State Plan to Address Health Promotion and Disabilities
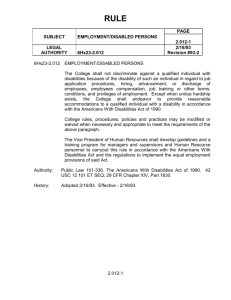
advertisement

State Plan to Address Health Promotion and Disease Prevention in Populations with Disabilities By The Disability and Public Health Planning Group May 2013 1 Table of Contents The Disability and Public Health Planning Group………………….…………………3 Executive Summary ……………………………………………………………………………….4 I. Introduction ………………………………………………………………………………..6 II. Methods ……………………………………………………………………………………..9 III. Priority Areas and Recommendations ………………………..……………….10 1. Access to Care ………………………………………………………..…………10 2. Environments Where We Live, Learn, Work and Play ………..12 3. Awareness and Promotion of Health Equity ………………………14 4. Data …………………………………………………………………………….…..16 5. Emergency Planning and Response…………..……………………….18 IV. Next Steps for Health Equity in New Hampshire……………..…………..20 Appendix A: Strategies and Activities…………………………………………………..21 2 The Disability and Public Health Planning Group This publication was supported by Grant / Cooperative Agreement Number 1U59DD000954-01 from the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the views of CDC. The New Hampshire Disability and Public Health project (DPH) is a collaboration between the New Hampshire Division of Public Health Services and the Institute on Disability at the University of New Hampshire. The overarching goal of the collaboration is to promote and maximize health, prevent chronic disease, improve emergency preparedness, and increase the quality of life among people with disabilities. DPH is led by Charles Drum, MPA, JD, PhD, Director of the UNH Institute on Disability and José Their Montero, MD, Director of the NH Division of Public Health Services. The NH Disability Community Planning Group, the project’s advisory board, provides input on methods for achieving program goals, objectives, and activities, and assists in leveraging resources and partnerships within the state. Disability Community Planning Group Members Richard Cohen, NH Disability Rights Center Diana Dorsey, Special Medical Services Bonnie Dunham, Parent Information Center Debbie Krider, Granite State Independent Living Martha-Jean Madison, NH Family Voices Kris McCracken, Manchester Community Health Center Jo Moncher, Military Community Programs John Richards, NH Governor’s Commission on Disability Julie Smith, IOD Consumer Advisory Council Carol Stamatakis, NH Council on Developmental Disabilities Trinidad Tellez, Office of Minority Health & Refugee Affairs Allyssa Thompson, National Multiple Sclerosis Society, New England Chapter Gloria Fulmer, Easter Seals NH Disability Services 3 State Plan to Address Health Promotion and Disease Prevention in Populations with Disabilities Executive Summary In 2012, the Institute on Disability at the University of New Hampshire and the Division of Public Health Services entered a cooperative agreement with funding from the Centers for Disease Control and Prevention to promote and maximize health, prevent chronic disease, improve emergency preparedness and increase the quality of life among people with disabilities. With the aim to infuse disability components into existing public health programs and activities, the new public-private partnership identified the need for a clear plan to guide its work in the state of NH (small “s”). The State Plan to Address Health Promotion and Disease Prevention in Populations with Disabilities outlines strategic priorities for this partnership. The scope and implementation of the plan is not limited by the resources of State Government, nor by the capacity of a single person, agency or organization. This plan is a call to action for organizations and community members to join the NH Disability and Public Health Planning Group to implement this agenda across multiple sectors. Five priority areas have been identified, and summary recommendations from each area are as follows: Access to Care Expand access to high quality and affordable healthcare. Promote an integrated, whole person approach. Develop community members’ health literacy and capacity to navigate the healthcare system. Support efforts to improve providers’ capacity to serve populations with disabilities. Improve the education that providers receive on patient-centered, culturally responsive care. Ensure access to ASL interpreters, AAC, and medical information in alternate formats. Advocate for funding streams tied to appropriate care. Environments Where We Live, Learn, Work and Play Increase access to physical activity and recreation, access to healthy foods, and safety in neighborhoods in which populations with disabilities live, learn, work and play. Expand accessible transportation alternatives and improve use of existing options. Support initiatives that encourage populations with disabilities to build networks. Improve early childhood development and school-based programs’ cultural effectiveness. Expand accessibility and effectiveness of education and training opportunities for people with disabilities. Encourage employers to recruit, train, and retain people with disabilities for staff and leadership positions. 