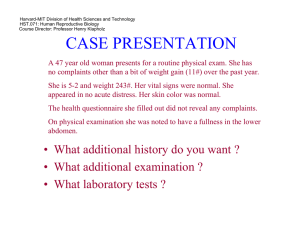
Harvard-MIT Division of Health Sciences and Technology HST.071: Human Reproductive Biology
advertisement

Harvard-MIT Division of Health Sciences and Technology HST.071: Human Reproductive Biology Course Director: Professor Henry Klapholz HST 071 IN SUMMARY FIBROIDS FIBROIDS • • • • • • • • Smooth muscle tumors of the uterus ,very common; Occur in more than one third of women over the age of 35 Complaints include discharge, bleeding from the vagina, pain, pressure Circumscribed - but not truly encapsulated Tumor can be readily "shelled out." - is glistening gray Composed of interdigitating bundles of smooth muscle. Incidence in black women three times greater than in white women. Strong hormonal relationship LOCATION • Intramural, subserosal, and submucosal • Subserosal and submucosal leiomyomas may become pedunculated • Submucosal leiomyomas most important - bleeding symptoms may occur • May occur in the cervix and broad ligaments as well • Few mitoses are present • Their spindle shape is readily apparent. • When the cells are cut across the nuclei appear round • Frequently undergo degeneration. - hyaline and cystic • Presence of large amounts of connective tissue - known as fibromyomas or "fibroids” • Bleeding symptoms caused in part by thinning of the overlying endometrium • Vessels are not capable of retracting in the usual manner • No basal zone from which the overlying thin layer of endometrium can regenerate • Submucous, pedunculated leiomyomas may prolapse • Necrosis in intramural leiomyomas - Only one artery supplies the leiomyoma • May calcify or undergo “red” degeneration ATYPICALITY • Atypicalities occur in leiomyomas - may be confused with leiomyosarcomas • Mitotic rate is characteristically less than 5 per 10 high-power fields • Intravascular leiomyoma - rare tumor -nodular masses of histologically benign smooth muscle growing within veins INCIDENCE & ETIOLOGY • Most common solid pelvic tumors in women • Clinically apparent in 20% to 25% of women during the reproductive years • Pathologic inspection of the uterus - present in more than 80% • Leiomyomas are clonal in origin o Classic paradigm – caused by and stimulated to grow by o Estrogen o Progesterone It is now clear that the following are responsible for fibroid growth o Transforming growth factor-s o Basic fibroblast growth factor o Somatic mutations of genes such as HMGI-C Fibroids are characterized by their location in the uterus o Subserosal leiomyomas o Intramural leiomyomas o Submucous leiomyomas • • • • • Few leiomyomas are actually of a single "pure" type Most leiomyomas are hybrids that span more than one anatomic location Increased incidence of leiomyomas in women of color Risk is increased in women with greater body mass index Decreased in women who smoke or who have given birth IN SUMMARY FIBROIDS • • • Good epidemiological evidence to suggest that use of oral contraceptive Birth control pills decreases the risk for leiomyomas 20% and 50% of women with leiomyomas have tumor-related symptoms • Fibroids often cause – Abnormal uterine bleeding Prolonged menstrual flow (menorrhagia) Submucous leiomyomas appear to be particular ly prone – Pelvic pressure. – Increase in uterine size – Pressure of particular myomas on adjacent structures Colon - constipation Bladder - urinary frequency. Ureters - hydronephrosis – Recurrent miscarriage – Infertility – Premature labor – Fetal malpresentation – Complications of labor HST 071 DIAGNOSIS • Easily determined by bimanual examination – Uterus is enlarged – Mobile – Irregular – Palpated abdominally above the symphysis • Ultrasonography most common method for diagnosis – Submucous fibroid can be missed on traditional ultrasonography • • • • • • • Magnetic resonance imaging (MRI) – Electron spin characteristics can often distinguish • Leiomyomas • Adenomyomas • Leiomyosarcomas Primary therapy for patients with large or symptomatic leiomyomas is surgery Hysterectomy is the most often United States: more than 175,000 hysterectomies are performed yearly for leiomyomas o Diagnosis of leiomyoma the most common indication for this procedure o Hysterectomy, the only true "cure" for leiomyoma, is a surgical option when women are no longer interested in future pregnancies Subtraction angiography o Easily visualize the fibroids and also embolize them in order to cause infarction o May dramatically reduce bleeding as well as size. Myomectomy o 18,000 myomectomies are performed yearly o Myomectomy diminishes menorrhagia in roughly 80% o Significant risk for recurrence of leiomyomas o Ultrasonography evidence of recurrence in 25% to 51% of patients o 10% require a second major operative procedure GnRH agonists (Lupron, Naferelin, Gosserelin) o Induce a