covS EXPRESSION AND INNATE IMMUNE EVASION IN A HYPERVIRULENT STREPTOCOCCUS

THE EFFECT OF A NATURAL covS MUTATION ON VIRULENCE FACTOR
EXPRESSION AND INNATE IMMUNE EVASION IN A HYPERVIRULENT
STRAIN OF GROUP A STREPTOCOCCUS by
Zachary William Stetzner
A thesis submitted in partial fulfillment of the requirements for the degree of
Master of Science in
Immunology and Infectious Diseases
MONTANA STATE UNIVERSITY
Bozeman, Montana
November 2013
©COPYRIGHT by
Zachary William Stetzner
2013
All Rights Reserved
ii
APPROVAL of a thesis submitted by
Zachary William Stetzner
This thesis has been read by each member of the thesis committee and has been found to be satisfactory regarding content, English usage, format, citation, bibliographic style, and consistency and is ready for submission to The Graduate School.
Dr. Benfang Lei
Approved for the Department of Immunology and Infectious Diseases
Dr. Mark Quinn
Approved for The Graduate School
Dr. Ronald W. Larsen
iii
STATEMENT OF PERMISSION TO USE
In presenting this thesis in partial fulfillment of the requirements for a master’s degree at Montana State University, I agree that the Library shall make it available to borrowers under rules of the Library.
If I have indicated my intention to copyright this thesis by including a copyright notice page, copying is allowable only for scholarly purposes, consistent with “fair use” as prescribed in the U.S. Copyright Law. Requests for permission for extended quotation from or reproduction of this thesis in whole or in parts may be granted only by the copyright holder.
Zachary William Stetzner
November 2013
iv
ACKNOWLEDGEMENTS
I wish to express my gratitude to my mentor, Dr. Benfang Lei, for dedicating so much of his time to making me a better scientist. He has been a powerful motivator and his words of encouragement have been pivotal to my success in graduate school. I also wish to thank my graduate committee, Dr. Mark Quinn and Dr. Josh Obar for their guidance and feedback during the writing of my thesis. I wish to express my appreciation to all current and past members of the Lei lab including but not limited to Dr. Guanghui
Liu, Wenchao Feng, Tracey Hanks, Dr. Jim Wiley, Alix Herr, Dengfeng Li, Mengyao
Liu, Jinquan Li, and Yang Zhou; thank you all for making the lab an exceptional working environment. I am especially grateful to Dr. Guanghui Liu for teaching me everything I know about molecular cloning. Finally, to my family and friends, your support has meant everything and I wouldn’t have come this far without all of you.
v
TABLE OF CONTENTS
1. INTRODUCTION ...........................................................................................................1
Epidemiology of GAS .....................................................................................................1
Emm -Gene Serotyping.............................................................................................2
Pharyngeal GAS Disease .........................................................................................4
Invasive GAS Disease .............................................................................................5
Virulence Factors.............................................................................................................6
Hyaluronic Acid Capsule.........................................................................................7
Streptococcal Secreted Esterase...............................................................................8
SpyCEP/ScpC ..........................................................................................................8
Streptococcal Pyrogenic Toxin B (SpeB)................................................................9
Transcriptional Regulation of Virulence Factors.............................................................9
CovR/S Gene Regulation.......................................................................................10
CovR/S Mutations in Hypervirulent Strains..........................................................11
Project Objective....................................................................................................12
2. MATERIALS AND METHODS...................................................................................13
Bacterial Strains and Growth.........................................................................................13
Generation of MGAS315 sse Deletion Mutant..............................................................13
Generation of MGAS315 covS Deletion
Mutant and Replacement with MGAS2221 covS ..........................................................14
Generation of MGAS315 ropB Deletion
Mutant and Replacement with MGAS2221 ropB ..........................................................15
In trans Expression of the MGAS315 covS Gene in MGAS2221 Δ covS .......................17
Measurement of Esterase Production and Acetylhydrolase Activity ............................17
Mouse Infections............................................................................................................18
Quantification of Neutrophil Infiltration .......................................................................19
Quantitative RT-PCR Analysis......................................................................................20
SpeB Activity Assay......................................................................................................20
Statistical Analyses ........................................................................................................20
3. RESULTS ......................................................................................................................21
Hypervirulent MGAS315 has a High Capacity
to Invade Soft Tissue and Evade Innate Immunity........................................................21
A Critical Role for the Esterase SsE in Skin Invasion
and Innate Immune Evasion of MGAS315....................................................................24
Repairing the covS G1370T Mutation of MGAS315..........................................................25
457V Effects of the Replacement of CovS
in MGAS315 on Expression of Multiple Virulence Genes ...........................................30
vi
TABLE OF CONTENTS – CONTINUED
SpeB Activity is not Fully Dependent on CovS
Repairing of the CovS
G457V Mutation .....................................33
G457V Mutation Attenuates MGAS315
Skin Invasion, Innate Immune Evasion, and Virulence.................................................35
4. DISCUSSION................................................................................................................38
5. CONCLUSION..............................................................................................................42
REFERENCES CITED......................................................................................................46
vii
Table
LIST OF TABLES
Page
1. Gene expression patterns and SpeB production in
MGAS2221, MGAS315, and MGAS315 isogenic mutants ..............................43
viii
Figure
LIST OF FIGURES
Page
1. GAS has a variety of virulence factors that
contribute to disease pathogenesis .......................................................................7
2. MGAS315 is a hypervirulent isolate associated
with reduced neutrophil recruitment ..................................................................23
3. Esterase is required for virulence in MGAS315 ................................................25
4. Replacement of CovS G457V in MGAS315 with wild-type CovS .......................28
5. CovS G457V mutation in MGAS315 increases expression
of multiple virulence factors ..............................................................................32
6. SpeB activity is absent in MGAS315wt covS .....................................................34
7. MGAS315wt covS virulence is significantly attenuated in vivo .........................37
8. Model of the effect of covS and ropB mutations on MGAS315 infection ........45
ix
ABSTRACT
Group A Streptococcus (GAS) is a highly versatile pathogen that is able to colonize multiple locations on the body, resulting in numerous diseases such as mild pharyngitis and the potentially lethal necrotizing fasciitis (NF) and streptococcal toxic shock syndrome (STSS). The high mortality rates associated with severe invasive diseases are particularly concerning. GAS strains isolated from patients with severe invasive infections frequently display hypervirulence, but the basis for this hypervirulence is not fully understood. The objective of this project is to elucidate the underlying mechanism behind this hypervirulent phenotype in a serotype M3 STSS isolate, MGAS315. A comparative study of MGAS315 and a serotype M28 puerperal sepsis isolate, MGAS6180, revealed that MGAS315 has a substantially higher capacity to invade soft tissue and inhibit neutrophil recruitment than MGAS6180 in a murine model of subcutaneous infection. Deletion of the platelet-activating factor (PAF) acetylhydrolase gene sse reduced MGAS315 skin invasion and innate immune evasion.
These results cannot be explained by the proposal that the hypervirulence of MGAS315 is due to the acquisition of additional prophage-encoding virulence factors. SsE is negatively regulated by the two-component regulatory system CovR/S, and MGAS315 has a CovS G457V mutation compared with the covS gene of the serotype M1 isolate
MGAS2221. We hypothesize that the CovS G457V mutation is responsible for the hypervirulence of MGAS315. To test this hypothesis, the mutated covS gene in
MGAS315 was replaced with wild-type covS , resulting in MGAS315wt covS . The mRNA levels of CovR/S-controlled capsule synthase gene hasA and the IL-8 peptidase gene spyCEP in MGAS315wt covS were 24% and 3% of those in MGAS315, respectively. Repairing the covS mutation in MGAS315 also reduced the PAF acetylhydrolase activity in the culture supernatant and SsE production as measured by western blotting analysis. These results indicate that the CovS G457V mutation enhanced the expression of CovR/S-controlled virulence factors. More importantly, repairing the
CovS G457V mutation attenuated the innate immune evasion, skin evasion, and virulence during infection. Collectively, this work demonstrates the CovS G457V mutation increases virulence factor expression and enhances innate immune evasion, thereby contributing to the hypervirulence of MGAS315.