4 Awareness and Promotion of Health Equity Educate and involve partners outside the health sector who impact where we live, learn, work and play in improving health for populations with disabilities. Incorporate concepts of civic and social responsibility in health and equity discourse. Identify and pursue funding opportunities to support the priorities of this plan. Encourage public, private, and nonprofit organizations to prioritize and budget for health equity. Build and maintain a collaborative public-private partnership structure to implement the plan. Influence and create public policy that supports health and equity. Data Establish NH DHHS guidelines and policy for the collection of data on disabilities as a model for other agencies and organizations. Dedicate resources for electronic data system improvements and quality assurance. Train collectors and submitters of data to use NH DHHS policy. Educate the public about the collection of disabilities related data. Work with data stewards to stratify their data to identify disparities on populations with disabilities. Monitor and report on health care utilization and the health status of people with disabilities. Emergency Preparedness and Response Provide technical assistance and model plans to local emergency management directors; regional public health emergency planners to facilitate complementary planning in accordance with the ADA. Ensure the State of NH Emergency Operations Plan respects the equal liberty, autonomy and dignity of all persons across all Emergency Support Functions as appropriate. Provide technical assistance and model plans, including Continuity of Operations Plans, to private agencies and businesses supporting individuals with disabilities. Foster engagement of individuals with disabilities in local, regional, and state-level emergency planning and exercises. Increase the number of individuals and families that are personally prepared for emergencies to the greatest extent possible. Improve the ability to share information between state and local emergency responders about the location and needs of individuals with disabilities. Activate health, medical and shelter facilities during emergencies that meet ADA requirements and are staffed by well-trained staff and volunteers who can address the needs of individuals with disabilities. Integrate disabilities service providers into local and regional systems that provide situational awareness during emergencies. Support disabilities service providers capacity to continue to provide services during emergencies 5 I. Introduction In 2012, funding from the Centers for Disease Control and Prevention (CDC) established the Disability and Public Health project (DPH), collaboration among CDC, the Institute on Disability at the University of New Hampshire, and the Hew Hampshire Division for Public Health Services. The overarching goal of the collaboration is to promote and maximize health, prevent chronic disease, improve emergency preparedness, and increase the quality of life among people with disabilities. One of the initial actions of DPHS was to convene a board of advisors into the Disability Community Planning Group. The Group includes experts, advocates, and representatives from both public health and disability. The work group developed this plan using a collaborative planning process involving diverse public, private and nonprofit stakeholders and using as a template the State Plan to Address Health Disparities and Promote Health Equity in New Hampshire. The goal of this plan is to define statewide priorities and prepare recommendations to advance health equity for NH residents with disabilities. The scope and implementation of the plan is not limited by the resources of State Government, nor by the capacity of a single person, agency or organization. What are Health Disparities? Not everyone in the United States enjoys the same health opportunities. Studies show that certain populations, including racial, ethnic, and linguistic minorities and people with disabilities, often experience poorer than average health and health outcomes. In 2005 the Surgeon General’s Call to Action to Improve the Health and Wellness of Persons with Disabilities reminded the nation that “Health and wellness are not the same as the presence or absence of a disability; they are broader concepts that directly affect the quality of a person’s life experience.”1 Health disparities among people with disabilities have been well documented at the national and state level. Data from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS) presented in the 2012 New Hampshire Disability and Public Health Needs Assessment show that people with disabilities are more likely to be smokers, more likely to be obese, and less likely to receive certain clinical preventive services and screenings than people without disabilities.2 What Factors Influence Health? Barriers in access to health care and differences in the quality of care received contribute to health disparities. Overcoming cultural, linguistic, and environmental barriers, especially, are 6 critical to accessing high quality health care. However, health is not merely the result of medical or clinical care but the sum of what we do as a society to create the conditions in which people can be healthy.3 Other factors are now recognized as being equally, if not more important in determining one’s health and health status including income and poverty status, education, employment and working conditions, housing quality, and environmental features including access to healthy food choices, walkable or wheelable streets, and safe neighborhoods. This complex array of social, cultural, and environmental factors that impact one’s quality of life are called social determinants of health, and they contribute significantly to health disparities. Figure 1 illustrates these diverse factors, or social determinants, that impact health. It is the combined differential experiences in access to health care, quality of healthcare, individual health behaviors, and social determinants that result in inequalities in health for racial, ethnic, and linguistic minority populations and for people with disabilities. FIGURE 1. Factors that Determine Health 1 1 Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health. Stockholm: Institute for Future Studies; 1991. 