From: AAAI Technical Report SS-94-01. Compilation copyright © 1994, AAAI (www.aaai.org). All rights reserved.
Intensive Care Monitoring and TherapyPlanning for Newborns
3), Franz
4)
Silvia Miksch1), WernerHorn1,2), Christian Popow
Paky
l) AustrianResearchInstitute for Artificial Intelligence, Schottengasse
3, A-1010
Vienna,Austria
2) Department
of MedicalCyberneticsandArtificial Intelligence, Universityof Vienna,Austria
3) NeonatalICU,Department
of Pediatrics, Universityof Vienna,Austria
4) Department
of Pediatrics, Hospitalof M6dling,Austria
Email:silvia @ai.univie.ac.at
We developed a knowledge-based system, VIE-VENT, for
monitoring and therapy planning of the artificial ventilation
of newborninfants. Clinical and textbook knowledge were
implemented in VIE-VENT’sknowledge base. Therapy planning was based on transcutaneously and invasively determined blood gas measurementsand on clinical observations.
After the selection of appropriate input parameters, measured
data werevalidated and transformedinto qualitative values. If
these values differed from target values, therapeutic actions
were proposedaccordingto heuristic clinical rules of artificial ventilation. VIE-VENTwas specifically designed for
practical use under real-time constraints in Neonatal Intensive Care Units (NICUs). VIE-VENTwas applied to the ICU
data set provided by the organizers of the AAAI-AIM-94
symposiumand a neonatal data set, which covered a neonatal case
of similar severity. It included all transcutaneous measurements and allowed to explore the full potential of VIE-VENT.
ilar severe situations as the AAAI-AIM
94 sample, but deals
with a neonate instead of a 8.5 monthsold child. Weused this
seconddata set to showthe full functionality of our system,
which was designed for neonates.
2. VIE-VENT’sSystem Architecture
Our aim in developing VIE-VENTwas to incorporate
monitoring and therapy planning tasks. The architecture of
VIE-VENT
consists of several modules: data selection, data
validation, data abstraction, data interpretation and therapy
recommendations. All these steps are involved in a single
cycle of data collection and interpretation from monitors.
Accordingto our aim to design a practically oriented knowledge-based system, we built the various modulecomponents
in analogy to the clinical reasoning process. VIE-VENT
represents a data-driven approach and is an open-loop system. A
detailed description of VIE-VENT’s
system architecture is
given in Miksch,et al. (1993).
1. Introduction
2.1 Data Selection
During the past decade, several knowledge-basedsystems
The phase of data selection is the process of filtering out
were introducedto support clinicians in the monitoringof crit- context-relevant data for further analysis. VIE-VENT’s
ically ill patients and to assist the staff in diagnosticdecision wholeinput data set is divided into continuousand discontinumaking and therapy planning (Uckun, 1993). These systems ous variables. VIE-VENT
uses the following input paramerange from simple intelligent alarms (e.g., Beneken, et al. ters:
1989) to sophisticated systems for anesthesia monitoring and (a) continuousdata:
managementof artificial ventilation, e.g., VentPlan (Rutventilator settings: FiO f, PIP, PEEP,q, tE,vi, Ve, VT
ledge, et al. 1993), SIMON
(Uckun, et al. 1993), GUARDIAN modeof ventilation: 2,IPPV, IMV,CPAP
(Hayes-Roth,et al. 1992).
transcutaneous blood gases: PtcO2, PtcCO2,
SaO
e
Closest to our approach is the SIMON
project, a ventilator (b) discontinuousdata:
monitoring system for premature infants. Wecould not apply
neonate’s personal description (e.g., name,sex)
its knowledgebase, because, firstly, SIMON’s
main issue is a
clinical parameters(e.g., weight, age, chest wall expancontext sensitive understandingof the patient’s status related
sion, spontaneousbreathing effort)
to the pathophysiologyof existing disorders with no therapy
invasively determined blood gases: pH, PO2, PCO
2
planning component included. Secondly, SIMONanalyses
site of bloodgas measurement:
arterial, capillary,
invasively determined blood gas measurements, which are
venous.