hypo estrogenic pseudo menopausal state o Fibroids are dependent on estrogen for their development and growth o Hypo estrogenic state causes shrinkage o Uterine volume has been shown to decrease 40% to 60% after 3 months IN SUMMARY FIBROIDS HST 071 o Induces amenorrhea – increase iron stores and hemoglobin concentrations o Cessation of GnRH agonist treatment results in rapid re-growth o GnRH agonist treatment is useful as a pre-surgical treatment o Not a long-term treatment option • • • • • • • Androgenic agents – Danazol – Gestrinone Progestins – Medroxyprogesterone acetate (Provera) – Depo medroxyprogesterone acetate (Depo-Provera) – Norethindrone Do not consistently decrease uterine or fibroid volume Mechanism of action is thought to be the induction of endometrial atrophy Often not successful in controlling significant menorrhagia Somatic mutation is the initial event in most tumorigenesis Somatic mutations include a variety of chromosomal aberrations Point mutations or Chromosomal loss or gain. • Large chromosomal abnormalities such as translocations and deletions often detected with standard cytogenetic karyotypes • Independent monoclonal origin of individual myomas • Suggests somatic mutations offer a selective growth advantage to the mutated myocyte Variety of chromosomal rearrangements • Most common 12q14-15 and 7q22 • Heterogeneity of the cytogenetic abnormalities • Different somatic mutations may be involved in myoma tumorigenesis • Unique somatic mutations in individual myomas • Biologic basis for the differential responsiveness of individual myomas to a variety of growth-promoting agents SOME THOUGHTS ON THE DEVELOPMENT OF FIBROIDS • Clonal proliferation precedes the development of cytogenetic rearrangements o Somatic mutations which cannot be detected cytogenetically with the light microscope are the initial events in myoma tumorigenesis. o Explains the absence of cytogenetic abnormalities in a large proportion of myoma specimens. • ER alpha and ER beta mRNA expressed in leiomyoma and normal myometrium. • Expression of ER alpha higher than ER beta in both leiomyoma & myometrium • ER alpha expression is increased in leiomyoma compared to that the adjacent normal myometrium • ER beta expression is same or lower in leiomyoma than in the adjacent normal myometrium • Estrogen considered the major promoter of myoma growth • The long-term administration of a gonadotropin-releasing hormone (GnRH) agonist associated with both hypoestrogenemia and a reduction in myoma volume • Concentration of estradiol significantly higher in myomas than in normal myometrium. • Lower conversion of estradiol to estrone in myomas than myometrium. IN SUMMARY FIBROIDS HST 071 • Significantly increased concentration of estrogen receptors in myomas compared with autologous myometrium • Observations suggest intramyoma hormonal milieu is hyperestrogenic • No evidence that estrogen directly stimulates myoma growth • Mitogenic effects of estrogen are likely mediated by other factors and their receptors. • Several estrogen-regulated genes have been confirmed • Evidence to suggest that estrogen stimulates o progesterone receptor o epidermal growth factor o insulin-like growth factor-I • Regulation of myoma extracellular matrix • Estrogen directly stimulates collagen types I and III m-RNA • Stimulates expression of gap junction protein connexin-43 • Stimulates local production of the parathyroid hormone related peptide • Expression of these estrogen-regulated genes appears to be greater in uterine myomas than in the adjacent myometrium. • Hypersensitivity to estrogen may be important in the pathogenesis of myomas. • Ultrastructural features of cultured smooth muscle cells from uterine myomas and normal myometrium • Myoma and myometrial cells in estrogen and progesterone media more active under EM than cells in estrogen only medium. • Progesterone exposure -> increased number of myofilaments with dense bodies (suggesting that progesterone is involved in myoma differentiation) • Increased progesterone receptor m-RNA expression • Increased progesterone receptor protein levels in myoma tissue compared with adjacent myometrium FUNDAMENTAL QUESTIONS 1. What constitutes the female reproductive tract? 2. Discuss the histologic makeup of the uterus. 3. Where does the ureter lie with respect to the uterus and why is this important? 4. Describe the histology of the ovary. What cell lines are present? 5. What is a fibroid? 6. What hormones make fibroids grow? 7. Discuss the genetics of fibroids? 8. What are the clinical manifestations of fibroids? 9. How may fibroids be treated? IN SUMMARY FIBROIDS HST 071



![Fibroid Presentation [PPT]](http://s3.studylib.net/store/data/009527783_1-d7b94c2fba5c06a3eb93cab0950a79a7-300x300.png)