1
Group A Streptococcus
INTRODUCTION
(GAS; Streptococcus pyogenes ) is an extracellular, Grampositive bacterium responsible for a variety of diseases ranging from mild cases of pharyngitis and pyoderma to highly invasive necrotizing fasciitis and streptococcal toxic shock syndrome (STSS) 1 . GAS infection is also highlighted by post-streptococcal immune sequelae resulting in acute rheumatic fever and glomerulonephritis. The clinical impact is significant as GAS is exclusively a human pathogen and maintains a narrow ecological in a human reservoir. Fortunately, S. pyogenes has maintained susceptibility to penicillin likely do to the inability to express β -lactamase 2 . Still, even with effective antibiotics, GAS infections continue to plague a substantial proportion of the world’s population.
Epidemiology of GAS
Since the resurgence of severe GAS infections in the mid-1980s, there have been approximately 10,000 cases reported in the United States annually 3,4 . In 2005, approximately 18.1 million people suffered from severe GAS infection accounting for
517,000 deaths annually; however, this number is likely much higher as many GAS infections go unreported 5 . In addition to these severe cases, over 700 million cases of superficial and self-limiting infections such as pharyngitis and pyoderma occur each year further contributing to increases in health care costs 5 . The prevalence of GAS is attributable to several factors responsible for transmission. GAS is transmitted via direct skin contact, droplets from pharyngeal carriers, and contaminated fomites.
2
Overcrowding has a considerable impact on spread as many cases of GAS have been documented on military bases and crowded households in New Zealand have reported increases in rheumatic fever 6,7 .
Transmission of GAS and the disease manifestations tend to differ between urbanized and developing countries. Traditionally, in industrialized countries with temperate climates, GAS infections are most commonly associated with pharyngeal carriage and droplet spread 8 . In contrast, a disproportionately high rate of pyoderma
( ≥ 70% in children) has been observed in aboriginal communities of northern Australia, where up to 14 different strains of GAS may be circulating through an individual community at any one time 9,10 . Moreover, the prevalence of rheumatic heart disease is highest (5-7 cases/1000) in regions such as Sub-Saharan Africa where poor hygiene is common and access to medical treatment is limited 11 . However, the infrastructure needed to monitor and accurately classify differences in GAS disease is relatively uncommon in these developing countries suggesting these numbers may, in fact, be underestimates of the actual GAS burden. This disparity in disease between socioeconomic classes has led to increased surveillance of GAS to elucidate what molecular markers are associated with particular disease types and identify the populations most commonly associated with those GAS strains.
Emm -Gene Serotyping
While economic and environmental factors are indicators of specific cases of
GAS, they are certainly not the sole determinants. In order to effectively monitor the spread of GAS and identify the variations in disease both geographically and in body site
3 preference, epidemiologists began using the cell surface M-protein to track incidences of
GAS across the globe. More than 200 different emm -types have been documented and it is evident that GAS emm serotypes differ significantly between developing and developed countries 12,13 . In low-income regions such as India and Ethiopia, the diversity of circulating emm -types is high and no one emm -type appears to dominate 14,15 . In industrialized nations; however, a fewer number of circulating emm -types have been reported with even less dominant 16 . Only 25 emm -types accounted for 90% of the GAS isolates from urbanized countries 16 .
Differences in emm -types exist not only between geographic and socioeconomic regions but also in tissue tropism. This variation in emm -typing can be further classified based on emm chromosomal architecture or “ emm patterns” which have been shown to be strong biological markers of tissue site preference 17,18 . Emm patterns are based on the arrangement of emm and emm -like genes and have been shown to directly correlate with the emm -type of a specific GAS strain 17,19 . GAS can be categorized into three major patterns: A-C, D, and E. Pattern A-C isolates are commonly associated with throat colonization, pattern D strains correspond to isolates recovered from skin infections, and pattern E consists of individuals associated with both throat and skin sites 20 . Emm pattern A-C includes a wide range of GAS strains such as the “invasive” ( emm 1, 3, 12, and 18) and the “rheumatogenic” isolates ( emm 1, 2, 6, 12, 18, 28, 75, and 89) 3,21 .
It appears differences in emm type, pattern, and tissue preference play a pivotal role in GAS pathogenesis and disease presentation.
4
Pharyngeal GAS Disease
GAS is responsible for 15% to 36% of pharyngitis-related cases that occur each year in the United States resulting in a significant economic burden of approximately $2 billion annually in direct medical costs 22,23 . A major contributor to this pronounced number of pharyngeal GAS cases is the carrier state. During carriage, GAS poses no threat to the host; however, it serves as a critical reservoir for transmission through contact 24 . The carrier state further complicates the estimates of acute rheumatic fever
(ARF) and acute post-streptococcal glomerulonephritis (ASPGN) by misappropriating asymptotic carriers as possible infectious cases 25 .
Pharyngitis is a seemingly benign disease that subsequently leads to relatively mild illnesses such as scarlet fever but also results in more severe, life-threatening complications such as STSS and ARF. Scarlet fever is associated with illness in schoolaged children ranging from 5-12 years old and characterized by a red rash and strawberry tongue 26 . The streptococcal pyrogenic exotoxins or superantigens A, B, and C have been identified as the key factors of the disease 27 . Since the introduction of antibiotics, however, the disease is easily managed and has become less common. Rheumatic fever, on the other hand, is a particularly devastating illness responsible for irreversible heart damage. ARF, a nonsuppurative sequelae of pharyngitis, is estimated to affect 1 in 1,000 people with a significant proportion being children, adolescents, and young adults 11,28 .
During ARF pathogenesis, an autoimmune response is generated when cross-reactive antibodies to the GAS M protein also target cardiac myosin and heart valve glycoproteins 28 . In addition, the hyaluronic acid capsule of GAS which is also present in
5 the host extracellular matrix may produce an autoimmune response by activating B cells via cross-linking of the B cell receptors 29 .
Invasive GAS Disease
Invasive GAS infections such as necrotizing fasciitis (NF) and STSS display a rapid onset of severe symptoms including accelerated deterioration of tissue and systemic dissemination resulting in a high number of fatalities. From 1994-1995, 556 Swedish patients diagnosed with invasive GAS had a 16% mortality rate which rose to 37% among those identified with STSS 30 . In 1999, the United States reported 9,500 cases of invasive GAS contributing to 1,100 deaths 31 . These high mortality rates demonstrate the virulence of invasive GAS and the need for effective treatments to combat this manifestation of the pathogen.
Necrotizing fasciitis is a particularly devastating disease and is often deceptive in its presentation. NF often begins as a harmless skin lesion but progresses rapidly to a highly lethal disease. Invading GAS penetrates subcutaneous and deep soft tissue and spreads along the fascial planes of the muscle inducing a potent proinflammatory response 32 . The combination of GAS virulence factors and degradative host enzymes causes significant tissue damage as well as increased bacteremia and systemic dissemination 33 .
STSS can begin with infection at any site but is often associated with a preexisting skin lesion. Symptoms of STSS include pain which can be found in an extremity or the peritoneal cavity, fever, and localized swelling or erythema which is followed by shock and multiple organ failure a few hours later 34,35 . Superantigens of S. pyogenes
6 have been identified as the primary culprits responsible for STSS. These superantigens bind to the T-cell receptor and major histocompatibility complex class II (MHCII) simultaneously 36 . Subsequent activation of T-cells and antigen-presenting cells leads to production of dangerously high levels of cytokines such as tumor necrosis factor alpha
(TNFα ) and beta (TNFβ ), interleukin-1 (IL-1) and IL-2 36-38 . Streptococcal pyrogenic exotoxin (Spe) A and C as well as the streptococcal mitogenic exotoxin Z (SmeZ) have been reported to be involved in STSS 39-41 . The resurgence of invasive GAS infections is unsettling and, although, the probability of contracting NF and STSS is low, the mortality rates are high warranting further examination into the molecular mechanisms responsible for the severity of the disease.
