SMS FOR LIFE (A): A PUBLIC-PRIVATE COLLABORATION MALARIA DRUGS IN AFRICA
advertisement

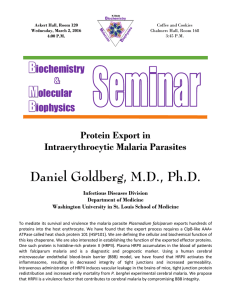
IMD-3-2168 v.03.09.2012 SMS FOR LIFE (A): A PUBLIC-PRIVATE COLLABORATION TO PREVENT STOCK-OUTS OF LIFE-SAVING MALARIA DRUGS IN AFRICA Research Associate Anna Moncef prepared this case under the supervision of Professor Donald A. Marchand as a basis for class discussion rather than to illustrate either effective or ineffective handling of a business situation. Every 30 seconds a child dies of malaria. Over 40% of the world’s children live in countries in which malaria is endemic. Each year, approximately 300 to 500 million malaria infections cause about one million deaths, most of them African children under the age of five. Increasing resistance to anti-malarial drugs, coupled with widespread poverty, weak health infrastructure and, in some countries, civil unrest mean that mortality from malaria in Africa continues to rise. The tragedy is that the vast majority of these deaths are preventable. The main reason why malaria is still such a threat, despite the existence of drugs to cure the disease, is a supply chain problem. Supply does not meet the demand where it occurs, and stock-outs of drugs to treat malaria cost lives. Jim Barrington, former chief information officer (CIO) at Novartis and current director of the SMS for Life project, had been trying to solve the problem since 2006, when he first heard about the “last mile” problem from Silvio Gabriel, executive vice president (EVP), Novartis Malaria Initiatives. At the end of 2008 Jim decided to commit 100% of his time and effort to an initiative to solve the supply chain problem and, after receiving the green light from Novartis to leave his current job as CIO, embarked on this new adventure. By January 19, 2009, he was sitting alone in an empty office, with only his computer, a phone and a solitary desk and chair. It was a few days after a US Airways pilot had successfully landed his plane in the Hudson River after birds flew into the engines. Jim described his thoughts at the time: I was tremendously motivated. I was excited. I felt inside that this was a problem I could solve. I thought about the pilot, who did such a fantastic job landing that plane in the Hudson River and I remember him saying afterwards that he felt his whole life, everything he did, all his training, was preparing him for this one moment. I can really relate to that, and I felt that this project was something that would allow me to utilize all the skills, training and experiences I had gained from 40 years in IT. If I could apply all those learnings to solve this one problem, this would be just magic. Copyright © 2010 by IMD, Lausanne, Switzerland (www.imd.org). No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means without the permission of IMD. -2- IMD-3-2168 Malaria as a Disease Malaria is a mosquito-borne infectious disease caused by the plasmodium parasite. The species Plasmodium falciparum is the most common cause of infection and is responsible for about 80% of all cases of malaria, and about 90% of deaths. Malaria is a public health problem in over 100 countries worldwide, inhabited by over 2 billion people. It occurs in tropical and subtropical regions, including parts of the Americas, Asia and Africa. About 85% of the 300 to 500 million cases annually occur in Africa, over 50% of them in five countries: Nigeria, Democratic Republic of the Congo, Ethiopia, Tanzania and Kenya.1 The African region accounts for 90% of malaria deaths globally, of which 85% of deaths are of children under five, especially in remote rural areas with poor access to health services. Causes and Symptoms Malaria is transmitted to humans by the bite of an infected female Anopheles mosquito, which injects the parasites into the bloodstream.2 The parasites travel to the liver, where they grow for six to nine days. They then leave the liver and invade red blood cells, where they multiply rapidly until the cells burst, releasing thousands of parasites into the bloodstream, which then attack other red blood cells, and the cycle continues. It takes between 7 and 21 days for symptoms to appear. These include waves of fever (when the blood cells are attacked), followed by shivering (when the blood cells burst), plus other symptoms such as sweating, headache, joint pain, vomiting, anemia and convulsions. If not treated within 24 hours, P. falciparum malaria can progress extremely rapidly and cause death within days or even hours. Overall fatality rates in endemic areas can be as high as 10% of all malaria cases. Young children and pregnant women are especially vulnerable. Malaria is a major cause of anemia in children and pregnant women, of low birth weight, premature births and infant mortality. Infants and children who have suffered from severe malaria may also develop mental impairments and even brain damage. Economic Burden Malaria is a disease that primarily affects the poor, but it is also a cause of poverty and a major hindrance to economic development. The gap in prosperity between countries with and without malaria has become wider every year.3 The economic impact of malaria has been estimated to cost Africa US$12 billion each year. This includes the cost of health care and medication, publicly managed mosquito control, 1 The WHO World Malaria Report 2008, http://www.who.int/malaria/publications/atoz/9789241563697/en/index.html 2 A mosquito becomes infected by biting an infected person and sucking up some blood containing malaria parasites, which undergo further development before being passed on when the mosquito feeds. 