Changes in concentrations of oxidised cytochrome oxidase
advertisement

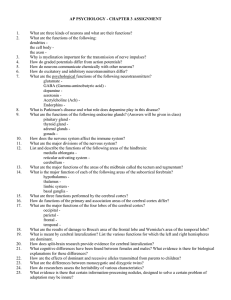
Changes in concentrations of oxidised cytochrome oxidase measured using both broadband and four wavelength near infrared spectroscopy reflect changes in oxygen delivery during hypoxaemia in healthy volunteers Martin Tisdall and Martin Smith Department of Neuroanaesthesia, The National Hospital for Neurology and Neurosurgery, Queen Square, London WC1N 3BG m.tisdall@ion.ucl.ac.uk Ilias Tachtsidis and Clare E. Elwell Department of Medical Physics and Bioengineering, University College London, Gower Street, London WC1E 6BT Abstract: Cranial broadband, and four wavelength, near infrared spectroscopy were used to measure changes in concentration of oxidised cytochrome oxidase in healthy volunteers during hypoxaemia. Significant changes, which reflect changes in cerebral oxygen delivery, are demonstrated. ©2006 Optical Society of America OCIS codes: (170.1610) Clinical Application; (170.1470) Blood/tissue constituent monitoring 1. Introduction Cytochrome c oxidase (CCO) is the terminal electron acceptor of the mitochondrial electron transfer pathway. It catalyses over 95% of the metabolism of oxygen and drives adenosine triphosphate synthesis. Changes in the redox state of CCO therefore reflect changes in cellular energy status. The absorption spectrum of oxidised–reduced CCO has a distinct band in the near infrared region which can be measured using near infrared spectroscopy (NIRS). Assuming that the concentration of CCO remains constant over the course of an experiment then changes in the NIRS CCO signal represent changes in the redox state of CCO. Oxy- (HbO2) and deoxyhaemoglobin (HHb) also have characteristic absorption spectra in the near infrared region (NIR) and NIRS can measure changes in the concentrations of these three optical chromophores using the modified Beer-Lambert law[1]. Changes in the total concentration of haemoglobin (Δ[HbT]=Δ[HbO2]+Δ[HHb]) and differential concentration of oxy- and deoxyhaemoglobin (Δ[Hbdiff]=Δ[HbO2]-Δ[HHb]) can then be calculated. The aim of this study was to measure changes in the concentration of cerebral oxidised cytochrome oxidase (Δ[ox-redCCO]) using both broadband and four wavelength near infrared spectroscopy systems during an isocapnoeic hypoxaemic challenge in healthy human adults. 2. Experimental Methods 14 healthy volunteers were studied following local ethics committee approval and written consent. 12 complete datasets were produced (9 male, 3 female, median age 30.5 years, range 26-36). NIRS optodes from a continuous wave, four wavelength spectrometer with a sampling rate of 6 Hz (NIRO 300, Hamamatsu Photonics KK) were placed on the forehead with channel 1 on the right and channel 2 on the left, and a detector emitter separation of 5 cm. The optodes from a broadband spectrometer (BBS) were placed high on the right side of the forehead with a detector emitter separation of 3.5 cm. Light from a tungsten halogen source was long pass filtered and transmitted to the head via a glass optic fibre bundle. Detected light was focused onto the slits of a 300 g/mm spectrograph grating (270M, Instruments SA), allowing collection of NIR spectra between 650 and 980 nm to a cooled charge coupled device detector (Wright Instruments, Enfield, UK) at a spectral resolution of ~5 nm. Data were collected at 1Hz. Non-invasive arterial oxygen saturation (SaO2) and blood pressure were collected from the left ear and left index finger respectively. Blood flow velocity in the right middle cerebral artery (vMCA) was measured continuously using transcranial Doppler ultrasonography and an anaesthetic machine delivered gas to the subject via mouthpiece. The study protocol consisted of initial period of five minutes baseline monitoring at normoxia and normocapnoea. The inspired oxygen concentration (FiO2) was reduced, by the addition of nitrogen, to induce a fall in SaO2 to 80%. The FiO2 was then returned to baseline for five minutes. This cycle was repeated three times and the study finished with a further period of baseline recording. End tidal partial pressure of carbon dioxide (EtCO2) was continuously fed back to subjects throughout the study and they were instructed to maintain normocapnoea. 