Virulence Factors
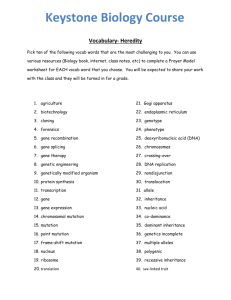
Several GAS virulence factors have been identified that are responsible for the severe pathogenesis of invasive GAS disease. These include but are not limited to: the hyaluronic acid capsule, M protein, streptococcal secreted esterase, streptococcal pyrogenic toxin B (SpeB), streptolysin S, DNases, and SpyCEP, an interleukin-8 (IL-8) protease (Fig. 1). This array of proteins allows GAS to circumvent the host response and survive in an otherwise hostile environment. This thesis will focus only on virulence factors specific to the work presented.
7
Figure 1. GAS has a variety of virulence factors that contribute to disease pathogenesis.
Virulence factors such as the hyaluronic acid capsule and M protein prevent opsonophagocytosis whereas SpyCEP and SsE inhibit neutrophil infiltration. The broadspectrum protease SpeB targets both host and bacterial proteins.
Hyaluronic Acid Capsule
The GAS capsule consists of a polymer of hyaluronic acid containing repeating units of glucoronic acid and N-acetylglucosamine 42 . Synthesis of the capsule depends on coordinated transcription of three genes contained in the has operon (Fig. 1): hasA, hasB, and hasC 43 . The hasA gene encodes hyaluronate synthase, hasB encodes UDP-glucose dehydrogenase, and hasC encodes UDP-glucose pyrophosphorylase 44-46 . The hyaluronic
8 acid capsule promotes adherence to CD44 found on keratinocytes allowing for penetration into deeper tissues and subsequent dissemination 47 . However, the primary function of the capsule is to prevent phagocytosis. This is most likely accomplished by inhibiting access of phagocytes to complement found on the surface of GAS 27 . Increased capsule production has also been associated with hypervirulent GAS strains as well as prolonged post-infection sequelae of rheumatic fever 48,49 .
Streptococcal Secreted Esterase
The carboxylic esterase identified in GAS (SsE) contributes to skin invasion and systemic dissemination and immunization with SsE has been shown to provide protection against invasive infection 50-52 . SsE regulates virulence by modulating the host immune response. Esterase reduces neutrophil recruitment to the infection site by hydrolyzing the chemotactic signal, platelet-activating factor (PAF) to its biologically inactive form, lyso-
PAF (Fig. 1) 53 .
SpyCEP/ScpC
SpyCEP/ScpC is a cell wall anchored protein which cleaves the chemokine IL-
8/CXC at the C terminus (Fig. 1) 54 . IL-8 promotes neutrophil recruitment by adhering to the vasculature effectively slowing down rolling neutrophils and increasing transmigration into infected tissue 55,56 . IL-8 also induces the formation of neutrophil extracellular traps (NETs). Consequently, the degradation of IL-8 by SpyCEP prevents the formation of these NETs 57 .
9
Streptococcal Pyrogenic Toxin B (SpeB)
SpeB is an extracellular, broad-spectrum cysteine protease that degrades both host and bacterial factors (Fig. 1). This protease degrades fibronectin and vitronectin, converts IL-1 β precursor to mature IL-1 β , and cleaves a range of chemokines such as
CXCL10 and CXCL11 eliminating their antibacterial effects 58-60 . SpeB also cleaves the
M protein and the C5a peptidase from the cell wall surface and degrades the DNase,
Sda1 61-63 .
Transcriptional Regulation of Virulence Factors
GAS pathogenesis requires a sophisticated transcriptional network to regulate gene expression of these virulence factors. S. pyogenes gene transcription consists of stand-alone regulators (RRs) and two-component systems (TCSs). The RRs include
Mga, RofA-like protein, and Rgg/RopB which control expression of several virulence genes 64-66 . Mga is, perhaps, best known as a positive regulator of the emm gene but it also mediates scpA (C5a peptidase), sclA (collagen-like protein), and sic (secreted inhibitor of complement) 67,68 . Because Mga regulates numerous GAS virulence factors, deletion of mga leads to considerable attenuation of S. pyogenes in mouse models of infection 69 . RopB, another RR, is the major regulator of the non-specific cysteine protease, SpeB, and is necessary for speB transcription 70 . Mutations in ropB are frequently identified in M3 GAS strains and these single nucleotide polymorphisms
(SNPs) in ropB display a SpeB-negative phenotype and exacerbate disease 71 . In addition to the stand-alone regulators, S. pyogenes also modulates transcription via two-
10 component systems. GAS has many TCSs but the CovR/S (control of virulence) system is of particular interest because of the prominent role it plays in regulation of virulence factors. The CovR/S transcriptional network is complex and is mediated by a variety signals within the bacterium as well as the host.
CovR/S Gene Regulation
The CovR/S TCS which regulates directly or indirectly nearly 15% of the GAS genome is the primary mediator of virulence factor expression 72 . The response regulator,
CovR, represses a variety of virulence factors such as the hyaluronic acid capsule, streptokinase, and the DNase sda1 72 . The sensor kinase, CovS, regulates CovR repression of virulence factors by phosphorylation thereby altering CovR binding to the respective promoters. However, it appears CovR phosphorylation is independent of CovS as other molecules are capable of phosphotransfer to CovR such as acetyl phosphate 73 . In addition to the kinase activity of CovS, environmental signals such as increased temperate and low pH can switch CovS to a phosphatase subsequently inactivating
CovR-mediated repression 74 . Many studies have shown that changes to CovR or CovS as well as the route of infection alter GAS pathogenesis significantly leading to either attenuated or increased virulence 75-77 .
Comparison of pharyngeal and invasive GAS isolates revealed that the pharyngeal transcriptome varied by 10% from the invasive transcriptome which included 23 proven virulence factor genes 78 . Animal passage of the pharyngeal isolate MGAS2221 produced an invasive derivative strain which contained a 7-bp frameshift mutation in the covS gene suggesting covS mutations regulate CovR binding and the ability of GAS to cycle
11 between pharyngeal and invasive phenotypes during infection 75,78 . This phenotypic heterogeneity observed in vivo is an advantageous defense mechanism and enables the bacteria to survive the hostile host environment. To better elucidate the mechanism behind cycling of pharyngeal and invasive phenotypes, a considerable effort has focused on the genetic differences in transcriptional regulators such as CovR/S and how mutations in these genes affect GAS pathogenesis.
CovR/S Mutations in Hypervirulent Strains
It is apparent that mutation in covR/S plays a role in altering disease presentation; however, the extent of that role is not fully understood. Whole genome sequencing of
GAS has been used to characterize the frequency of nucleotide variation in the covR/S locus in invasive and pharyngeal strains providing evidence linking specific serotypes to an increase in covR/S mutations 79 . For example, an excess of covS polymorphisms has been reported in invasive M3 isolates relative to pharyngeal strains that are expected to result in a truncated form of the CovS protein 79 . Consequently, divergence in the rate of acquisition of covS mutations suggests host selection pressures influence invasive and pharyngeal genomes differently 79 . Furthermore, a substantial proportion of covR mutations have been observed in numerous invasive and pharyngeal isolates of different serotypes and the nonsynonymous CovR Q216P mutation has been implicated in the hypervirulence of an M3 isolate 77,79-81 . The high frequency of covR/S polymorphisms during invasive infection suggests mutations of the covR/S genes contribute directly to the severity of disease.