3 Sachs, J. and P. Malaney. “The Economic and Social Burden of Malaria.” Nature, 415, February 7, 2002. -3- IMD-3-2168 education and research, work and school days lost due to sickness, decreased productivity due to brain damage from cerebral malaria, and loss of investment and tourism.4 In some countries with a heavy malaria burden, the disease may account for as much as 40% of public health expenditure, 30% to 50% of hospital admissions, and up to 50% of outpatient hospital visits.5 The Fight against Malaria Although malaria is preventable and fully curable, it is a challenging task for African countries to control and eliminate it. In the last few years some progress has been achieved, with 9 countries in Africa and 29 elsewhere documenting reductions in malaria cases of more than 50% in 2008 compared with 2000. However, the number of cases fell least in countries with the highest incidence rates.6 Malaria Prevention Malaria can be prevented by the use of prophylactic, or preventative, drugs; by mosquito eradication through indoor spraying with insecticides; or by avoiding mosquito bites by using mosquito nets impregnated with insecticide. The first method is recommended to short-term visitors and travelers to countries where malaria is endemic. Intermittent preventative treatment is also recommended for pregnant women in areas of high transmission, where a single curative dose of an anti-malarial drug is administered at least twice during pregnancy. It is not practical and too expensive to be used for all full-time residents. Vaccines for malaria are currently under development, but no effective vaccine is yet available. Diagnosis and Treatment Malaria can be diagnosed by examining a patient’s blood under a microscope, but this is often not practicable in Africa, particularly in remote areas where there are no laboratories. Rapid diagnostic tests are a possible alternative. They are simple to use, require only a drop of blood and display results in a few minutes. The World Health Organization (WHO) recommends that malaria be confirmed by this type of diagnosis before treatment is given, but some countries that cannot afford rapid diagnostic tests often use symptoms as the indication to treat for malaria. The best available treatment for P. falciparum malaria – and the only one recommended by the WHO – is artemisinin-based combination therapy (ACT). It contains the basic compound 4 Greenwood B.M., K. Bojang, Ch.J.M. Whitty and A.T. Geoffrey. “Malaria.” The Lancet, Vol. 365, Iss. 9469. 5 6 http://www.rollbackmalaria.org/cmc_upload/0/000/015/363/RBMInfosheet_10.pdf WHO World Malaria Report 2009, http://www.who.int/malaria/world_malaria_report_2009/en/index.html -4- IMD-3-2168 artemisinin, which is isolated from a herb used in Chinese traditional medicine, before being chemically modified and combined with other drugs, for example lumefantrine. ACT is very effective when used within 24 hours of symptoms occurring. The WHO explicitly discourages the use of artemisinin by itself as a monotherapy as there are signs that malarial parasites are developing resistance to the drug, which makes the highly effective artemisinin derivatives and their partner drugs vulnerable to the same risk, endangering future malaria control. Drug Producers The pharmaceutical company Novartis, based in Basel, Switzerland, was the major producer of ACTs in the world. In 2001 the company began a program to produce and distribute a treatment called Coartem without earning any profit on these costs. By 2010 the company had produced and distributed over 320 million doses. To ensure a dependable supply and meet rising demand for Coartem, Novartis invested heavily to expand production in China and the United States, scaling capacity up to 100 million treatments annually. Since 2001, production efficiency gains enabled Novartis to halve the price per treatment, greatly increasing patients’ access to the drug. Novartis supplied Coartem in color-coded packages with doses to suit different ages. In 2008 the company developed Coartem Dispersible, a cherry-flavored sweet formulation of Coartem for children, which dissolved easily in a small amount of water. It eased administration and helped ensure effective compliance. Coartem Dispersible was the result of a public-private partnership between Novartis and Medicines for Malaria Venture, a nonprofit foundation dedicated to the development of affordable new anti-malarials.7 Institutions and Funding Committed to Eradicating Malaria The key institution in the fight against malaria was the Roll Back Malaria (RBM) Partnership,8 founded in 1998 by the WHO, the United Nations Development Programme, the United Nations Children’s Fund and the World Bank, in an effort to provide a coordinated global response to the disease. It has since become a global movement of more than 500 partners organized in eight constituencies: malaria endemic countries, multilateral development partners, the private sector, foundations, ex officio members, non-governmental and community-based organizations, research and academic institutions, and OECD donor countries. It forged consensus between key actors in malaria control, harmonized action and mobilized resources to fight malaria in endemic countries. The RBM Partnership together