Post-Bariatric Patients in Substance Abuse Treatment:
Do they differ from the traditional substance abuse inpatient?
Ashley A. Wiedemann & Karen K. Saules
Eastern Michigan University
Introduction
Method
PROCEDURES:
A sample of PB (n=57) and NB (n=60) patients from a
comprehensive substance abuse treatment facility completed
a survey assessing demographics, and substance use (AUDITR). Diagnostic data and quantity of alcohol use were extracted
from electronic medical records (EMR) of all treatment
seekers from July 2009 through April 2011.
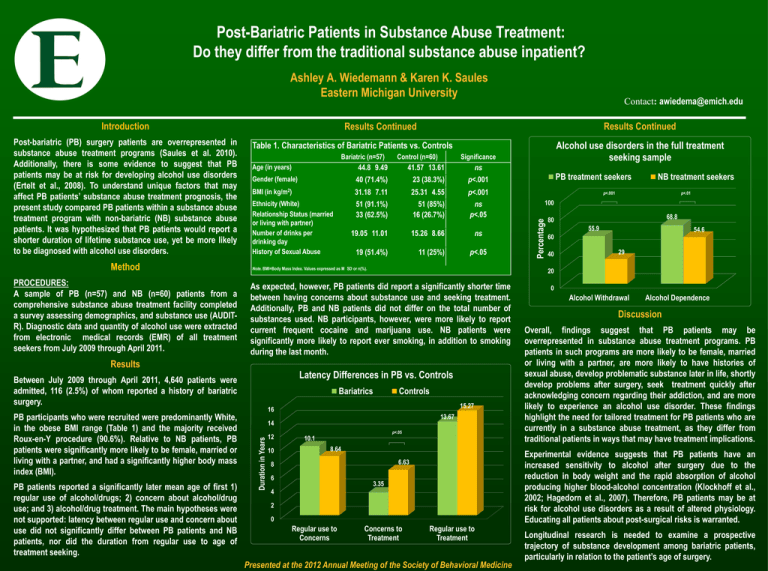
Bariatric (n=57)
Control (n=60)
Significance
Age (in years)
44.8 9.49
41.57 13.61
Gender (female)
40 (71.4%)
23 (38.3%)
p<.001
BMI (in kg/m2)
31.18 7.11
25.31 4.55
p<.001
Ethnicity (White)
Relationship Status (married
or living with partner)
Number of drinks per
drinking day
History of Sexual Abuse
51 (91.1%)
33 (62.5%)
51 (85%)
16 (26.7%)
ns
p<.05
19.05 11.01
15.26 8.66
19 (51.4%)
11 (25%)
ns
ns
p<.05
Note. BMI=Body Mass Index. Values expressed as M SD or n(%).
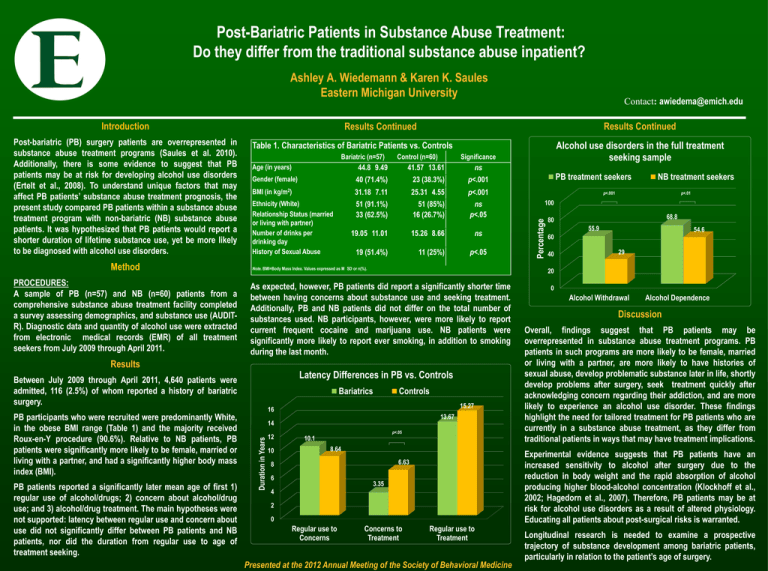
Latency Differences in PB vs. Controls
Bariatrics
Controls
15.27
16
13.67
Duration in Years
14
12
10
p<.05
10.1
8.64
6.63
8
6
3.35
4
2
0
Regular use to
Concerns
PB treatment seekers
NB treatment seekers
p<.001
p<.01
100
68.8
80
55.9
54.6
60
40
29
20
As expected, however, PB patients did report a significantly shorter time
between having concerns about substance use and seeking treatment.