12
Project Objective
MGAS315, an invasive serotype M3 isolate, is hypervirulent. It has been proposed that the hypervirulence of MGAS315 is due to the acquisition of additional prophage-encoding virulence factors 82 . However, the basis for MGAS315 hypervirulence has not been established. Preliminary sequence analysis of the invasive and pharyngeal GAS isolates, MGAS315 and MGAS2221, respectively, revealed the covS gene of MGAS315 encodes a valine residue at position 457 whereas the
MGAS2221 covS gene encodes a glycine at the same position. We hypothesize the
CovS G457V mutation in MGAS315 causes its hypervirulence. The objective of this project is to test this hypothesis in order to elucidate the basis for the hypervirulence of
MGAS315.
13
MATERIALS AND METHODS
Bacterial Strains and Growth
MGAS315 and MGAS2221 are representative M3 and M1 serotypes isolated from a patient with streptococcal toxic shock syndrome in Texas and a scarlet fever patient in Australia, respectively 75,82 . MGAS6180 is a serotype M28 puerperal fever isolate 83 . MGAS2221 Δ covS and MGAS2221 Δ covS complemented with the wild-type covS gene have been described previously 75 . These strains and their derivatives were grown in Todd-Hewitt broth supplemented with 0.2% yeast extract (THY) at 37°C in 5%
CO
2
.
Generation of MGAS315 sse Deletion Mutant
The plasmid used to generate the MGAS315 Δ sse isogenic mutant (p Δ sse ) was generated by sequentially PCR cloning the downstream and upstream flanking fragments of the sse gene from MGAS315 chromosomal DNA into pGRV at the HindIII/HincII and
HindIII sites using primer pairs
[GCTGAAGCTTCCACCAATTACTTTATTTACTGGGACAC and
CGTCAGGTTGACGATACTATTGAAGCCTATATTATGG;
GCTGAAGCTTTAAACCCATTATGGTAATAATGACG and
CGTCAAGCTTGTCATCTTGTTTAGAATAGTAACTC], respectively 51,84 . This plasmid was introduced into MGAS315 using electroporation as described previously 51 .
The plasmid was integrated into the MGAS315 genome through two homologous
14 recombination events. The first crossover event occurred between the flanking fragment on p Δ sse and the homologous region in the MGAS315 genome. The strain was selected with 150
μ g/mL of spectinomycin. Transformants were passaged eight times in THY without spectinomycin to allow for the second crossover event to occur, generating an isogenic mutant which contained an in-frame deletion of sse in MGAS315 which was spectinomycin sensitive.
Generation of MGAS315 covS Deletion Mutant and Replacement with MGAS2221 covS
The covS gene of MGAS315 was deleted and then subsequently replaced with the wild-type covS gene from MGAS2221 as described previously 85 . To generate an inframe deletion of the covS gene in MGAS315, we constructed a plasmid (p Δ covS ) by amplifying the upstream and downstream flanking fragments of the 1,290-bp internal fragment of MGAS315 covS into pGRV at the BglII/XhoI and XhoI/BamHI restriction enzyme sites using primer pairs [GGACAAGCTTTGAAATAGTCTAGGATATGAG and GCGGATCCGGCAATCAGTGTAAAGGCAGA;
GCGGATCCGTAGATGGGTATCATTTACAG and
GCGGATCCTGGTAGATAGAGACCGCGTCA ], respectively. This plasmid was introduced into MGAS315 by electroporation. Chloramphenicol-resistant transformants were selected on THY agar plates with 10 µ g/ml chloramphenicol. Transformants obtained were passaged several times on THY plates to allow the second crossover event to occur, generating an in-frame deletion mutant of covS , which was chloramphenicol sensitive and identified by diagnostic PCR using primers
15
CTCTAACTCTCTTTAGACTG and GATTTCTCTCACTAAACGTG.
Next, the wild-type covS gene was inserted into the MGAS315 Δ covS genome. A
DNA fragment containing covS and the flanking sequences from MGAS2221 was PCR amplified. The PCR product was cloned into pGRV at the BglII and BamHI sites, yielding p covS , which was introduced into MGAS315 Δ covS by electroporation. The
Δ covS locus in MGAS315 Δ covS was replaced with the wild-type covS gene in p covS through two recombination events, yielding an isogenic mutant of MGAS315 that carried the wild-type covS gene (MGAS315wt covS ), which was confirmed by diagnostic PCR using primers CTCTAACTCTCTTTAGACTG and GATTTCTCTCACTAAACGTG .
DNA sequencing was used to confirm the CovS V457 mutation was replaced by the wildtype CovS G457 .
Generation of MGAS315 ropB Deletion Mutant and Replacement with MGAS2221 ropB
An in-frame ropB deletion mutant of MGAS315 missing amino acids 30–223 of
RopB was created as described above. First, the 3’ and 5’ ~ 700-bp flanking fragments of the ropB fragment were amplified from the MGAS315 chromosomal DNA using primer pairs
[GGGGACAAGTTTGTACAAAAAAGCAGGCTAGATGATATGGGACCGTTCTC and ATGTCTTGACATCAGTAGCAATTGCCTAGTGAGATAATCACC;
TTGCTACTGATGTCAAGACATTATGAACGGTGTTGTGTGTC and
GGGGACCACTTTGTACAAGAAAGCTGGGTACGTACCCAAAATGTAGGAG], respectively. Crossover PCR was used to fuse together the two PCR products via the 21-
16 bp complementary tag sequence that is underlined in the primer sequences. Using
Gateway® technology, the fused PCR product was subcloned into the donor vector pDONR221 resulting in the plasmid pDONR221Δ ropB . The Δ ropB DNA fragment was then transferred to the destination vector pBBL740 vector, yielding the suicide plasmid
BBL740Δ ropB . This plasmid was then introduced into MGAS315 using electroporation. The first crossover between BBL740Δ ropB and the homologous region in MGAS315 was selected for on THY agar plates containing 10 µ g/ml chloramphenicol.
Chloramphenicol-resistant transformants were then passaged several times in THY media to allow the second crossover event to occur, generating an in-frame deletion mutant of ropB , which was chloramphenicol sensitive and identified by diagnostic PCR using primers ATCAACTAGGAAGGCTTGAC and CAAAAGGCTAGACCTCTGC.
Next, the wild-type ropB gene from MGAS2221 was inserted into the
MGAS315 Δ ropB genome via electroporation. Generation of the plasmid containing the wild-type ropB (BBL740-wt ropB ) gene was generated as described above. Two homologous recombination events between the wt ropB plasmid and the Δ ropB locus in
MGAS315 Δ ropB resulted in the derivative MGAS315 strain containing the wild-type ropB gene (MGAS315wt ropB ) which was confirmed by diagnostic PCR using primers
ATCAACTAGGAAGGCTTGAC and CAAAAGGCTAGACCTCTGC. DNA sequencing was used to confirm the RopB P103 mutation was replaced by RopB S103 .
17
In trans Expression of the MGAS315 covS Gene in MGAS2221 Δ covS
The covS gene of MGAS315 was PCR cloned into pDCBB-RFA using Gateway®
Technology as described above. pDCBB was modified into pDCBB-RFA by inserting the blunt-ended reading frame cassette A into pDCBB at the EcoRV site 75 . The covS gene was PCR amplified from MGAS315 using primer pairs
GGGGACAAGTTTGTACAAAAAAGCAGGCTACGTTATTCGTGAGAAATAAGTC and
GGGGACCACTTTGTACAAGAAAGCTGGGTTACCTGTCACATTAACAATGC.
The PCR product was cloned into the donor vector pDONR221 resulting in pDONR221covS . The covS gene in pDONR221 was then transferred to the destination vector DCBB-
RFA yielding pDCBBcovS G1370T which was confirmed by PCR. pDCBBcovS G1370T was introduced into MGAS2221 Δ covS via electroporation.