with the World Health Assembly, the decision making body of the WHO, established goals to reduce the number of malaria cases and deaths recorded in 2000 by 50% or more by the end of 2010, and by 75% or more by 2015. These were further emphasized in the Global Malaria Action Plan launched by RBM in September 2008, which defined the necessary steps to accelerate achievement of these targets. Two other very 7 http://www.corporatecitizenship.novartis.com/patients/access-medicines/access-inpractice/malaria.shtml 8 http://www.rollbackmalaria.org/docs/AMD/RBM_Background.doc -5- IMD-3-2168 important targets were outlined in the Abuja Declaration,9 committing African governments to an intensive effort to halve the burden of malaria in Africa by 2010, and the United Nations Millennium Goals.10 Goal no 6 was about combating HIV/AIDS, malaria and other diseases and one of its targets was to have halted by 2015 and begun to reverse the incidence of malaria and other major diseases. Another important organization in the fight against malaria was the Global Fund,11 a public/private partnership created in 2002 and dedicated to attracting and distributing financial resources to prevent and treat HIV/AIDS, tuberculosis and malaria. This partnership between governments, civil society, the private sector and affected communities represented a new approach to international health financing. The Global Fund worked in close collaboration with other bilateral and multilateral organizations to supplement existing efforts dealing with the three diseases. It provided three quarters of all international funding for malaria, with an allocation of $1.8 billion over the next five years. Every year a round of funding was conducted and grants were awarded to countries based on the assessment of the programs requesting support. In 2010, the 10th round of funding opened for applications. The funding came from about 50 donor governments and private sector donors, for example the Bill & Melinda Gates Foundation. Despite the increased funding from international sources (from $0.3 billion in 2003 to $1.7 billion in 2009) there still was a major gap.12 The estimated global requirement to eradicate malaria by 2015 was about $3.2 billion a year. Exploring the Problem at Novartis In June 2006 Silvio Gabriel, EVP, Novartis Malaria Initiatives, spoke at an internal Novartis IT conference in Basel designed to bring Novartis IT employees closer to the company’s patients. He talked about the problem of malaria and the existence of Coartem, which cured over 95% of cases after only three days of therapy. At the same time he mentioned the death statistics in Africa and the huge problem of matching patients with the pills. The in-country supply chain did not work very well, and there were many stock-outs in rural health facilities, where patients received free drugs, as opposed to having to pay for them from pharmacies or private clinics. African countries found it difficult to accurately forecast the usage levels of the drug, which resulted in Novartis receiving a lot of emergency orders. This meant it had to ramp up production and ship everything by air in order to meet this sudden demand. The pharmaceutical company could not hold too much stock of Coartem because it guaranteed that when the drugs were delivered they would still have a shelf-life of at least 18 months, out of the original 24 months. As CIO, Jim Barrington, participated in the conference and thought that IT could help solve the supply chain problem. He thought it would be a good challenge for his team to take on and asked René Ziegler, head of Global IT Governance and Operations, to go to Zambia, 9 http://www.rbm.who.int/docs/abuja_declaration_final.htm 10 http://www.undp.org/mdg/basics.shtml 11 http://www.theglobalfund.org/en/about/ 12 The WHO World Malaria Report 2009, http://www.who.int/malaria/world_malaria_report_2009/en/index.html -6- IMD-3-2168 where Novartis had been supplying Coartem to the public sector since 2001, to explore the situation. René met with the Zambian Ministry of Health and visited medical stores, hospitals, dispensaries and the like. He looked at the healthcare system, in particular at the processes for drug distribution, consumption reporting and needs forecasting, as well as the available technology and telecommunications. He discovered that the stock-out problem was huge, there was no consistent forecasting and consumption reporting in place, and ordering was paper based and sporadic. He produced a report with his main findings which highlighted two main problems. First, the information and communications infrastructure was still very poor – especially in rural areas – computers were not readily available, there were frequent power cuts, and the mobile phone coverage was not sufficient at that time but it was growing very fast. Second, Novartis could not assume responsibility for the in-country distribution of Coartem, since this was the primary responsibility of the Ministry of Public Health in each country. They concluded that there were no practical solutions to these issues. Defining the Solution In March 2008 Jim found another opportunity to explore the issue further, in an IMD/Novartis executive development program called IT Excellence (ITX). Silvio once again made an inspiring presentation to the participants. Several of them were so moved by the story that they formed a voluntary project team (ITX team), headed by Cathy Hein, senior