only discontinuously and infrequently determined. Moreover,
The continuous data are received every 10 seconds. The
in modernICUstherapeutic decisions are increasingly based arithmetic meansof the 10-seconddata are stored after every
on noninvasive continuous measurementsof transcutaneous 10 minutes for further analyses and trend detection. At the
partial pressure of oxygen(PtcO2), arterial oxygensaturation onset of the monitoring and therapy planning process the neo(SaO2)and transcutaneous partial pressure of carbon dioxide nate’s personal description is entered. The other discontinuous
(PtcCO2).Thirdly, its knowledgebase consists of data inter- data are either demandedfrom VIE-VENT
depending on difpretation componentswhichdo not represent the clinical rou- ferent conditions (e.g., critical ventilatory condition, elapsed
tine at our hospitals.
time intervals) or entered by users without being requested.
In this paper we present VIE-VENT’s
system architecture
The output parameters are primarily therapy recommenconcentrating on our data interpretation and therapy recom- dations. A therapy recommendationconsists of the amount
mendation components. Additionally, we apply the knowl- and frequency of the ventilator settings to be changed(e.g.,
edge base of VIE-VENT
to selected parts of the AAAI-AIM-"decrease PIP to 20"). Additionally, VIE-VENTprints
94 data set and to a secondneonataldata set, whichcovers sim- information about detected invalid measurementsand their
Thecurrentphaseof the projectis supportedby the "Jubil~umsfonds
der Osterreichischen
Nationalbank",
Vienna,Austria,projectnumber
4666.
Wealso greatlyappreciatethe supportgivento the AustrianResearch
Institute for Artificial Intelligence(OFAI)
bythe AustrianFederalMinistry
of Scienceand Research,Vienna.
91
transformations (e.g., "unplausible SaO2, classified as
unknown","calibration of PtcCO2with factor 1.3 since 5 min.
30 sec."), commentsand explanations about the health condition of the neonate (e.g., "respiratory acidosis", "PtcCO2is
substantially belowtarget range"), as well as warningsin critical situations (e.g., "extremely bad health condition, check
perfusion").
possibilities and the therapeutic goals of artificial ventilation,
i.e., the target values of PCO2and PO2, may change. We
divided the whole period of artificial ventilation into four
phases: an initial phase, a phase of controlled ventilation
(IPPV), a phase of weaning(IMV)and a phase of returning to
spontaneousbreathing. Transition from one phase to the next
is handled by rules dependingon the amountof artificial ventilation (e.g., if FiO2 can be reduced to a value _< 50%and PIP
2.2 Data Validation
to _< 20 mbars IMVis recommended).
Themajor aimof the data validation process is to arrive at
For every phase a set of target values and rules of therapy
reliable measurements. VIE-VENT
combines different kinds recommendations
are formulated. No restrictions of the quanof methodsto detect faulty data. Firstly, the plausibility of the tity of ventilator settings to be changedare defined if the
measurementsis checked. Wedefined look-up tables for all
amountof artificial ventilation must be increased for limiting
input parameters, which cover the plausible measurements an extremely severe health condition of a neonate. But VIEdepending on additional attributes, e.g., (pCO2,(arterial,
VENT
prunes the quantity of ventilator settings to be changed
IPPV), 15, 130). Secondly, we defined causal and functional to a maximum
of two parametersin case the artificial ventiladependenciesof the measurementsand the ventilator settings tion must be decreased. Context-dependent preference rules
(e.g., causal dependenciesof the chest wall expansionand the control the pruning process.
tidal volume; or a functional dependence: AMV
= VT* f,
Additionally, we defined three types of users (aggressive,
where AMV
is the minute ventilation, VTis the tidal volume normal, conservative) to represent different kinds of therapeuand f is the frequency). Thirdly, we used reliability ranking tic behavior of physicians in order to increase the acceptance
whichis derived frompriority lists of the measurements
(e.g., of our system. The most important characteristics of the user
oxygenation: invasive PO2is more reliable than SaO2and model are the maximum
of the allowed amoun~of change and
SaO2is more reliable than PtcO2). Fourthly, VIE-VENT
has the interval recommended
between invasive blood gas analytwo options to deal with missing values: a simplified system ses.
modelof neonatal respiration during the initial phase whenthe
For example,no changesof the ventilator settings are reconly reliable continuous measurementis SaO2and a set of ommended
ifpH, PCO2or PtcCO2are within target range durcontext--dependentrules applying defaults.
ing the phase of controlled ventilation.