Measurement of Esterase Production and Acetylhydrolase Activity
Esterase activity was measured using a colorimetric assay using 2-thio PAF as described previously 53 . MGAS315 and mutant strains were grown to mid-exponential phase in THY and the supernatants collected. 100 µL of supernatant was mixed with 30
µL of a solution containing 0.88 mM 2-thio PAF and 1.26 mM 5,5’-dithiobis-(2nitrobenzoic acid) (DTNB). The absorbance at 414 nm of the reactions was recorded every 10 s for 6 min using a SPECTRA Max 384 Plus spectrophotometer (Molecular
Devices, Sunnyvale, CA).
To obtain esterase in culture supernatant, MGAS315 was grown in protein-
18 reduced THY (PR-THY) to an OD
600
of 0.20, and the cultures were centrifuged to obtain the culture supernatant. Proteins in 8-13 mL of culture supernatant were precipitated with
3 volumes of cold ethanol, and the precipitates were pelleted by centrifugation and dissolved in 200 µL of saturated urea, followed by adjustment with 4X sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) loading buffer to 1X. PR-THY was prepared by passing THY through a membrane filter with a 10,000 molecular-weight cutoff as described previously 86 . For Western blotting, proteins separated by SDS-PAGE were transferred to nitrocellulose membranes with Towbin transfer buffer using a Trans-
Blot SD semidry transfer cell (Bio-Rad Laboratories) at 15 V for 40 min. The membrane was treated with 10 mL of block solution (1:20 Amersham Liquid Block in 150 mM
NaCl and 100 mM Tris-HCl, pH 7.4) for 1 h and incubated for 1 h with primary antibodies added to the block solution. The membrane was then rinsed twice and washed three times for 10 min each with 0.1% Tween 20 in PBS. The membrane was incubated with goat anti-mouse (heavy plus light chains) horseradish peroxidase-conjugated secondary antibodies (GenScript, Corp.) for 1 h and rinsed and washed as described above. Antigen-antibody reactivity was visualized by enhanced chemiluminescence.
Mouse Infections
GAS was grown to the mid-exponential phase or an optical density at 600 nm
(OD
600
) of 0.30 in THY. The bacteria were harvested by centrifugation and washed three times in pyrogen-free Dulbecco phosphate-buffered saline (DPBS) and then resuspended in DPBS to the desired doses. Groups of female CD1 mice (5 weeks old; Charles River
19
Laboratory) were subcutaneously infected with 0.2 ml of GAS suspension in DPBS at an
OD
600
of 0.08 or 1.1, and actual inocula were determined by plating. For survival studies, mice were monitored daily for 12 or 14 days to determine mortality rates. For other studies, mice were sacrificed at 24 h after inoculation to collect skin for measurement of the infected lesion size and neutrophil infiltration. Spleen and liver samples were homogenized in 0.4 mL DPBS using a Kontes pestle. Homogenates were serially diluted in DPBS and plated to quantify the number of viable GAS.
Quantification of Neutrophil Infiltration
Numbers of recruited neutrophils in the infected skin samples were determined by the myeloperoxidase assay, as described previously 53,87 . First, the skin around the infection site was peeled off, and the infection area was recognized by the boundary of inflammation in its picture and measured using the area measurement tool of the ImageJ software program (version 1.46, rsbweb.nih.gov/ij/). The infection area was excised and homogenized in 0.5% hexadecyltrimethylammonium bromide (HTAB) in 50 mM potassium and sonicated on ice for 90 s to extract myeloperoxidase. The samples were centrifuged at 3,500 RPM for 15 min. The myeloperoxidase activity in the supernatant was measured in 0.2 ml of HTAB, 0.167 mg of o-dianisidine dihydrochloride/mL, and
0.001% hydrogen peroxide. The change in absorbance at 460 nm ( Δ A
460
) was recorded over time with a SPECTRA Max 384 Plus spectrophotometer. A standard curve of myeloperoxidase activity, Δ A
460
/min, versus known numbers of murine neutrophils was used to convert the measured myeloperoxidase activity to the number of neutrophils.
20
Quantitative RT-PCR Analysis
GAS strains were grown in THY at 37°C in 5% CO
2 to an OD
600
of 0.30 and centrifuged at 3,500 RPM for 15 min. Total RNA was isolated by RNeasy minikit
(Qiagen). TaqMan real-time PCR was used to analyze the relative expression levels of hasA , spyCEP , and emm3 mRNA. Changes in the transcript levels were compared using the ΔΔ C
T
method and normalized to the control gene gyrA 51 .
SpeB Activity Assay
GAS strains were grown overnight in THY at 37°C in 5% CO
2 to stationary phase and centrifuged at 3,500 RPM for 15 min to collect the supernatants. SpeB activity was assessed by mixing 10 µL GAS supernatant with 5 µL β -mercaptoethanol and plating 5
µL of the mixture on a casein plate 88 . The plate was incubated at 37°C for 2 hours.
SpeB-positive GAS strains were identified by the presence of an opaque, white color indicating casein hydrolysis.
Statistical Analyses
All data sets were analyzed using GraphPad Prism, version 6 for Macintosh
(GraphPad Software, San Diego, CA). Survival data were analyzed using the Log-rank
(Mantel-Cox) test. Other data sets were analyzed using a two-tailed Student’s t-test, oneway ANOVA, or Kruskal-Wallis test as indicated.
21
RESULTS
Hypervirulent MGAS315 has a High Capacity to
Invade Soft Tissue and Evade Innate Immunity
Different clinical GAS isolates can display different manifestations in infections.
Mice subcutaneously infected with an invasive GAS isolate, MGAS315, could not survive (Fig. 2A), confirming its hypervirulence in previous studies 39,77,82 . In contrast, all mice infected with MGAS6180 survived (Fig. 2A). These strains must have dramatic differences in skin invasion, systemic dissemination, and innate immune evasion. Near the endpoint in the survival study, lesion size in MGAS315-infected mice (1437 ± 42 mm 2 ) was 85-fold higher compared to that in the MGAS6180 infection (16.9 ± 2.5 mm 2 )
(Fig. 2B). Concomitantly, dissemination to the spleen and liver increased drastically over the course of infection. Near the endpoint, MGAS315-treated mice had (8.1 ± 1.8) x 10 8
CFU/g and (8.9 ± 2.7) x 10 7 CFU/g GAS in the spleen and liver, respectively (Fig. 2C-D, closed symbols) . However, mice inoculated with MGAS6180 had 5495 ± 5163 CFU/g and 7180 ± 3955 CFU/g GAS in the spleen and liver, respectively (Fig. 2C-D, closed symbols). These GAS load data suggest that MGAS315 has a higher capacity to invade the skin and become systemic in the subcutaneous infection.
To further compare the systemic dissemination of the two strains, we measured the GAS load in the spleen and liver at day 1 after inoculation. Mice infected with
MGAS315 had (6.2 ± 4.8) x 10 5 CFU/g and (9.4 ± 5.3) x 10 4 CFU/g in the spleen and liver, respectively, which were 120- and 37-fold higher than the bacterial load in the spleen (4864 ± 4484 CFU/g) and liver (2484 ± 1182 CFU/g) of MGAS6180-infected
22 mice, respectively (Fig. 2C-D, open symbols). The MGAS315 bacterial load increased from 24 hours post-infection to the endpoint by >1,000 fold; however, the MGAS6180 bacterial load from day 1 to day 12 after inoculation (MGAS6180 CFU in spleen: day 1,
4864 ± 4484; day 12, 5495 ± 5163. CFU in liver: day 1, 2484 ± 1182; day 12, 7180 ±
3955) was not nearly as dramatic as MGAS315.