project manager, to tackle the problem. Cathy recalled: A personal belief in the impact we could make as a whole to save lives was more than enough motivation to be persistent in overcoming all hurdles. It was particularly rewarding to know we were contributing to the fight against malaria. They went back to their home countries and continued working on the project remotely. Because they all had other work commitments their resources and time for the project were limited. At around this time, René and Jim made a presentation to Silvio, recommending that the SMS13 cell phone technology was the only viable IT solution for the rugged African environment. René then spoke with Jim about asking for help from IBM, Novartis’s major outsourcing partner, and specifically from the Value Creation Centre, a joint Novartis and IBM activity to drive innovation with IT in the pharmaceutical company. They contacted Charlotte Newton, chief innovation officer at the Value Creation Centre, and Jörg Sprengel, Global IBM R&D Client Manager on the Novartis Account. Charlotte was convinced about the project: Corporate responsibility projects carry something indefinably motivating to allow people to reach into their own self and to make a contribution that they are truly aligned behind. And this was the case with this project, where you are essentially saving babies’ lives. 13 SMS = Short Messaging Service, text message. -7- IMD-3-2168 The IBM team proposed using the Extreme Blue method, which it had used successfully for 10 years to help explore problems and find solutions. The program enlisted the help of students, who were valued for their fresh thinking, which was uncontaminated by the “corporate way” of solving problems. Jim and Silvio agreed to act as sponsors and to share the expenses and finance the students from their departmental budgets; IBM agreed to provide people to lead the project. There was no time to lose. It was already May 2008 and they had to find and hire eight students for a summer internship. Charlotte and Jörg started recruiting immediately. From 66 candidates, they chose a diverse team of 4 undergraduates and 4 graduates, 4 male and 4 female, from various backgrounds and nationalities; 3 of them had had malaria. On July 1, 2008, they kicked off the 12-week project with the sponsors and the ITX team. They started by mapping the existing supply chain, in particular “the last mile” problem (refer to Exhibit 1), and investigated possible improvements to the Coartem in-country supply chain in Nigeria and Tanzania. Typically, once stocks of drugs arrived in the country by airplane from abroad, they were transported in trucks to a central medical store (MSD in the exhibit). From there they went to zonal medical stores, then district warehouses and, finally, health facilities or health posts, which each served a large number of villages. Distances were great and the poor condition of some roads and climate complicated matters. At each step in the chain there was a lack of information flow. Coached and facilitated by Charlotte and Jörg, the students brainstormed 142 ideas, reduced them to 80, refined 42 of them and produced 10 possible solutions, which were combined into 5 final ones: SMS-based stock management, malaria schools initiative, a distribution coordination service, the year-out program, and community healthcare access. In September 2008 the students presented beautiful posters with drawings explaining the five proposed solutions in detail and their value assessment to Jim and Silvio, who chose SMSbased stock management as the preferred solution. The essential idea was to create an incounty forecasting system based on the use of SMS messaging between the health posts that dispensed Coartem and the district and regional warehouses that distributed the drug. A data management system with a reporting interface using charts would provide stock level information from all facilities to facilitate stock movement and supply, as well as improving stock forecasting and planning. Finding the Right Partners At the end of September the students went back to their universities and Jim continued thinking about how to move the project forward. By December 2008 he had decided to resign from the Group CIO position and his boss Raymond Breu, Novartis’s CFO, agreed to sponsor him for 12 months until his early retirement to focus solely on special projects. Jim recalled: Before this project, I had already made up my mind to resign from the CIO position for personal reasons. And the agreement with Raymond Breu was that I would be working on any special project he gave me. But this project was certainly at the back of my mind and one of the areas that I was going to target like crazy. And I persuaded him that I would like to progress it and see if I could make it happen. He didn’t really think I could: He was very skeptical; it required funding, it was highly political; and I would get caught up in bureaucracy, he thought. But he said: Fine, try it and we will see. Which I did. He gave me the approval in January and I purposely didn’t go near him again until I had everything in place. -8- IMD-3-2168 Enlisting the Roll Back Malaria Partnership In January 2009, in his new and empty office on the Novartis Basel campus, Jim set to work preparing what he called the “SMS for Life” project proposal to present to Professor Awa Marie Coll-Seck, executive director of the RBM Partnership. His idea was to establish