3. Data Analysis Absolute changes in chromophore concentrations were calculated from changes in light attenuation and normalised to the baseline optical pathlength, calculated for the NIRO 300 data assuming a differential pathlength factor of 6.26[2], and measured for the BBS data using second differential analysis of the 740 nm water feature[3]. The start and end of each hypoxia was identified by manually finding the corresponding drop from, and return to, baseline of the FiO2. Mean changes for the three hypoxias from baseline to end of hypoxia, and baseline to end of recovery for each subject were compared using non-parametric ANOVA with post hoc pairwise comparisons. The group data were described by dividing the time course of the hypoxia and recovery periods into 16 epochs and calculating median change from baseline for each period. Changes in vMCA reflect changes in cerebral blood flow[4] and so, assuming constant arterial haemoglobin concentration over the course of the study, change in estimated oxygen delivery (ΔeDO2) is calculated as percentage change from baseline of SaO2*vMCA. 4. Results A 120 (%) 110 100 90 % ΔvMCA SaO2 80 0 -5 -10 -15 Δ[HbT] Δ[Hbdiff] -20 0 500 1000 Time (seconds) 1500 2000 0 C 25 0 -25 -50 Δ[ox-redCCO]*100 -75 500 1000 Time (seconds) 2000 5 0 -5 % ΔeDO2 Δ[Hbdiff] Δ[HbT] Δ[ox-redCCO]*100 -10 -15 0 500 1000 Time (seconds) 1500 2000 1 2 3 4 5 6 7 E 8 9 10 11 12 13 14 15 16 17 Epoch F 15 5 0 -5 % ΔeDO2 Δ[Hbdiff] Δ[HbT] Δ[ox-redCCO]*100 -10 -15 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Epoch Concentration (μM) ΔeDO2 (%) 10 Concentration (μM) ΔeDO2 (%) 1500 D 10 Concentration (μM) ΔeDO2 (%) 50 Chromophore concentration (μM) B 5 Chromophore concentration (μM) 130 10 5 0 -5 -10 -15 % ΔeDO2 Δ[Hbdiff] Δ[HbT] Δ[ox-redCCO]*100 -20 -25 -30 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Epoch Fig. 1. (A) SaO2 and % ΔvMCA data collected from single subject during repeated hypoxias. % ΔvMCA reveals cerebral vasodilatory response to hypoxia. (B) Δ[HbT] and Δ[Hbdiff], and (C) Δ[ox-redCCO] from same individual. Note overshoot in Δ[ox-redCCO] above baseline during recovery period. Group median ΔeDO2, Δ[Hbdiff], Δ[HbT] and Δ[oxredCCO] for (D) channel 1 and (E) channel 2 of the NIRO 300, and (F) the BBS against time period. Epoch 1 represents baseline, epoch 9 the nadir of hypoxaemia and epoch 17 the end of recovery. The group data are presented here as median (interquartile range). At the nadir of hypoxaemia, the reduction in SaO2 was 15.9(13.9-17.3) % and this corresponded with a reduction in eDO2 of 6 (3-10) % and an increase in heart rate of 14.7(10.6-15.5) beats per minute. The reduction in [ox-redCCO] was 0.12(0.07-0.17) μM for NIRO 300 channel 1, 0.05(0.04-0.10) μM for NIRO 300 channel 2 and 0.27(0.06-0.28) μM for the BBS. At this point, the changes in SaO2, eDO2, heart rate and the three measured Δ[ox-redCCO] values were statistically significant (p<0.05 for change from baseline). There were no significant changes in EtCO2 or mean blood pressure during the study. 5. Discussion This paper describes a significant reduction in [ox-redCCO] measured using two different NIRS systems during severe isocapnoeic hypoxaemia in healthy adult humans. The magnitude of the measured concentration change differed between both the two channels of the NIRO 300 (channel 1 -0.12 μM, channel 2 -0.05 μM), and the BBS (0.27 μM). This may be related to the exact positioning of the optodes on the head, the different inter-optode spacings used or the different pathlength corrections. Pathlength will vary depending on the optical properties of the interrogated tissue and the BBS system’s ability to directly calculate pathlength may therefore be beneficial. NIRS measured changes in [ox-redCCO] have been described in animals[5] and have been validated as a marker of cellular energy failure against magnetic resonance spectroscopy measured reduction in phosphocreatine levels[6],but using much more severe hypoxaemia than would be ethical