This difference in bacterial load was accompanied by distinct neutrophil responses to MGAS315 and MGAS6180 infection. At 24 h post-inoculation (p.i.), neutrophil infiltration at the lesion site was 3.7-fold lower in mice inoculated with
MGAS315 (4.15 ± 3.22 x 10 6 neutrophils/mm 2 ) than MGAS6180-treated mice (15.2 ±
2.02 x 10 4 neutrophils/mm 2 ) (Fig. 2E). Visual observation of the lesions revealed mice treated with MGAS315 had larger lesions with less pus-like infiltrate than MGAS6180 sites (Fig. 2F-G). MGAS315 has a high capacity to invade skin tissue, to disseminate, and to cause lethal systemic infection whereas MGAS6180 causes a persistent infection with low bacterial load and lower virulence. From this data, it is apparent MGAS315 is associated with increased systemic dissemination accompanied by reduced neutrophil recruitment.
23
Figure 2. MGAS315 is a hypervirulent isolate associated with reduced neutrophil recruitment. (A) Mice inoculated subcutaneously with MGAS315 (~1.7x10
8 CFU) had significantly higher mortality compared to mice treated with MGAS6180 (~1x10 8 CFU).
At the time of death, mice treated with MGAS315 had larger lesions (B), higher bacterial load in the spleen (C, closed), and liver (D, closed). At 24 h p.i., mice treated with
MGAS315 (~4x10 7 CFU) had higher bacterial load in the spleen (C, open) and liver (D, open) compared to MGAS6180 (~5.8x10
7 CFU). At 24 h p.i., mice treated with
MGAS315 (~1.5x10
8 CFU) had lower neutrophil influx (E) compared to MGAS6180
(~2.3x10
8 CFU). Visual observation of the lesions also revealed more severe spread and less pus-like infiltrate in mice inoculated with MGAS315 (F) compared to MGAS6180
(G). *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 as determined by a two-tailed
Student’s t-test and Log-rank (Mantel-Cox) test. Data graphed are mean ± standard error of mean (SEM) for replicate biological samples.
24
A Critical Role for the Esterase SsE in Skin Invasion and
Innate Immune Evasion by MGAS315
The streptococcal secreted esterase has been shown to play an active role in the virulence of an invasive serotype M1 strain MGAS5005 specifically through innate immune evasion. Hydrolysis of PAF by esterase impeded neutrophil recruitment and thus, enhanced virulence 53 . Additionally, immunization with the recombinant SsE protein was shown to be protective in a mouse model of subcutaneous infection with
MGAS5005 50 . Furthermore, deletion of the sse gene in MGAS5005 revealed significant attenuation of GAS following subcutaneous infection 51 . We hypothesize that SsE also critically contributes to the capability of MGAS315 to invade soft tissues and evade neutrophil responses. To test this hypothesis, we deleted the sse gene in MGAS315 and evaluated the effects of the sse deletion on MGAS315 invasion of the skin and inhibition of neutrophil recruitment in subcutaneous infection of mice. The lesion size caused by
MGAS315 Δ sse , 286 ± 32 mm 2 , was reduced by 71% compared with that caused by
MGAS315 (997.4 ± 72.5 mm 2 ) (Fig. 3A). The level of neutrophils at the MGAS315 Δ sse infection site were (27.7 ± 6.58) x 10 4 neutrophils/mm 2 , a 7.3-fold increase relative to the parental strain (3.77 ± 1.3 x 10 4 neutrophils/mm 2 ) (Fig. 3B). Thus, SsE plays a critical role in the skin invasion and innate immune evasion by MGAS315.
25
Figure 3. Esterase is required for virulence in MGAS315. At 24 h p.i., mice treated with
MGAS315 had larger lesions (A) and decreased neutrophil infiltration (B) compared to treatment with MGAS315 Δ sse . **P<0.01, ***P<0.001 as determined by a two-tailed
Student’s t-test. Data graphed are mean ± standard error of mean (SEM) for replicate biological samples.
Repairing the covS G1370T Mutation of MGAS315
The serotype M1 strain MGAS5005 contains a natural 1-bp deletion in the covS gene, and this null covS mutation is responsible for the high capacity of MGAS5005 to evade neutrophil responses and invade the skin tissue 85 . The MGAS315 skin invasion, inhibition of neutrophil recruitment, and hypervirulence observed in subcutaneous mouse infection are very similar to that of MGAS5005. The MGAS315 covS gene does not have a deletion or nonsense mutation but, rather, a covS G1370T missense mutation, resulting in the CovS G457V substitution. We hypothesize that the covS G1370T mutation enhanced the skin invasion, innate immune evasion, and hypervirulence of MGAS315.
To test our hypothesis, we generated a derivative strain from MGAS315 in which the
26 mutated covS gene was replaced by the functional covS gene from MGAS2221.
Repairing the MGAS315 covS gene was achieved by first knocking out the mutated covS gene in MGAS315 and then knocking in the MGAS2221 covS gene. The entire procedure consisted of four steps (Fig. 4A). In step 1, the suicide plasmid p Δ covS containing a chloramphenicol resistance gene in addition to the two flanking regions of the covS gene was introduced into MGAS315 and was integrated into the MGAS315 genome through a single crossover event between one flanking fragment on the plasmid and the homologous region in the MGAS315 genome resulting in a strain that was resistant to chloramphenicol. In step 2, this chloramphenicol-resistant derivative was grown on THY agar plates for at least 10 serial passages to facilitate the second crossover event between the other covS flanking fragment on the plasmid and the homologous sequence in the chromosome resulting in the MGAS315 Δ covS strain. In step 3, the suicide plasmid p covS wt containing the covS gene from MGAS2221 and its two flanking sequences was integrated into the MGAS315 Δ covS genome. A single crossover event between the flanking sequence on the plasmid and corresponding region in the chromosome yielded a chloramphenicol-resistant strain. In step 4, this strain was passaged on THY agar plates to produce the second crossover event between the other flanking sequence on the plasmid and the homologous region in the genome, resulting in the replacement of the MGAS315 covS G1370T with the wild-type covS gene.
MGAS315 Δ covS mutants in step 2 and MGAS315wt covS derivatives in step 4 were obtained by first identifying chloramphenicol-sensitive colonies and then by analyzing chloramphenicol-sensitive colonies via PCR using primers that flank the
27 deleted covS sequence. In the PCR analysis, the PCR product from MGAS315 Δ covS should be smaller than that from MGAS315 while the size of the PCR product from
MGAS315wt covS should be restored to that of MGAS315. Accordingly, we obtained strains with the smaller PCR product in step 2 and strains with the PCR product size of the full covS gene in step 4 (Fig. 4B, upper). DNA sequencing confirmed the replacement of the thymine at position 1370 of covS with a guanine in MGAS315wt covS .
(Fig. 4B, lower).
Some of our previous GAS mutants displayed down-regulation of the major virulence factor M protein due to a secondary spontaneous mutation during the construction of mutants, and M protein down-regulating mutations can cause virulence attenuation and most likely confound the interpretation of effects attributable to the function of the gene being investigated 89 . To confirm normal expression of the M protein gene in the MGAS315wt covS strain, we measured the mRNA levels of the M3 protein gene, emm3 , in MGAS315, MGAS315 Δ covS , and MGAS315wt covS by qRT-PCR. The relative levels of the emm3 transcript in MGAS315 Δ covS , and MGAS315wt covS normalized to that of gyrA was decreased by less than 0.5-fold compared with that in
MGAS315 whereas previously a >25-fold decrease in emm transcripts was observed in secondary mutations-caused M protein down-regulating mutants 89 . Furthermore, the cycle numbers reaching threshold in RT-PCR signal for MGAS315 Δ covS and
MGAS315wt covS were actually lower than that in MGAS315. Thus, the
MGAS315wt covS strain had normal M protein expression.
28
Figure 4. Replacement of CovS G457V in MGAS315 with wild-type CovS. (A) Schematic of deletion and subsequent replacement of MGAS315 covS with covS from MGAS2221.