a partnership project under the leadership of RBM in order to take ownership of the project away from Novartis and give him credibility and legitimacy when bringing other partners on board. When he presented to her and her team on February 10, 2009, they were quite excited about the project. They liked the fact that it tackled a major problem, and that both the problem and the potential solution were clearly defined. Finding Corporate Partners While waiting for RBM to commit, Jim started selling the idea to potential corporate partners based on the proposed project governance. The concept was that each selected partner would undertake to provide skilled resources and a financial contribution of approximately $200,000. This would provide a project team of five or six skilled people and an overall budget of $1 to $1.2 million. By the end of February 2009, Jim had secured the funding and resources from Novartis, a project manager and the use of LotusLive project management software from IBM, funding and advisor resources from Sara Lee, and initial interest from P&G. Sara Lee and P&G were both interested based on their logistics experience in African countries selling low-cost essential products like Kiwi Shoe Polish and soap. He still needed a mobile telecommunications company, an IT company to develop the system, and some type of visualization or mapping technology. He started talking to three companies: Zain, a mobile telecommunications company founded in Kuwait with operations in 17 African countries and 6 in the Middle East; Vodafone, the world’s largest14 multinational mobile telecommunications network company with operations in 31 countries; and Google, whose map service was of interest. Their responses and the ways these companies approached the potential cooperation were quite different. What was similar was that they all wanted to do everything by themselves, without other partners. Jim recalled: Google, which was by far the most enthusiastic, put six people on the project. I was sure they would be the most successful. After the initial contact I talked to them twice a week, but by April we still had nothing in writing. With Vodafone’s team we had an initial meeting in London with the director of intellectual property, the scientific director and the head of corporate research. After that they kept contacting me and disappearing for a while as they discussed the project internally. Zain kept quiet. He also started to look for a potential country in which to pilot the project. Two were on his list, Tanzania and Zambia, and he started to talk to their Ministries of Health. 14 Based on revenue. -9- IMD-3-2168 Setting up a Steering Committee In April, Professor Coll-Seck agreed to support the project and to chair the steering committee. Other members of the committee, from a broad range of backgrounds, were: Dr Alex Mwita, Tanzania National Malaria Control Program (NMCP) manager Dr Desmond Chavasse, PSI15 vice president and Global Malaria Control director Professor Marcel Tanner, director of the Swiss Tropical Institute Professor Klaus Leisinger, CEO of the Novartis Foundation for Sustainable Development Silvio Gabriel, EVP of Novartis Malaria Initiatives Jim Barrington, who became the “SMS for Life” program director. At the first steering committee meeting on April 20, 2009, Jim had to present the commitments from potential partners. By this time, he had received written confirmation from Vodafone that it would participate. It committed to cover all the costs of developing the software, for which it would hire an external software house, MatsSoft Ltd,16 as well as costs related to implementing the pilot, including providing handsets and covering the SMS costs. The other partners were not ready. Google was unable to obtain internal approval in time. Zain did not respond. Sara Lee withdrew its commitment after the financial crisis meant it had to cut funding of all non-essential activities. After many discussions with P&G, the company wrote back to say that it would not participate in the project. The initial concept of obtaining donations from a number of partner companies changed to having fewer partners, who each would finance their own parts of the project. They all agreed to fund their own travel costs and their people, eliminating the need for a central project budget. Getting Ready With the partners on board, the work on designing the system solution and preparing for the pilot began. In April, Jim hired Olympia Wereko-Brobby, one of the students who had taken part in the Extreme Blue process earlier in 2008, to help him coordinate the project. Other members of the team were three part-time project members from Novartis (Tara Cook, associate director, IT, sales & marketing US; Marty Putenis, executive director, healthcare compliance US; and Peter Buesch, head of IT project office Germany); Kevin Ferriday, project manager, from Vodafone; and Peter Ward, project manager, from IBM. 15 PSI provides malaria control support to national Ministries of Health in over 30 countries around the world, tailoring its programs to the environment in each location. 