If PtcCO2 is
increasing--represented in VIE-VENT
as slightly / substan2.3 Data Abstraction
tially / extremely below target range--respiratory or metaData abstraction is the process of transforming quantita- bolic acidosis is detected, and an increase of f or PIP is
tive data of the observable systeminto qualitative values. In recommended.Dependingon the degree of abnormality of the
VIE-VENT,the basis for transforming blood gas measure- blood gas measurementand the type of physician, a different
ments are schemata,which categorize the data in seven quali- amountof changeis suggested(e.g., if PtcCO2is substantially
tative categories depending on the degree of the blood gas below target range and the "normal" user type is active, then
abnormalities (slightly/substantially/extremely below target an increase of the PJP of 15%is recommended).
range, target range, slightly/substantially/extremely above
VIE-VENTrecommendschanges of the ventilator settarget range). These schemata are defined for all kinds of tings as long as the conditions for the changeshold and the setbloodgases dependingon the samplingsite (arterial, capillary, tings are not changed by the physician. If the physician
venous, transcutaneous) and the modeof ventilation (IPPV, changes the ventilator settings, her/his actions have highest
IMV).
priority. VIE-VENT
accepts the changes as a correct decision
and
waits
for
10
minutes
adaptation time without giving any
2.4 Data Interpretation and Therapy Recommendations
therapy recommendation. The other components of VIENeonatalrespiration in our systemmodelis represented by VENT
are still active during this phase. After this delay time,
two processes, ventilation (CO2elimination) and oxygenation VIE-VENT
starts criticizing the ventilator settings again.
(oxygenuptake). Ventilation is reflected by the blood tension Therefore, VIE-VENT
recognizes a fruitless or even a wrong
of CO2(PCO2or PtcCO2).Ventilation is increased (and PCO2 adjustment of the ventilator settings and forces to change
or PtcCO2decreased) depending on an increase of the AMV them.
(AMV
= VT* f). The VTis strongly but not linearily related
the peakinspiratory pressure (PIP) and clinically to the extent 3. Applying VIE-VENT
to Sample Cases
of chest wall expansion. Independentlyof the ventilation proWe applied VIE-VENTto the AAAI-AIM-94ICU data
cess, the PCO2or PtcCO2maybe increased due to a poor pulmonaryperfusion or to right to left shunting. Oxygenationis set and a neonatal data set. Weassumeda "normal" type of
user in both cases.
reflected by the blood tension of 02 (PO2or PtcO2). Oxygenation is increasedwith a raising of the inspiratory oxygencon- 3.1 Our Evaluation Conception
centration (FiO2) and of the meanairway pressure (MAP).
Our main issue was the evaluation of VIE-VENT’sdata
MAPincreases with PIP, inspiratory time (tl) and positive interpretation and therapy recommendationcomponents. Two
endexpiratory pressure (PEEP). Independently of the oxygen- domainexperts participated in the evaluation. The physicians
ation, PO2or PtcO2maybe decreaseddue to right to left shunt- ranked VIE-VENT’stherapy recommendations, warnings
ing and an increased pulmonaryvascular resistance, which and explanations as "correct", "correct, but needs smoothing"
itself at least partly dependson the PCO2.
and "incorrect" and the therapeutic actions of the provided
Dependingon the course of the disease, the monitoring cases compared to VIE-VENT’srecommendations. They had
92
to rank the decision steps in the AAAI-AIM-94
data set and in
our neonatal data set.
