Early Exposure to Intimate Partner Violence and Infant Social-Emotional
advertisement

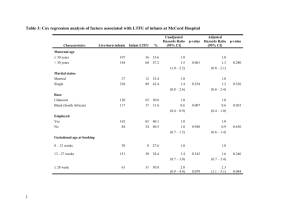
Early Exposure to Intimate Partner Violence and Infant Social-Emotional Development at 1 Year of Age: The Impact of Maternal Mental Health Sarah M. Ahlfs-Dunn, M.S., and Alissa C. Huth-Bocks, Ph.D. Eastern Michigan University INTRODUCTION METHOD PARTICIPANTS: A community sample of primarily low-income women (N = 120) participated in an interview at 1 year postpartum as part of an ongoing study on women’s transition to motherhood. The interview lasted approximately 2 ½ - 3 hours, and as part of a larger assessment battery, participants completed questionnaires regarding their experience of IPV during the last year, their mental health symptoms, and their infants’ social-emotional development. Participants were compensated with $50. Age: Mean = 26 (Range = 18 – 42, SD = 5.7) Race/ Ethnicity: 47% = African American, 37% = Caucasian, 11% = Biracial, 5% = Other Ethnic Groups Education: 20% = High School Diploma/ GED or less, 44% = Some College or Trade School, and 36% = College Degree Monthly Income: Median = $1,500 Relationship Status: 64% = Single, 28% = Married, 4% = Separated, 4% = Divorced First Time Mothers: 30% MEASURES: 1 – Intimate Partner Violence (IPV). The Conflict Tactics Scales-2 (CTS-2; Straus, Hamby & Warren, 2003) is a questionnaire designed to assess partner psychological, physical, and sexual violence, and injury resulting from partner violence during the last year. Presence or absence of IPV during the last year was used in this study. 2 – Maternal Depression. The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) is a 21-item selfreport instrument designed to assess the severity of depressive symptoms. Participants respond based on how they have been feeling for the past two weeks. Higher scores indicate greater severity of depressive symptoms. The presence of IPV during the infant’s first year of life was associated with more infant social-emotional problems at 1 year of age, r = .26, p < .01. The association between the presence of IPV during the first year of life and infant social-emotional problems at 1 year of age was moderated by maternal PTSD hyperarousal symptoms (β = .20, p < .05). There also was a main effect for maternal hyperarousal symptoms (β = .25, p < .01) . Post-hoc analyses revealed that there was a significant positive slope for high hyperarousal symptoms (β = .45, p < .01), but not for low hyperarousal symptoms (β = .07, p > .05). Interaction between Intimate Partner Violence and Maternal PTSD Hyperarousal Symptoms 0.8 .69 Infant Social-Emotional Problems A substantial amount of research has documented the detrimental effects of intimate partner violence (IPV) on children aged 3 and older; however, research examining the effects of IPV on infants is limited. Of the studies that have been conducted, researchers have found that infants who are exposed to IPV experience trauma symptoms (Bogat et al., 2006; Zeanah & Scheeringa, 1997), increased distress when exposed to adult conflict (DeJonghe et al., 2005), externalizing, internalizing, and atypical/maladaptive problems, and poorer emotional and physiological regulation (Crockenberg et al., 2007; McDonald et al., 2007; Porter et al., 2003). Furthermore, mothers’ mental health is significantly impacted by experiences of IPV (Bonomi et al., 2006; Roberts et al., 1998), and impaired maternal well-being may further exacerbate the impact of IPV exposure on infants. AIM: To investigate the impact of IPV exposure on 1-year-old infants’ social-emotional development as well as the impact of maternal mental health on this association. RESULTS 0.6 0.4 0.2 Absence Presence 0 -0.2 -0.4 This finding suggests that greater maternal hyperarousal symptoms exacerbate the effect of IPV exposure on infant social-emotional problems. High Hyperousal Symptoms β = .45, p < .01 -.20 -.19 -.33 Low Hyperarousal Symptoms β = .07, p > .05 -0.6 Intimate Partner Violence The association between the presence of IPV during the first year of life and infant social-emotional problems at 1 year of age was NOT moderated by maternal general anxiety (β = .13, p > .05), total maternal PTSD symptoms (β = .09, p > .05), or maternal depression (β = .15, p > .05). This suggests that it is particular maternal mental health disturbances that may exacerbate the impact of IPV on infants. DISCUSSION 4 – Maternal Post-Traumatic Stress Disorder (PTSD). The PTSD Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993) is a 17-item questionnaire designed to assess specific symptoms of PTSD, including avoidance, dysphoria, and hyperarousal. Participants respond based on how they have been feeling for the past month. Higher scores indicate greater severity of PTSD symptoms. These findings not only indicate the significant impact that exposure to IPV can have on infants’ social-emotional development, but they also indicate that certain maternal mental health symptoms (i.e., PTSD hyperarousal symptoms) may be particularly important. Maternal PTSD hyperarousal symptoms, in comparison to maternal general anxiety, total PTSD symptoms, and depression, may exacerbate the impact of IPV exposure on infants due to the nature of these symptoms. Mothers who evidence PTSD hyperarousal symptoms may startle easily, be jumpy, be very watchful or hypervigilant, be more irritable or prone to anger outbursts, and experience panic more often. Symptoms like these may lead a mother to over react to her infant’s normative behaviors and normative responses to IPV exposure as well as lead her to express an excessive amount of fear in response to daily experiences that then increase her infant’s overall fears and anxieties. Hyperarousal symptoms may also prevent a mother from being appropriately attuned with her infant and able to consistently respond sensitively to his/her biological and emotional needs, which may be intensified as a result of IPV exposure. 5 – Infant Social-Emotional Development. The Brief Infant-Toddler Social and Emotional Assessment (BITSEA; Briggs-Gowan & Carter, 2006) is a 42-item questionnaire designed to assess for social-emotional and behavior problems in young children. Participants respond based on their children’s behavior in the last month. Higher scores indicate more social-emotional problems. For clinicians who work with mothers and children who have experienced IPV, it is important to assess the mother’s mental health symptoms and assist her in obtaining services that appropriately address her symptoms. Appropriate treatment of maternal mental health symptoms, particularly PTSD hyperarousal symptoms, will help mothers to better respond to their infants’ needs; thereby, reducing the impact of IPV exposure on their infants. 3 – Maternal Anxiety . The Brief Symptom Inventory (BSI; Derogatis, 1993) is a 53-item self-report designed to assess general psychological symptoms. The 6 anxiety items were used in the present study. Participants respond based on how they have been feeling for the past week. Higher scores indicate greater severity of anxious symptoms.