16 MatsSoft had previously worked with Vodafone on developing an SMS-based banking solution. - 10 - IMD-3-2168 Field Trips to Potential Pilot Countries The team started to refine the project scope, technical requirements and desired outcomes, as well as planning the project in detail. In May, they departed on a three-week field trip to Tanzania to meet with National Malaria Control Program (NMCP) representatives on the ground, including the manager Dr. Alex Mwita and the senior health officer Winfred Mwafongo. The NMCP would be the main owner and user of the SMS for Life solution in Tanzania. The team visited hospitals, health centers, dispensaries and warehouses in the three districts that the NMCP had chosen to participate in the pilot, namely Lindi Rural, Kigoma Rural and Ulanga (refer to Exhibit 2 for the location of the three districts). The three districts covered a population of over 1.2 million people in 226 villages and 129 health facilities. They were chosen because of their situation in three different regions that were representative of the country and supplied from different zonal medical stores; malaria was the most common cause of death there; and there were no other pilots running at the same time, which might have skewed the results. Thus, Lindi Rural represented an “average” district in Tanzania; Ulanga was one of the top 10 most difficult districts to work in, because of its remoteness and staff shortages and skill levels; and Kigoma Rural was so large that the zonal medical store was a one-day drive away from the main town, Kigoma, and the furthest health facility was a 12-hour boat trip away. The team explained the pilot to all stakeholders, showed them the draft solution and obtained their agreement to participate. They also met with a couple of NGOs17 that worked in Tanzania and understood the health system well, in order to benefit from their experience. Based on the inputs from all stakeholders, the team modified their project. The feedback received gave them a high degree of certainty that the designed solution would work. Once they were back in the UK, MatsSoft started to develop the system. At the beginning of June, Jim went to Zambia to discuss implementing the pilot there. Google representatives joined him on the trip to explore the possibility of doing the pilot in that country in place of Vodafone. They also met with a representative of Zain, which had temporarily regained interest in the project.18 After the trip, Google withdrew. Internal changes at google.org had led to a revised strategy and the reassessment of all projects in the pipeline, and the SMS for Life project no longer fulfilled the new selection criteria. In further discussions with the head of the NMCP in Zambia, it was agreed that Zambia did not need to run a separate pilot, as it could benefit from the Tanzanian results because the healthcare system organization in the two countries was very similar. Countdown to Launch Over the summer of 2009, the team focused all their efforts on getting ready to launch the pilot in Tanzania. They prepared training sessions for 157 health workers, in both English and Swahili, printed training materials including wall posters (refer to Exhibit 3), designed and ordered branded T-shirts with the logos of the RBM Partnership and the other partners. They 17 The Mennonite Economic Development Association (MEDA) and PSI Social Marketing & Communications for Health (PSI). 18 On June 8, 2010 Zain sold its operations in 15 African countries to the Indian company Bharti Airtel, keeping only those in Sudan and Morocco. - 11 - IMD-3-2168 also prepared a project website that was hosted on the RBM website. The SMS/mobile phone system, the Web-based reporting system and Google mapping were readied and tested. On August 5, the second steering committee meeting took place. It endorsed the start of the pilot in Tanzania, despite the fact that the memorandum of understanding with the Tanzanian Ministry of Health had not been signed. Piloting the Solution At the end of September 2009, the first training sessions took place. The training was tailored to three different user groups: (1) central management, including NMCP and MSD employees, (2) district management, including district management officers (DMO), district pharmacists and zonal MSD representatives, and (3) health facility workers, who were trained on how to store medicines, count stock levels, register their phones in the system and send the SMS messages (refer to Exhibit 4 for training details). The training included pharmacy best practices, which were well received by the health workers who had very little training. On October 1, the pilot was launched in the first district, Lindi Rural. Subsequently it was launched in Ulanga, on October 15, and Kigoma Rural, on October 22. The pilot ran for 21 weeks to cover two quarterly order and delivery cycles. How It Worked The solution consisted of two components: an SMS management application and a webbased reporting tool. All of the data was collected in a central system housed in the UK in the Vodafone MatsSoft data center. The SMS application stored the locations of the health facilities and the personal mobile phone numbers of the health workers, which were registered in the system to ensure that information was only sent by authorized workers. Every Thursday at 14:00 the system sent a weekly stock request message to all the registered mobile phones. The health facility workers had to count the level of stock in quinine injectables and four different dosages of Coartem and send back an SMS with the stock count message, as shown in Figure 1. In order to ensure maximum response rate, a free phone number was established and the costs were covered by the pilot. Figure 1: SMS stock levels and