3.2 Evaluating the Original AAAI-AIM-94
ICU Data Set
because dependingon the invasive blood analyses at 4:30 and
6:11 and in respect to the high PEEP(9 mbars), they additionally would have recommendedto decrease the PEEP.
3.3 Evaluating our Neonatal Data Set
3.2.1 The Data Selection and Transformation
Weused the following data subsets from the AAAIAIM-94sample: the continuous measurement of SaO2(during approximately12 hours), the ventilator settings: FiO2, f,
PIP, PEEP,VT, arterial blood gases pH, PO2, PCO2and the
modeof ventilation CMV.
In our evaluation process we compressedthe time axis by
the factor of 6, resulting in oneminuteintervals of the data set.
Weaddeda default value of inspiratory time ti of 0.7 and calculated the correspondentexpiratory time tE (f = 60 / (ti+tE)).
The modeof ventilation CMVis equivalent to our phase of
controlled ventilation (IPPV). Weused four of the available
five arterially determined blood gases. Westopped VIEVENTafter receiving the last continuous measurement of
SaO2because the last blood gas analysis was available only 54
minuteslater.
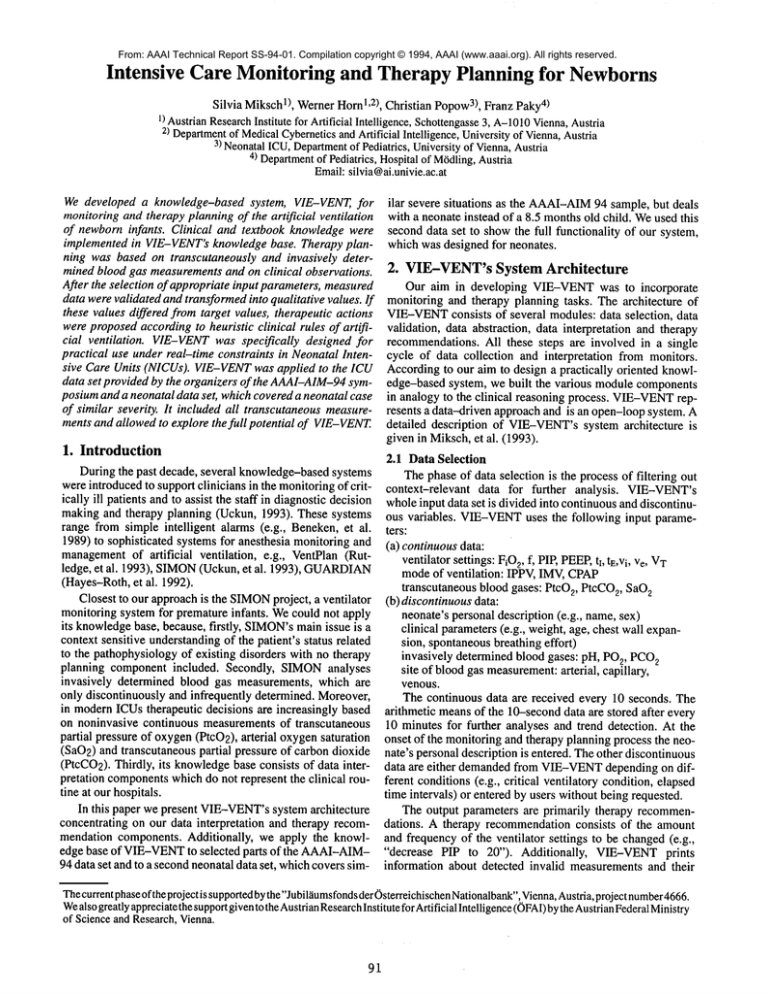
3.3.1 Case Description
Weapplied VIE-VENT
to a historical case of comparable
severity from one of our neonatal ICU’s case base to demonstrate the full functionality of our system. Wechose a male
premature infant with a birth weight of 2,920g, whopresented
with a history of oligohydrammios,bilateral hydronephrosis
due to an urethral valve. Moreoverhe had lung hypoplasia,
massive ascites and was in circulatory shock. He was ventilated immediatelyafter birth and received exogenoussurfactant three and 12 hours after birth. Our input parameters are
listed in chapter 2.1. Our therapeutic recommendationsare
based on the transcutaneous blood gases (SaO2, PtcO2,
PtcCO2)and on three capillary blood gas analyses (PcCO2,
PcO2,pH). Figure 1 presents these values (upper two charts)
and the ventilator settings (lower four charts) whichshowthe
physician’s actions (by a- line) and VIE-VENT’srecom3.2.2 Results
mendations (by a small Atriangle). The acting physician’s
Wedid not apply the restricted modeof the initial phase decisions and VIE-VENT’stherapy recommendations were
because there were arterially determined blood gases avail- retrospectively analyzed by our two domainexperts.