Figure 4 Continued.
29
Figure 4. Replacement of CovS G457V in MGAS315 with wild-type CovS. (B) Upper ,
PCR confirmation of the covS deletion and replacement with wild-type covS . The picture shows agarose gel analysis of PCR reactions using MGAS315 (lane 1), MGAS315 Δ covS
(lane 2), and MGAS315wt covS (lane 3) genomic DNA. Lower , DNA sequencing verified replacement of the thymine at position 1370 with the guanine in the wild-type covS gene resulting in the subsequent valine to glycine substitution at position 457. (C)
Differences in relative emm transcript levels between MGAS315, MGAS315 Δ covS , and
MGAS315wt covS . MGAS315 Δ covS and MGAS315wt covS emm transcript expression was reduced by less than 0.5-fold compared to MGAS315. **P<0.01 as determined by
ANOVA with Tukey’s post-test. Data graphed are mean ± standard error of mean (SEM) for 2 replicate measurements.
30
Effects of the Replacement of CovS 457V with CovS 457G in MGAS315 on Expression of Multiple Virulence Genes
The two-component system CovR/S negatively regulates multiple virulence genes, including the capsule synthase gene hasA , IL-8 degrading peptidase spyCEP , and the PAF acetylhydrolase gene sse 51,72,75,90 . If the CovS G457V mutation is the basis for the high skin invasion, systemic dissemination, innate immune evasion, and virulence, it must relieve the CovR/S suppression of multiple virulence genes. If true, the replacement of CovS 457V with CovS 457G should reduce the expression of hasA , spyCEP , and sse . To test this idea, MGAS315wt covS was compared with MGAS315 and
MGAS315 Δ covS in hasA, spyCEP expression as well as esterase production. We grew
MGAS315, MGAS315 Δ covS , and MGAS315wt covS to mid-exponential phase and measured transcript abundance of hasA and spyCEP . The level of hasA mRNA in
MGAS315wt covS was reduced by 4.2-fold compared with MGAS315 (Fig. 5A) while spyCEP expression was down-regulated by 32.8-fold (Fig. 5B). The difference in the down-regulation between hasA and spyCEP expression suggest that CovR/S with the
CovS G457V mutation could still negatively control hasA to some extent but fully relieve the repression of spyCEP . Consequently, deletion of the covS gene from MGAS315 further increased the expression of hasA but not spyCEP .
To provide additional support for the effect of the CovS G457V mutation on virulence gene expression, we transformed an MGAS2221 Δ covS strain with a plasmid containing the MGAS315 covS G1370T gene or the MGAS2221 covS wt gene and measured hasA and spyCEP expression. The transcript abundance of hasA was 94- and 98-fold
31 lower in MGAS2221 and MGAS2221 Δ covS complemented with covS wt , respectively, compared to that in MGAS2221 Δ covS, which was similar to hasA expression observed in
MGAS315 (Fig. 5C). Additionally, there was a 178- and 135-fold decrease in the expression of spyCEP in MGAS2221 and the covS wt complement MGAS2221 Δ covS strain, respectively, relative to MGAS2221 Δ covS (Fig. 5D). However, in trans expression of covS G1370T in MGAS2221 Δ covS resulted in hasA and spyCEP expression levels similar to those seen in MGAS2221 Δ covS (Fig. 5C-D). This data further demonstrates that the CovS G457V mutation loses the repressive function of covS in regulation of multiple virulence genes.
To determine the effect of covS mutation on sse expression, we compared the activity levels of the PAF acetylhydrolase in the culture supernatant of MGAS315,
MGAS315 Δ covS , and MGAS315wt covS using the colorimetric 2-thio PAF assay 53 . The
PAF acetylhydrolase activity of esterase was markedly lower in the MGAS315wt covS strain (Fig. 5E) and was accompanied by a significant reduction in the amount of esterase produced as shown in the western blotting analysis (Fig. 5F). These results validate the contribution of this CovS G457V mutation to high levels of CovR/S-controlled virulence factors in MGAS315.
32
Figure 5. CovS G457V mutation in MGAS315 increases expression of multiple virulence factors. Relative quantification of hasA and spyCEP in MGAS315, MGAS2221 and isogenic mutants. MGAS315wt covS had decreased hasA (A) and spyCEP (B) expression compared to wild-type MGAS315. MGAS315 Δ covS had higher expression of hasA (A) but not spyCEP (B) compared to MGAS315. In trans expression of covS G1370T in
MGAS2221 Δ covS restored hasA (C) and spyCEP (D) expression levels to those observed in MGAS2221 Δ covS . Gene expression is normalized to gyrA expression. ***P<0.001,
****P<0.0001 as determined by ANOVA with Tukey’s post-test when compared to
MGAS315. Data graphed are mean ± standard error of mean (SEM) from 2 replicate measurements.
Figure 5 Continued.
33
Figure 5. CovS G457V mutation in MGAS315 increases expression of multiple virulence factors. (E) GAS strains were grown to an OD
600
of 0.30 and acetylhydrolase activity of esterase was measured using the 2-thio PAF colorimetric assay. MGAS315 and
MGAS315 Δ covS had considerably higher esterase activity compared to the THY control and MGAS315wt covS . (F) Western blot revealed a considerable decrease in the amount of esterase produced by MGAS315wt covS .
SpeB Activity is not Fully Dependent on CovS G457V Mutation
SpeB is known to degrade several host proteins as well as bacterial virulence factors and, its down-regulation is critical for GAS to transition from superficial to severe, invasive infections 63 . Epidemiological studies have revealed an inverse
34 relationship between SpeB production and disease severity 91 . Isolates from severe cases such as STSS and NF had considerably lower SpeB activity compared to those from noninvasive infections 91 . Alterations in SpeB are often attributed to covR/S polymorphisms and depending on the mutation may differentially regulate SpeB. For example, deletions in covS abrogate SpeB production while null covR mutations significantly enhance SpeB expression 75,92 . Furthermore, mutations in the SpeB regulator gene ropB also alter SpeB expression 93 . Previously, a serine to proline substitution at position 103 has been identified in the ropB gene of MGAS315 and this mutation accounts for the lack of SpeB as it prevents RopB from binding to the SpeB promoter 94 . To determine the effect of both ropB and covS mutation on SpeB activity, we used the caseinolytic plate assay as described previously to compare differences among strains 88 . SpeB production was not present in MGAS315wt covS and, in fact, was only restored when MGAS315 Δ ropB was corrected with the wild-type ropB gene (Fig. 6). From this data, it appears in M3 GAS strains SpeB production is dependent on RopB, not CovS, for proper expression; however further analysis is required to determine the effect of covS mutation on SpeB.
Figure 6. SpeB activity is absent in MGAS315wt covS . MGAS315 and isogenic mutants were grown to stationary phase and SpeB activity measured using the caseinolytic plate assay. Restoring MGAS315 covS with wild-type covS has no effect on SpeB activity; however, when MGAS315 ropB is replaced by MGAS2221 ropB activity is restored.