interpretation Y4: Coartem Yellow, for babies 5–15 kg: 4 boxes B3: Coartem Blue, for children 15–25 kg: 3 boxes R2: Coartem Red, for children 25–35 kg: 0 boxes G1: Coartem Green, for children above 35 kg and adults: 2 boxes Q99: Quinine injectables: 99 - 12 - IMD-3-2168 On Friday at 14:00, the SMS system sent an automatic reminder message to all health facility workers who had not yet responded. At 17:00, the system sent a credit of 1,500 Tanzanian shillings (the usual top-up amount in the area) to all mobile phones that had submitted a stock level SMS message. Late messages were accepted but no credit was awarded. The mobile phone credit was an incentive to motivate health workers to send the message on time and also to recognize the additional tasks they had to perform for the pilot above their normal workload. Because health workers were using their personal phones, the credit was for their personal use. Every Monday at 12 noon, the system sent an automatic message to the DMO indicating the health facilities that had not sent a message and the details of all health facilities with a stock-out. The web-based reporting tool enabled access to the data through a secure reporting website (refer to Exhibit 5), which was available via the internet or Blackberry mobile phones. It enabled the users, namely the NMCP district and central management employees, to view the current and historical stock levels at both the health facility and the district level. It displayed the facilities on Google maps, showed the SMS messages sending statistics, as well as any errors, and indicated the web-reporting usage statistics – e.g. how many times the web tool was accessed. Jim commented: One of our criteria was to design and build a solution that did the minimum necessary and was stripped of all complexity. We felt that this was necessary because in Africa it is quite difficult to work: remote locations, varying levels of education and literacy. We had to come up with something that is very simple. We designed a system that collects just five pieces of information every week in a very simple SMS message. Pilot Support and Monitoring Each DMO appointed one person to take the lead in driving corrective actions resulting from the stock level visibility. This person received a Blackberry device to access the system and was responsible for registering new users, educating them, assisting workers experiencing difficulties, and ordering and redistributing medicines in response to the stock-outs. An additional salary was paid to the district lead person for the duration of the pilot in recognition of the extra tasks he/she was asked to perform. The project team monitored the pilot in two ways. There was a daily review of the online information available through the web application. In addition, for the duration of the pilot, the team conducted surveillance visits to 116 out of the 129 pilot health facilities. There they registered physical stock counts and matched them against the most recent data entered in the SMS for Life application. They also checked the GPS positioning of the health facilities and provided answers to any questions the health workers had, as well as gathering their feedback. In total, the team spent over 370 man days on the ground supporting the pilot. These follow-up visits were very important for the health care workers’ perception of the project and its significance. Olympia recalled: To me, the most important part of the training was the visits we made to individual health facilities throughout the pilot. This process often involved long and difficult journeys to very remote areas, but the opportunity to catch up with people we had met at the centralized training, to experience their daily working environment and get their feedback on the project in an intimate setting, was amazing. They were also motivated by the visits and in having their feedback taken into account for the countrywide scale-up. I am sure this contributed to both the accuracy and the frequency of their SMS messages. The project is as much about the people you meet and learn from as it is about technology. - 13 - IMD-3-2168 On December 17, 2009, the third steering committee meeting took place, at which the pilot’s progress and initial results were discussed. The members also discussed handing over the pilot to the Ministry of Health and Social Welfare in 2010 and the possible implementation of the solution in other African countries. To do this, they agreed to organize meetings with the Global Fund, WHO and UNITAID. Pilot Results The pilot had three objectives: 1. To demonstrate that visibility of stock levels will prompt action to reduce stock-outs, thereby improving access to anti-malarial drugs. 2. To demonstrate that a data-gathering infrastructure can be made available via simple tools that can be used by people in the most remote locations. 