able since the beginningof the treatmentand it was unrealistic
that such a severely ill child wouldbe monitoredin a restricted 3.3.2 Results
way during approximately 12 hours. Moreover, we did not
In general, VIE-VENT
anticipated the acting physician’s
have any information about the chest wall expansion or the decision. However,when the SaO2increased above the norspontaneous breathing effort, which is temporally needed in mal range, the physicians gave clinical priority to a reduction
the restricted mode. A problem of the AAAI-AIM-94
case of the high PIP instead of a reduction of the high FiO2. Morewas that PIP and PEEPwere set extremely high and that VIE- over, the physician was more conservative in reducing the
VENT
suggests changes to the ventilatory parameters mainly FiO2 (steps of 5%compared to VIE-VENT’ssuggested 10%)
in relation to changesof the PtcCO2.However,there were only as he wasafraid to produceflip--flopping of the SaO2due to a
four invasively determined blood gas analyses within 12 too rapid reduction of the FiO2. Additionally, they criticized
hours. Additionally, hand bagging for raising the PCO2is a VIE-VENT’stherapy recommendations for suggesting a too
rather unusualtherapeutic action at both of our clinical depart- dramatic reduction of the FiO2. The evaluating experts critiments. Weenlarged our knowledge-baseby recognizing hand cized the acting physicianfor not increasing the rate (f) and the
baggingand classifying data values during this period as arti- PEEPearly enough in view of the high PtcCO2. VIE-VENT
facts.
recommendedsuch changes several times.
For VIE-VENT’stherapy recommendations one general
trend was discovered: VIE-VENTrecommended mainly a References
decrease of the PIP. However,the unusually high PIP was not Beneken
J.E.W.,AaJ.J. vander: Alarmsandtheir Limitsin Monitoring,
changedin the samplecase for morethan 6 hours (6 hours 29
Journal of Clinical Monitoring,5(3),pp. 205-10,1989.
minutes). Moreover,within the next 6 hours, PIP was alterna- Hayes-Roth
B., Washington
R., AshD., HewettM., Collinot A., Vina
tively decreased and increased without any corresponding
A., SeiverA.: Guardian:A PrototypeIntelligent Agentfor Intenclinical information(43, 40, 43, 42, 43, 42, 41). Thefirst artesive-CareMonitoring,Artificial Intelligence in Medicine,4(2),
rial blood gas analysis (23:16), whichwasinterpreted as hypopp.165-66, 1992.
xemia and respiratory
acidosis,
forced VIE-VENTto MikschS., Horn W., PopowC., Paky F.: VIE-VENT:
Knowledgerecommenda decrease of the PIP. Oxygenation was worse
BasedMonitoringand TherapyPlanningof the Artificial Ventilathan ventilation at a FiO2 of 50%.VIE-VENT
therefore tried
tion of Newborn
Infants~in Andreassen
S., et al. (eds.), Artificial
Intelligencein Medicine:Proceedings
of the 4th European
Conferfirstly to decrease the very high PIP and prunedthe other therence
(AIME-93),
lOS
Press,
Amsterdam,
pp.218-29,
1993.
apy recommendations. In summary, VIE-VENT recomG.E., Farr B.R., TovarM.A.,PolaschekJ.X.,
mendeddecision steps 31 times: 16 times a decrease of PIP RutledgeG.W.,Thomsen
BeinlichI.A., SheinerL.B., FaganL.M.:TheDesignand Implewas recommended,
once a decrease of the FiO2 and an increase
mentationof a Ventilator-management
Advisor,Artificial Intelliof the f (as a response to the invasive blood gas analysis at
gencein Medicine,5(1), pp.67-82,1993.