7 Why Does NH Need this Plan? NH residents with disabilities share concerns for health, housing, education, employment, and quality of life. Some populations struggle because they do not have adequate opportunities to maintain optimum health. We succeed as a state when we ensure opportunity for all, including the opportunity for health and well-being. By applying our ingenuity, we can make better use of our limited resources, progress towards solving health disparities affecting the NH disabled population and develop programs and services that are fairly distributed and improve their access to health promotion and disease prevention services accessible across all communities. Developing a State Plan to Address Health Promotion and Disease Prevention in Populations with Disabilities will focus our collective efforts to promote initiatives and policies that can help make our communities healthier places to live, learn, work and play for all. A State Plan will serve as a guiding document for a variety of organizations and coalitions, some of whom have been working to eliminate health disparities on disease promotion and disease prevention for the population with disabilities in NH for years. While much has already been accomplished, continued collaboration will be critical to achieve systemic change. Now is the time to focus the energy of these groups by improving collaboration. The State Plan also clearly presents these issues for a wide audience, including new leaders and stakeholders who have not worked on these issues in the past. This plan will help to engage new partners as issues of health and equity gain momentum and importance in NH. 8 II. Methods The State Plan to Address Health Promotion and Disease Prevention in Populations with Disparities in New Hampshire was developed through a collaborative, participatory process during the summer/fall of 2013. The planning process included two phases. Phase I During the late spring early summer of 2013 a small group took as template the Disparities plan and reviewed the results of the disabilities assessment and the objectives and goals of the grant (insert appropriate names) Phase II Phase II was the review by the Disability Community Planning Group. Phase III Phase III will offer an opportunity for interested partners and community members to become more engaged as the State Plan is implemented. As a living document, this State Plan will guide the work of the NH taskforce for at least 5 years, and progress towards the objectives will be monitored by the steering committee. 9 III. Priority Areas and Recommendations 1. Access to Care NH’s growing identification of populations with disabilities challenges the healthcare system to adapt to meet a broad spectrum of new, often unrecognized or unknown needs. The patientcentered care each healthcare organization strives to offer requires a high level of sensitivity and responsiveness. At the same time, requirements to provide appropriate care have increased. Given the high cost of U.S. healthcare, providers face real challenges in their efforts to provide high quality healthcare to the state’s entire population. At the same time, NH is home to a complex healthcare system. Even when individuals are insured, they often have to advocate for themselves or follow complicated directions to navigate the system, receive test results, locate specialists, or care for all aspects of their mind and body. In this context, achieving high quality health poses unique and complex challenges for populations with disabilities and providers. Key Points Access to affordable and quality health promotion and disease prevention services disproportionately affects populations with disabilities. Integrated care is essential for ensuring healthy individuals. This will require changes across the system. Federal regulations require that healthcare providers ensure effective communication with their patients, but there is limited funding available to support providers in this effort. Culturally responsive care and improved health literacy can greatly improve health outcomes and well-being for populations with disabilities. 10 Recommendations Healthcare Access Expand access to high quality and affordable health promotion and disease prevention healthcare. o Expand access to health insurance coverage and maximize opportunities presented by the implementation of the Affordable Care Act (health care reform). o Develop high quality patient centered medical homes for all. Promote an integrated health perspective to include the whole individual. Develop community members’ health literacy and capacity to navigate the healthcare system. Cultural Competence Support efforts to improve providers’ capacity to serve populations with disabilities. o Require training on cultural competence on populations with disabilities and on all forms of discrimination as part of training, licensure, and continued credentialing of all health professionals. o Promote culture change within healthcare organizations to improve the delivery of culturally responsive care. Improve the education that providers receive on establishing patient-centered, culturally responsive practices. Communication Ensure and/or expand access to ASL interpreters, augmentative and alternative communication, and medical information in alternate formats. Advocate for funding streams tied to appropriate preventive healthcare for populations with disabilities. o Support efforts to improve organizations’ capacity to serve this population. 