Additionally, PB and NB patients did not differ on the total number of
substances used. NB participants, however, were more likely to report
current frequent cocaine and marijuana use. NB patients were
significantly more likely to report ever smoking, in addition to smoking
during the last month.
Between July 2009 through April 2011, 4,640 patients were
admitted, 116 (2.5%) of whom reported a history of bariatric
surgery.
PB patients reported a significantly later mean age of first 1)
regular use of alcohol/drugs; 2) concern about alcohol/drug
use; and 3) alcohol/drug treatment. The main hypotheses were
not supported: latency between regular use and concern about
use did not significantly differ between PB patients and NB
patients, nor did the duration from regular use to age of
treatment seeking.
Alcohol use disorders in the full treatment
seeking sample
Table 1. Characteristics of Bariatric Patients vs. Controls
Results
PB participants who were recruited were predominantly White,
in the obese BMI range (Table 1) and the majority received
Roux-en-Y procedure (90.6%). Relative to NB patients, PB
patients were significantly more likely to be female, married or
living with a partner, and had a significantly higher body mass
index (BMI).
Results Continued
Results Continued
Percentage
Post-bariatric (PB) surgery patients are overrepresented in
substance abuse treatment programs (Saules et al. 2010).
Additionally, there is some evidence to suggest that PB
patients may be at risk for developing alcohol use disorders
(Ertelt et al., 2008). To understand unique factors that may
affect PB patients’ substance abuse treatment prognosis, the
present study compared PB patients within a substance abuse
treatment program with non-bariatric (NB) substance abuse
patients. It was hypothesized that PB patients would report a
shorter duration of lifetime substance use, yet be more likely
to be diagnosed with alcohol use disorders.
Contact: awiedema@emich.edu
Concerns to
Treatment
Regular use to
Treatment
Presented at the 2012 Annual Meeting of the Society of Behavioral Medicine
0
Alcohol Withdrawal
Alcohol Dependence
Discussion
Overall, findings suggest that PB patients may be
overrepresented in substance abuse treatment programs. PB
patients in such programs are more likely to be female, married
or living with a partner, are more likely to have histories of
sexual abuse, develop problematic substance later in life, shortly
develop problems after surgery, seek treatment quickly after
acknowledging concern regarding their addiction, and are more
likely to experience an alcohol use disorder. These findings
highlight the need for tailored treatment for PB patients who are
currently in a substance abuse treatment, as they differ from
traditional patients in ways that may have treatment implications.
Experimental evidence suggests that PB patients have an
increased sensitivity to alcohol after surgery due to the
reduction in body weight and the rapid absorption of alcohol
producing higher blood-alcohol concentration (Klockhoff et al.,
2002; Hagedorn et al., 2007). Therefore, PB patients may be at
risk for alcohol use disorders as a result of altered physiology.
Educating all patients about post-surgical risks is warranted.
Longitudinal research is needed to examine a prospective
trajectory of substance development among bariatric patients,
particularly in relation to the patient’s age of surgery.
References
•Ertelt,
T. W., Mitchell, J. E., Lancaster, K., Crosby, R. D., Steffen, K. J., & Marino, J. M. (2008). Alcohol abuse and
dependence before and after bariatric surgery: A review of the literature and report of a new data set. Surgery for
Obesity and Related Diseases : Official Journal of the American Society for Bariatric Surgery, 4(5), 647-650.
•Hagedorn,
J. C., Encarnacion, B., Brat, G. A., & Morton, J. M. (2007). Does gastric bypass alter alcohol metabolism?
Surgery for Obesity and Related Diseases, 3, 543-548.
•Klockhoff,
H., Naslund, I., & Jones, A. W. (2002). Faster absorption of ethanol and higher peak concentration in women
after gastric bypass surgery. British Journal of Clinical Pharmacology, 54(6), 587-591.
•Saules,
K. K., Wiedemann, A. A., Ivezaj, V., Hopper, J. A., Foster-Hartsfield, J., & Schwarz, D. (2010). Bariatric surgery
history among substance abuse treatment patients: Prevalence and associated features. Surgery for Obesity
& Related Diseases, 6, 615-621.doi: 10.1016.jsoard.2009.12.008