4:30). On4 occasions, the ventialtor settings werekept and on
Diagnosisin
10 occasions, VIE-VENT
only monitored the patient based on UckunS., DawantB.M., LindstromD.P.: Model-based
Intensive CareMonitoring:the YAQ
Approach,Artificial Intelli10 minutes adapting time after a changeof the ventilator setgencein Medicine,5(1), pp.31--48,1993.
tings or hand bagging.
UckunS.: Intelligent Systemsin Patient Monitoring
andTherapyManBoth physicians ranked 29 recommendations of VIEagement, Stanford University, Knowledge
SystemsLaboratory,
VENTas "correct", two as "correct, but needs smoothing"
Report KSL93-32, 1993.
93
75
i
I
i
/
i
I
:
i
t
,o .-.~ .....
~............
!............
::............
P~cc~2
...........
!! ....
i....
~)~A........ i ............
!: ............
i: ............
Ptc02
....
!
!
!
| ,,-,,.._...._~-!:
v \ /i~ ’, :
:
~ / : N
:
:
:
PcC02 []
’
8-----: :..... [] ..... : ............ :" ..........
°1 ~~i ......
\ "............ : ............ :i............ :i............ -’:............ ::............ :::........................
Pco2~ :
,,
40-
,
,
,
.,,
i ............ " ......... ’-~---~-.-
60--.i ...........
...............
..........................
iI...
.-
....
,
.....
’ ..........%~.i......z~.....~.._...v~............... ~............ ; ............ ~ ............ : ....
i... . .......
~, .....................
’,
~,
......
,
-;-~--
~._f .~.......
,,’
~..¢~.
__~
,
’,
,- ....... x..~.,,’
,, ..........2Y........
~’vk...... .;.~:~.,---
~
..............................................................
!t
20- ... ,-~.~:~,j: ......... ",.... 3.J
,, %.................
............................................
017:001
18!00
19!00
20!0021:00i
22:001
23!00
9O-----~,
............
~ ............................
m m- ,It-
-Inl
.....
A i
i
80
70
l:b0
2:b0
3:~)0
4:~)0
5:b0
m
J-~,~------i-~
........: ...........
’i ...........
100-
0:b0
I
,i
, - ...........
A
I
IIm
, .............
.............
,,~- .......................
...
~ ............
~__.
FiO2 i
~
:i
t
t
~A
...............................
60-"--~.... ta-.at.~...a........ t .... , .......am...A.!
tat n
n
m
i
, ......... .a ......................................................................
I n :maunt nan~~,nanm..............
nn
N
/ .......................................................................................................
i..
50Ate_
1
"1o
/
34-~i~:~~~i~:~~!~~i~~~i~i~:~!~:~i~i~:~
I30- i V--~i
’
’
26- "~ .....
! .......................................
22
35¯
I
...a,
:: I ::
i I i
i
::
::
:: ~m ::
-: ............ i-l--~....... I ............ i ............. :: ......................... ’: ............ : rig ......
i ....
I
’
t ............
............
I
, .............
11’ ............
a ............
t ............
’
~ ............
I
, .............
, ............
a, ............
I
t .........................
, ....
3--.-."........=--~--i,u,-~.-.
I:
, ,..................
............
L............
i...............
,............
,,.........................
i............
i............
~............
~............
~............
2-; ......~............
i............
i........................
i...........
i
2.5-""~
i
i
i
i
i PEEP
Figure 1: Blood gas measurements(top 2 charts) and therapy actions (physician- ; VIE-VENT’s
recommandations:
94