11 2. Environments Where We Live, Learn, Work and Play The economic, social and environmental conditions individuals experience on a day-to-day basis play a significant role in shaping their health and quality of life. Factors related to individual and community health status that challenge most NH residents—finding a job or housing in troubled economic times, finding transportation options—also affect populations with disabilities, often to a greater extent. It is the combination of factors related to where we live, learn, work and play that set the stage for health and well-being. Key Points The neighborhoods we live in, and the context of daily living, directly influence our health and well-being. This includes housing, education, employment, safety and other factors. Accessible, affordable transportation is of crucial importance to ensure equality of opportunity for health care, education, housing, employment, and other essentials of daily life. Academic success and educational attainment are directly linked to an individual’s ability to achieve socio-economic success and well-being. Populations with disabilities face significant social and cultural barriers in school that limit their chances for success. Populations with disabilities often face greater challenges in living healthy lifestyles due to social, cultural and environmental factors including discrimination and social isolation. 12 Recommendations Built Environment Increase access to physical activity and recreation, access to healthy foods, and safety in neighborhoods in which populations with disabilities live, learn, work and play. o Assist residents with disabilities in securing housing in safe and accessible neighborhoods. Expand accessible transportation alternatives and improve use of existing options. Social Inclusion Support initiatives that encourage populations with disabilities to build networks. o Encourage networking and community building for individuals with disabilities to address issues of isolation. o Encourage networking and community building between individuals with disabilities and the general population to foster integration. Education and Workforce Development Improve early childhood development and school-based programs’ cultural effectiveness. o Integrate culturally competent programming into early childhood development and school-based programs to improve integration for populations with disabilities and their families. Expand accessibility and effectiveness of education and training opportunities for people with disabilities. o Reach out to and include residents with disabilities in education and training opportunities including post-secondary education and vocational training programs. Encourage employers and labor unions to dedicate resources to recruitment, training and retention of people with disabilities for staff and leadership positions. 13 3. Awareness of Health Promotion and Disease Prevention as a Health Equity Issue In 2012, America’s Health Rankings rated NH the third healthiest state overall in the United States.2 But given the results of the reports and qualitative inputs examined for this State Plan, the question is: for whom? It is clear that the benefits of our healthy environment and our healthcare system are not equally distributed across the NH population. Populations with disabilities face a range of challenges in seeking a healthy lifestyle. This directly impacts their health and ability to achieve well-being. The importance of raising awareness of issues unique to these populations is increasing in urgency as diagnosis and early identification of disabilities increases and as these disparities persist. Key Points NH is considered the third healthiest state in the U.S., but not all residents experience this healthy status. Many health care providers and other organizations are unaware of the challenges populations with disabilities face when accessing health promotion and disease prevention services. Many public, nonprofit, and private sector organizations within and outside the health sector lack appropriate policies, systems, and processes, to address program and policy issues relating to disabilities. Promoting health promotion and disease prevention that meets the needs of NH’s population with disabilities requires funding; possible approaches include exploring new multi-sectorial approaches, redirecting budgets, and seeking new grants and funding streams. 2 America’s Health Rankings, New Hampshire (2010), Available online at http://www.americashealthrankings.org/yearcompare/2009/2010/NH.aspx. Accessed December 2010. 14 Recommendations Education and Outreach Educate and involve partners outside the health sector who impact where we live, learn, work and play in improving health promotion and disease prevention for populations with disabilities. o Develop materials and approaches to educate professionals, leaders and decision-makers about the social determinants of health, health equity, cultural competence and disabilities. o Encourage collaborations with new partners who influence community-level factors and systems that impact health. Incorporate concepts of civic and social responsibility in health and equity discourse. Funding Identify and pursue funding opportunities to support the priorities of this plan. o Coordinate funding initiatives across sectors to focus efforts and avoid duplication, and to address health promotion and disease prevention inequities for population with disabilities, as well as social determinants system-wide. Encourage public, private and nonprofit organizations to prioritize and budget for health equity. o Examine current operations and budgets to seek ways to promote health equity within existing, routine activities. o When distributing funding throughout the state, require applicants to demonstrate their commitment to health and equity in their response to RFPs. Infrastructure and Policy Build and maintain a collaborative public-private partnership structure to implement the plan. Influence and create public policy that supports health and equity. 