of autism and pervasive developmental disorder. The New England Journal of Medicine, 341(24), 1801–1806. See comments in: The New England Journal of Medicine. 1999 December 9;341(24):1842–1844; PMID: 10588973, and The New England Journal of Medicine. 2000 April 20;342(16):1216–1217; author reply 1218; PMID: 10777377 and PMID: 10777376 C (TRUNCATED). Sheinkopf, S. J., & Siegel, B. (1998). Home-based behavioral treatment of young children with autism. Journal of Autism and Developmental Disorders, 28(1), 15–23. Shonkoff, J. P., & Meisels, S. J. (2000). Handbook of early childhood intervention. New York: Cambridge University Press. Siegel, B. (1996). The world of the autistic child: Understanding and treating autistic spectrum disorders. New York: Oxford University Press. Siegel, B. (2003). Helping children with autism learn: Treatment approaches for parents and professionals. New York: Oxford University Press. Smith, T., Eikeseth, S., Klevstrand, M., & Lovaas, O. I. (1997). Intensive behavioral treatment for preschoolers with severe mental retardation and pervasive developmental disorder. American Journal of Mental Retardation, 102(3), 238–249. Szatmari, P. (2003). The cause of autism spectrum disorders. British Medical Journal, 326, 173– 174. Tager-Flusberg, H., Joseph, R., & Folstein, S. (2001). Current directions in research on autism. Mental Retardation and Developmental Disabilities Research Reviews, 7(1), 21–29. Tanguay, P. E. (2000). Pervasive developmental disorders: A 10-year review. Journal of American Academy of Child Psychology, 39(9), 1079–1095. The Autism Program (n.d.-a). Current interventions in autism—A brief analysis. Retrieved July 16, 271 2007, from http://www.theautismprogram.org/ autismtreatments.asp The Autism Program. (n.d.-b). Tips for daily life— Visiting the dentist. Retrieved July 16, 2007, from http://www.theautismprogram.org/dentist.asp The Autism Program. (n.d.-c). Tips for daily life— Toilet training. Retrieved July 16, 2007, from http://www.theautismprogram.org/toilet.asp The Autism Program. (n.d.-d). Tips for working with children with autism spectrum disorders. Retrieved July 16, 2007, from http://www.theautismprogram. org/tips.asp The Autism Program. (n.d.-e). Top 10 things to remember when working with children with autism spectrum disorders. Retrieved July 16, 2007, from http://www.theautismprogram.org/top10.asp Volkmar, F. R., & Pauls, D. (2003). Autism. Lancet, 362(9390), 1133–1141. Erratum in: Lancet. 2004 January 17;363(9404):250. Waisman Center. (2006). National Medical Home Autism Initiative. Retrieved July 2, 2007, from http://www.waisman.wisc.edu/nmhai/FRAMEWORK. HTML Wetherby, A. M., & Prizant, B. M. (2000). Autism spectrum disorders: A transactional developmental perspective. Baltimore: P.H. Brookes. Wing, L. (2001). The autistic spectrum: A parents’ guide to understanding and helping your child. Berkeley, CA: Ulysses Press. World Health Organization. (2001). International Classification of Functioning, Disability and Health: ICF. Geneva: Author. Yeargin-Allsopp, M., Rice, C., Karapurkar, T., Doernberg, N., Boyle, C., & Murphy, C. (2003). Prevalence of autism in a US metropolitan area. Journal of the American Medical Association, 289(1), 49–55. Zwaigenbaum, L. M. D., Bryson, S. P. D., Roberts, W. M. D., Brian, J. P. D., Szatmari, P. M. D., & Smith, I. P. D. (2006). Stability of 18-month diagnostic assessment for autism. Pediatric Academic Societies, E-PSA59, 5425.1. Current articles- http://depts.washington.edu/isei/iyc/iyc_comments.html