in humans. Our previous work has described significant [oxredCCO] concentration changes of 0.1-0.5 μM associated with obstructive sleep apnoea in adults, where severe desaturations inducing drops in SaO2 down to 50-80% were observed[7], but to our knowledge this is the first description of the magnitude of [ox-redCCO] reduction during a reproducible and ethical hypoxaemia in healthy adults. Changes in the partial pressure of carbon dioxide have been shown to affect [ox-redCCO][8] and so to investigate the independent effect of hypoxaemia it is essential to maintain a constant EtCO2. This was achieved in our study by continuously feeding back the EtCO2 to the subjects and their voluntary control of minute ventilation. During the hypoxaemic phase eDO2 decreases, however cerebral vasodilatation also occurs and on returning the FiO2 to baseline the elevated cerebral blood flow causes a transient overshoot in eDO2. This hypoxaemic reduction in eDO2 is reflected by the Δ[ox-redCCO] in all three datasets and Δ[ox-redCCO] then returns to baseline during recovery. The eDO2 pattern during recovery is reflected by the Δ[ox-redCCO] BBS data, and the NIRO 300 channel 2 data also show Δ[ox-redCCO] occasionally increasing above zero during the hyperaemic recovery period. It has been suggested that changes in the optical properties of the brain caused by large changes in chromophore concentrations can lead to artefacts in the observed Δ[ox-redCCO][9]. The BBS data in particular suggest that, in this subject group, the CCO signal is able to measure an independent variable which reflects changes in cerebral DO2. We describe an ethical, repeatable adult protocol which appears to produce changes in [ox-redCCO], and provides an ideal model for further investigation of the CCO signal. This signal has potential as a clinical tool for assessing changes in cerebral cellular redox state after brain injury. 6. References 1. 2. 3. 4. 5. 6. 7. 8. 9. D. T. Delpy, M. Cope, "Quantification in tissue near-infrared spectroscopy", Philosophical Transactions of the Royal Society of London Series B-Biological Sciences 352, 649-659 (1997). A. Duncan, J.H. Meek, M. Clemence, C.E. Elwell, L. Tyszczuk, M. Cope, D.T. Delpy, "Optical pathlength measurements on adult head, calf and forearm and the head of the newborn infant using phase resolved optical spectroscopy", Physics in Medicine and Biology 295304 (1995). S.J. Matcher, M. Cope, D.T. Delpy, "Use of the water absorption spectrum to quantify tissue chromophore concentration changes in nearinfrared spectroscopy", Phys Med Biol 39, 177-196 (1994). J.M. Valdueza, J.O. Balzer, A. Villringer, T.J. Vogl, R. Kutter, K.M. Einhaupl, "Changes in blood flow velocity and diameter of the middle cerebral artery during hyperventilation: assessment with MR and transcranial Doppler sonography", Am J Neuroradiol 18, 19291934 (1997). C.E. Cooper, M. Cope, R. Springett, P.N. Amess, J. Penrice, L. Tyszczuk, S. Punwani, R. Ordidge, J. Wyatt, D.T. Delpy, "Use of mitochondrial inhibitors to demonstrate that cytochrome oxidase near-infrared spectroscopy can measure mitochondrial dysfunction noninvasively in the brain", J Cereb Blood Flow Metab 19, 27-38 (1999). R.J. Springett, M. Wylezinska, E.B. Cady, V. Hollis, M. Cope, D.T. Delpy, "The oxygen dependency of cerebral oxidative metabolism in the newborn piglet studied with 31P NMRS and NIRS", Adv Exp Med Biol 530, 555-563 (2003). I. Tachtsidis, C. Cooper, A.D. McGown, H. Makker, D.T. Delpy, C.E. Elwell, "Changes in total haemoglobin volume and cytochrome oxidase redox state during deep apnoeas in patients with obstructive sleep apnoea", in Biomedical Optics (Optical Society of America, Washington, D.C., 2000), WF6. A.D. Edwards, G.C. Brown, M. Cope, J.S. Wyatt, D.C. McCormick, S.C. Roth, D.T. Delpy, E.O. Reynolds, "Quantification of concentration changes in neonatal human cerebral oxidized cytochrome oxidase", J Appl Physiol 71, 1907-1913 (1991). K. Uludag, M. Kohl, J. Steinbrink, H. Obrig, A. Villringer, "Cross talk in the Lambert-Beer calculation for near-infrared wavelengths estimated by Monte Carlo simulations", J Biomed Opt 7, 51-59 (2002).