15 4. Data As NH diversifies, it becomes increasingly important to understand and address how populations with disabilities experience health disparities. This necessitates an understanding of differences in health and in factors that affect health including health care, social determinants, and individual behavior. In order to understand and address these variations, we must be able to measure them. This requires common standards for what information is collected, how it is collected, training of data collectors, and how data is utilized. At the same time, public education and engagement is necessary so that populations with disabilities understand the importance of data collection and feel comfortable with supplying the information. Key Points Improving collection of data on disabilities is a priority for identifying, tracking and monitoring health disparities and improvements in health equity. Health and human service organizations in NH vary in their collection, reporting and utilization of disabilities related data. NH public health data stewards indicated that they would like guidance and more extensive training on the implementation of standards for the collection of disabilities related data. There may be some procedural challenges to implementing the collection of disability data in the public health data sets. Different data sets might require changes in contract language, policy, administrative rules or legislation. There are certain limitations on the capacity to collect data because of small sample sizes. Overcoming these limitations may require additional resources to capture information about subgroups. 16 Recommendations Guidelines and Systems Establish NH DHHS guidelines and policy for the collection of disability related data as a model for other organizations and state agencies. o Collaborate with stakeholders to define a list of relevant data fields for the state and develop a system for periodic updates. Dedicate resources for electronic data system improvements and quality assurance. Training and Education Train collectors and submitters of disabilities related data to use NH DHHS policy. o Create a forum for providers and data stewards to communicate and understand the importance of disabilities data collection. Educate the public about the collection of disabilities related data. Data Use Work with data stewards to stratify their data to identify health disparities experienced by people with disabilities. Monitor and report on health care utilization and the health status of people with disabilities. 17 Emergency Planning and Response Engaging individuals with disabilities in emergency planning and meeting their needs during emergency events is a high priority at all levels of government, as well as for the private individuals and agencies who support them. In addition to ensuring a strong and sustainable response capacity, strengthening community resilience is a key factor with respect to mitigating the impact from emergencies as well as restoring community-based systems of care to their pre-disaster capacity. While in many instances individual entities and individuals have a clear view of their role and responsibilities in preparing, responding and recovering from emergencies a more significant challenge is developing a comprehensive, systems-based approach to improve community resiliency. Key Points Individual units of local, county and state governments have clear mandates and responsibilities to prepare for, respond to, and recover from emergencies. There are a large number of private agencies and businesses in NH that support individuals with disabilities that are at different levels of preparedness. NH’s experience during recent emergencies has highlighted an higher level of vulnerability among some individuals with disabilities. Many times individuals with disabilities are not effectively engaged in local and state emergency planning efforts. Individuals and families who are personally prepared to the greatest extent possible increases personal and community resilience. 18 Recommendations Planning Provide technical assistance and model plans to local emergency management directors; regional public health emergency planners to facilitate complementary planning in accordance with the ADA. Ensure the State of NH Emergency Operations Plan respects the equal liberty, autonomy and dignity of all persons across all Emergency Support Functions as appropriate. Provide technical assistance and model plans, including Continuity of Operations Plans, to private agencies and businesses supporting individuals with disabilities. Foster engagement of individuals with disabilities in local, regional, and state-level emergency planning and exercises. Increase the number of individuals and families that are personally prepared for emergencies to the greatest extent possible. Response Improve the ability to share information between state and local emergency responders about the location and needs of individuals with disabilities. Activate health, medical and shelter facilities during emergencies that meet ADA requirements and are staffed by well-trained staff and volunteers who can address the needs of individuals with disabilities. Integrate disabilities service providers into local and regional systems that provide situational awareness during emergencies. Support disabilities service providers’ capacity to continue to provide services during emergencies. Recovery Ensure access among individuals with disabilities and their services providers to federal and state recovery programs, including financial assistance, following emergencies. Ensure that disabilities services providers are included in local and statewide recovery planning to restore services, facilities, and infrastructure within the public health, health care delivery, and human services sectors. 