3. To demonstrate the effectiveness of a public-private partnership model. By the time the pilot concluded at the end of February 2010, all three objectives had been fulfilled. The SMS for Life application provided, for the first time ever, reliable weekly stock information about anti-malarials in the health facilities. This enabled the district management to act upon the information and reduce or eliminate the stock-outs. At the beginning of the pilot, all three districts had high stock-out rates of one or more of the five drugs. During the pilot the stock-outs of all drugs were reduced from 57% to 0% in Lindi Rural, from 87% to 30% in Ulanga, and from 93% to 47% in Kigoma Rural (refer to Exhibit 6). At the beginning of the pilot, 26% of facilities had no stock of any dosage of Coartem; this figure was reduced to 0.8% by the end. The average response rate over the 21 weeks across all three pilot districts was 95%, never dropping below 93%. The data accuracy rate was 94%. The average usage of the system per user group was more than once per day. In the final report19 the team made a recommendation to implement the solution in all districts of Tanzania and other African or non-African countries to bring visibility to drug stock levels, which could be used for all priority drugs, depending on national environments. The solution could also be applied to disease surveillance and the public-private partnership model could be used to tackle other societal problems. The pilot results and recommendations were formally presented and the final report handed over to the Minister of Health, Professor David Mwakyusa, in Dar es Salaam on World Malaria Day,20 April 25, 2010. He said: If I only had that system before it would have made my life so much easier. I wanted to say: Thank you. 19 20 SMS for Life Tanzania Pilot Project Report World Malaria Day was declared in 2007 by the World Health Assembly after Africa Malaria Day, which was adopted in Abuja at the African Summit on Malaria in 2000. - 14 - IMD-3-2168 Dr. Alex Mwita, NMCP manager, commented: The SMS for Life project has demonstrated that it is possible to overcome the challenge of stock-outs by employing existing communications technologies. The use of mobile phones to inform about the stock position for anti-malarials has prompted the supply chain to replenish those medicines on time and thereby avoid stock-outs. The outcome has improved malaria treatment, patient satisfaction and, I have no doubt in my mind, has saved hundreds of lives in the districts where the pilot project was implemented. Looking Back The team wrote the following in their final report: The SMS for Life pilot created a unique public-private partnership model that enabled the problem to be precisely identified and a technical solution to be designed, built and implemented in three rural districts in Tanzania in about one year. In the end, no formal budget, legal contracts or memorandums of understanding were developed between any of the partners. The team working on the project was very lean but combined all the expertise, skills and influence necessary to tackle a complex problem. Each partner committed their unique resources and covered their associated project costs, eliminating the need to source and manage budgets on a project level. This model also made it easier, faster and more efficient to obtain results, bypassing the often lengthy and difficult approval process for project funding allocation and transfer. When asked about the rules of collaboration between the partners, Jim responded: The collaboration with them has been absolutely excellent; we managed to establish a team without the need for a contract, without the need for a budget, without any need for a formalized memorandum of understanding or agreements. The goodwill coming from those companies was amazing. And there are external partners that collaborated, for example British Airways gave a substantial discount on our air travel, which was a major cost in the project. He continued talking about their motivation to work for the project: The most important was to establish the emotional connection with what we were trying to achieve. All the people in MatsSoft, Vodafone and IBM, they know about malaria and they know that they are involved in a project that is directly contributing to saving people’s lives. That’s what drives us and keeps us all together. Post-pilot Strategies The pilot was successful, but Jim’s work did not stop there. Three issues had to be resolved: How to keep the pilot alive in the three districts and continue funding it for a “transitional” period? How to find support and financing for a full roll-out in Tanzania? How to approach a pan-African roll-out? - 15 - IMD-3-2168 Asked what he would do next, Jim replied: In the end the only single barrier is the funding. I believe that we can exercise tremendous power and influence through the donors such as the Global Fund, the WHO, UNICEF, the Bill and Melinda Gates Foundation. The donors are giving millions of dollars to buy the drugs and they would be very disheartened to hear that a country is running with a 76% stock-out rate and is happy to do so, and not make an intervention. So, I need to talk to the donors to make them aware of the potential to solve the stock-out problem with a small amount of funding. Maybe they would be prepared to divert some of the drug funding to managing the supply of drugs on the ground. - 16 - Exhibit 1 The Last Mile Problem Source: SMS for Life project team Exhibit 2 Map of Tanzania and the Three Pilot Districts Source: SMS for Life Tanzania Pilot Project Report, p. 8 IMD-3-2168 - 17 - Exhibit 3 Training Poster Source: SMS for Life project team IMD-3-2168 - 18 - Exhibit 4 Training of User Groups Source: SMS for Life Tanzania Pilot Project Report, p. 13 IMD-3-2168 - 19 - Exhibit 5 The Web-based View of the Information Reporting from the System Source: SMS for Life project team IMD-3-2168 - 20 - Exhibit 6 Pilot Results Source: SMS for Life Tanzania Pilot Project Report, p.28 IMD-3-2168