19 IV. Next Steps for Health Equity in New Hampshire The NH Disability Community Planning Group developed this State Plan to Address Health promotion and disease prevention in populations with disabilities, including recommendations to improve health and access to health care for NH’s populations with disabilities. This plan is a call to action for agencies, organizations and individuals across the public, private and nonprofit sectors of the state. Many of these recommendations are directed to stakeholders in the health and health care sectors. However, to truly implement the plan and its vision for health equity for populations with disabilities, NH will need a broad based community effort that reaches beyond the traditional “health” domain and approaches it from a multi-sectoral perspective that addresses the social determinants of health: education, housing, employment, and the context and environment of daily living for populations with disabilities. DPHS and the Disability Community Planning Group invite stakeholders throughout New Hampshire to play their part in bringing this vision to reality. 20 Appendix A: Strategies and Activities Access to Care Healthcare Access Expand access to high quality and affordable health promotion and disease prevention healthcare. o Expand access to health insurance coverage and maximize opportunities presented by the implementation of the Affordable Care Act (health care reform). o Develop high quality patient centered medical homes for all. Promote an integrated health perspective to include the whole individual. Develop community members’ health literacy and capacity to navigate the healthcare system. Research patient activation strategies and utilize findings in creation of health promotion materials. Create interactive obesity prevention program for youth with disabilities and their parents. Disseminate via IOD website and NH Family Voices online training center. Create and disseminate inclusion tips and facts for tobacco cessation and prevention programs and providers. Assist state public health programs and initiatives (including obesity prevention, tobacco cessation, emergency management, breast & cervical cancer screening) to develop strategies and protocols to target and include people with disabilities. Distribute CDC Right to Know (breast cancer screening) campaign materials to all partners in Let No Woman Be Overlooked program. Conduct accessibility assessments of built environment at Community Health Centers and provide customized feedback and offers of technical assistance. Advertise on the project website which centers have participated in the assessment process. 21 Cultural Competence Support efforts to improve providers’ capacity to serve populations with disabilities. o Require training on cultural competence on populations with disabilities and on all forms of discrimination as part of training, licensure, and continued credentialing of all health professionals. o Promote culture change within healthcare organizations to improve the delivery of culturally responsive care. Improve the education that providers receive on establishing patient-centered, culturally responsive practices. Develop curriculum and deliver Responsive Practice train-the-trainer model to Community Health Care centers across the state. Develop curriculum and deliver training to mammography technicians in responsive practice techniques for different types of disability. Communication Ensure and/or expand access to ASL interpreters, augmentative and alternative communication, and medical information in alternate formats. Advocate for funding streams tied to appropriate preventive healthcare for populations with disabilities. o Support efforts to improve organizations’ capacity to serve this population. 22 Environments Where We Live, Learn, Work and Play Built Environment Increase access to physical activity and recreation, access to healthy foods, and safety in neighborhoods in which populations with disabilities live, learn, work and play. o Assist residents with disabilities in securing housing in safe and accessible neighborhoods. Expand accessible transportation alternatives and improve use of existing options. Social Inclusion Support initiatives that encourage populations with disabilities to build networks. o Encourage networking and community building for individuals with disabilities to address issues of isolation. o Encourage networking and community building between individuals with disabilities and the general population to foster integration. Education and Workforce Development Improve early childhood development and school-based programs’ cultural effectiveness. o Integrate culturally competent programming into early childhood development and school-based programs to improve integration for populations with disabilities and their families. Expand accessibility and effectiveness of education and training opportunities for people with disabilities. o Reach out to and include residents with disabilities in education and training opportunities including post-secondary education and vocational training programs. Encourage employers and labor unions to dedicate resources to recruitment, training and retention of people with disabilities for staff and leadership positions. 23 Awareness and Promotion of Health Equity Education and Outreach Educate and involve partners outside the health sector who impact where we live, learn, work and play in improving health promotion and disease prevention for populations with disabilities. o Develop materials and approaches to educate professionals, leaders and decision-makers about the social determinants of health, health equity, cultural competence and disabilities. o Encourage collaborations with new partners who influence community-level factors and systems that impact health. Incorporate concepts of civic and social responsibility in health and equity discourse. Create Policy Surveillance System with Michelle Winchester to monitor legislative sessions and produce timely fact sheets and educative policy briefs. Disseminate to targeted audiences within legislature and make available electronically to the public. 24 Funding Identify and pursue funding opportunities to support the priorities of this plan. o Coordinate funding initiatives across sectors to focus efforts and avoid duplication, and to address health promotion and disease prevention inequities for population with disabilities, as well as social determinants system-wide. Annually assess standing health committees for inclusion of people with for Encourage public, privatepublic and nonprofit organizations to prioritize and budget disabilities. health equity. o Examine current operations and budgets to seek ways to promote health equity within existing, routine activities. o When distributing funding throughout the state, require applicants to demonstrate their commitment to health and equity in their response to RFPs. Infrastructure and Policy Build and maintain a collaborative public-private partnership structure to implement the plan. Influence and create public policy that supports health and equity. 25 Data Guidelines and Systems Establish NH DHHS guidelines and policy for the collection of disability related data as a model for other organizations and state agencies. o Collaborate with stakeholders to define a list of relevant data fields for the state and develop a system for periodic updates. Dedicate resources for electronic data system improvements and quality assurance. Training and Education Train collectors and submitters of disabilities related data to use NH DHHS policy. o Create a forum for providers and data stewards to communicate and understand the importance of disabilities data collection. Educate the public about the collection of disabilities related data. Data Use Work with data stewards to stratify their data to identify health disparities experienced by people with disabilities. Monitor and report on health care utilization and the health status of people with disabilities. Conduct statewide needs assessment / annual disability and health report. Disseminate widely to stakeholders, including legislators and policymakers, and the public. Identify data sources for inclusion in statewide disability and health reports. Promote inclusion of disability identifiers on strategic sources of public health data (state-level surveillance, administrative forms, etc). Annually report rates of preventive services and screenings among people with disabilities. Conduct sessions at the annual AHEC conference (or other statewide events) to educate on disability and public health data. 26 Emergency Planning and Response Planning Provide technical assistance and model plans to local emergency management directors; regional public health emergency planners to facilitate complementary planning in accordance with the ADA. Ensure the State of NH Emergency Operations Plan respects the equal liberty, autonomy and dignity of all persons across all Emergency Support Functions as appropriate. Provide technical assistance and model plans, including Continuity of Operations Plans, to private agencies and businesses supporting individuals with disabilities. Foster engagement of individuals with disabilities in local, regional, and state-level emergency planning and exercises. Increase the number of individuals and families that are personally prepared for emergencies to the greatest extent possible. DCPG will review state’s Emergency Ops Plan, Functional Needs and Support Services Annex to ensure that it is appropriate for people with a broad range of disabilities. Resources are available on project website and via IOD statewide trainings re planning and making EP kits for people with disabilities. Train-the-trainer curriculum is being developed for Emergency Response personnel to acquire cultural competence with disability, so they can train populations with disabilities about the importance EP plans and kits and how to develop them. Present sessions at the annual NH EP Conference about project activities and information for planners. Work with Public Health Networks to ensure a disability contact for each region to help recruit and include people with disabilities for exercises, trainings, and workshops. Help to determine baseline levels of people with disabilities and their caregivers who have EP kits and plans or know of tools to create them. Provide technical assistance to Public Health Network coordinators about inclusion of people with disabilities in EP messaging and communication. 27 Response Improve the ability to share information between state and local emergency responders about the location and needs of individuals with disabilities. Activate health, medical and shelter facilities during emergencies that meet ADA requirements and are staffed by well-trained staff and volunteers who can address the needs of individuals with disabilities. Integrate disabilities service providers into local and regional systems that provide situational awareness during emergencies. Support disabilities service providers’ capacity to continue to provide services during emergencies. Provide feedback to state re volunteer assessments of emergency shelter facilities. Offer technical assistance with next steps. Provide technical assistance to Public Health Network coordinators re results of a needs assessment to determine their readiness to respond to the needs of people with disabilities in the event of an emergency. Recovery Ensure access among individuals with disabilities and their services providers to federal and state recovery programs, including financial assistance, following emergencies. Ensure that disabilities services providers are included in local and statewide recovery planning to restore services, facilities, and infrastructure within the public health, health care delivery, and human services sectors. 28