35
Repairing the CovS G457V Mutation Attenuates MGAS315
Skin Invasion, Innate Immune Evasion, and Virulence
Since the replacement of CovS 457V with CovS 457G reduced the expression of multiple virulence genes in MGAS315, we hypothesize that repairing this CovS 457V -to-
CovS 457G mutation reduces the capacity of MGAS315wt covS to invade soft tissue and evade innate immunity, thereby attenuating MGAS315 virulence. MGAS315wt covS was compared with MGAS315 and MGAS315 Δ covS in skin lesion size, neutrophil recruitment, and survival during subcutaneous infection of mice. 93% of mice infected with MGAS315wt covS survived whereas mice infected with MGAS315 and
MGAS315 Δ covS had an 80% and 100% mortality rate, respectively, ( P values:
MGAS315wt covS versus MGAS315, <0.0001; MGAS315wt covS versus
MGAS315 Δ covS , <0.0001), indicating that repairing the CovS G457V mutation significantly reduced virulence of MGAS315 (Fig. 7A). MGAS315 Δ covS was more virulent than MGAS315 (P = 0.0009), and this result was consistent with the higher expression levels of hasA in MGAS315 Δ covS relative to MGAS315 as shown in Figure
5A. These results suggest that the CovS G457V dramatically increases virulence but not to the full extent of null covS mutation caused increases in virulence. Repairing the covS mutation in MGAS315 also reduced skin invasion and innate immune evasion by
MGAS315. At 24 h post-inoculation, lesion size and neutrophil recruitment did not vary significantly between MGAS315 (146.2 ± 12.7 mm 2 ; 7.49 ± 1.05 x 10 4 neutrophils/mm 2 ) and MGAS315 Δ covS (161.5 ± 12.4 mm 2 ; 7.49 ± 1.53 x 10 4 neutrophils/mm 2 ) groups; however, mice inoculated with MGAS315wt covS caused significantly smaller lesions
36
(37.8 ± 2.74 mm 2 ) and induced greater neutrophil infiltration (2.68 ± 1.78 x 10 6 neutrophils/mm 2 ) compared to both MGAS315 and MGAS315 Δ covS groups (Fig. 7B-
C). Collectively, these results demonstrate that the CovS G457V mutation in MGAS315 leads to reduced neutrophil recruitment accompanied by enhanced skin invasion and virulence.
37
Figure 7. MGAS315wt covS virulence is significantly attenuated in vivo.
Mice were inoculated subcutaneously MGAS315 (~3x10 and MGAS315wt covS (~3x10 8
8 CFU), MGAS315 Δ covS (~4x10 8 CFU),
CFU). (A) Survival analysis over 14 days showed a significant increase in survival in mice treated with MGAS315wt covS . (B) Lesion size was significantly greater in wild-type MGAS315 compared to MGAS315wt covS . (C)
Neutrophil infiltration at the lesion site was significantly less in wild-type MGAS315 compared to MGAS315wt covS . *P<0.05, ****P<0.0001 as determined by ANOVA with
Tukey’s post-test or Kruskal-Wallis with Dunn’s post-test and Log-rank (Mantel-Cox) test. Data graphed are mean ± SEM for 4 replicate biological samples.
38
DISCUSSION
This project aims at understanding the basis for the hypervirulence of MGAS315.
MGAS315 was recovered from a case of severe invasive GAS infection in the late 1980s and has been shown to display hypervirulence in mouse models of infection 39,86,95 .
Prophages encoding superantigens SpeA and SpeK and the extracellular phospholipase
A2 (Sla) have been documented in MGAS315, and what’s more, recombination of these phages produced chimeras which may be responsible for the unusual rise in these hypervirulent strains of GAS 82 . Acquisition of the virulence factor Sla is a crucial molecular event in the evolution, rapid emergence, and widespread dissemination of a distinct GAS clone that causes unusually severe human infections 96 . Then again, a high frequency of mutations in covR/S have been identified in invasive GAS isolates which may offer an alternative explanation for this hypervirulence 80 . Previously, null covS mutations have been shown to enhance expression of multiple CovR/S-controlled virulence factors, skin invasion, innate immune evasion and abolish SpeB production 75,85 .
Our results suggest the CovS G457V mutation is responsible for the hypervirulence of
MGAS315, the importance of which is two-fold. First, we identified an additional event that is critical for MGAS315 hypervirulence. Second, this finding illustrates covS mutations are also associated with invasive isolates of serotype M3.
The role of the CovS G457V mutation in the hypervirulence of MGAS315 is apparently mediated by the mutation-caused enhancement of multiple virulence factors.
Mutation in covS is associated with invasive GAS strains and is known to alter virulence factor expression 79,85 . We observed a significant reduction in hasA and spyCEP when
39 wild-type MGAS315 covS was replaced with the covS gene from MGAS2221 as well as diminished esterase production and activity. These findings correlate with a decrease in lesion size and enhanced neutrophil infiltration, suggesting that circumventing the innate immune response is critical for hypervirulent GAS strains. GAS produces a variety of virulence factors that aid in evading the innate immune response and are critical for GAS survival in the host. The hyaluronic acid capsule, esterase, and SpyCEP, for example, are key bacterial components that are critical for establishing and sustaining a persistent infection. Under basal conditions, the genes encoding these proteins are tightly regulated by the CovR/S TCS but within the hostile environment of the host, CovR-mediated repression is released and these genes become activated. In invasive cases, the CovR/S
TCS becomes dysregulated leading to uncontrolled transcription of virulence factors resulting in severe disease. Hypervirulent GAS strains are associated with a high frequency of covR/S mutations and null covS mutations increase hasA and spyCEP expression in an invasive M1 isolate 79,85 . However, these findings have yet to be documented in a M3 invasive isolate and the subsequent effect on innate immune evasion is unknown.
Repairing the CovS G457V mutation in MGAS315 lowered hasA and spyCEP expression significantly. Several studies have suggested a role for both SpyCEP and the capsule in innate immune evasion. SpyCEP has been shown to inhibit neutrophil recruitment by degradation of the chemokine IL-8 while the hyaluronic acid capsule enhances resistance to NET-mediated extracellular killing 57,90,97 . Notably, expression of the capsule was absolutely necessary for the acquisition of covR/S mutations and the
40 switch to an invasive phenotype in vivo 97 . Our work demonstrates partial relief of the
CovR repression of spyCEP and hasA as a result of the CovS G457V mutation in MGAS315 contributes to decreased neutrophil ingress at the lesion site.
Additionally, deletion of sse in MGAS315 displayed decreased lesion size and increased neutrophil infiltration (Fig.
3). This is not surprising given that previous work has shown that SsE is important for inhibition of neutrophil recruitment by hydrolysis of platelet-activating factor 53 . Our data showed repairing the covS mutation reduced esterase production and activity considerably. Thus, it appears covS mutation in hypervirulent isolates removes repression of sse further preventing neutrophil influx to the lesion site.
SpeB activity, or lack thereof, is a defining characteristic of invasive isolates and epidemiological studies have linked polymorphisms in covR/S to a loss in SpeB production 75,91 . Interestingly, while the CovS G457V mutation appears to be responsible for the increase in virulence factor expression, it doesn’t appear to affect SpeB production in
MGAS315 as repairing the CovS G457V mutation in MGAS315 did not restore SpeB activity. This result is consistent with the previous finding that the RopB S103P mutation is responsible for the SpeB production-negative phenotype 94 . The MGAS315 derivative strain with wild-type RopB/CovS G457V produces SpeB, indicating that the CovS G457V mutation does not abolish SpeB production. This is the first identified covS mutation that enhances virulence factor expression but does not affect SpeB production. If the enhanced expression of multiple virulence factors and abolishment of SpeB production both contribute to the hypervirulence of invasive GAS strains, the CovS G457V mutation of
MGAS315 was likely acquired after the RopB S103P mutation occurred. This speculation
41 is consistent with the finding that ropB polymorphisms in serotype M3 GAS strains are significantly associated with pharyngeal infections relative to invasive isolates such as
MGAS315 98 . Future work may focus on characterizing the interaction between RopB and CovR/S and how combinatorial mutation in these genes dictates virulence factor expression and subsequent innate immune evasion in vivo .
In summary, the CovS G457V mutation is required to relieve repression of virulence genes hasA , spyCEP , and sse leading to enhanced skin invasion, inhibition of neutrophil recruitment, and GAS dissemination. Although, RopB S103P mutation is necessary for the abrogation of SpeB, CovS G457V mutation doesn’t appear to have an effect. These results indicate that an intact CovR/S system are critical for preventing GAS from causing invasive infections and the introduction of mutations in the covS and ropB genes contributes to a reduced neutrophil response leading to a hypervirulent phenotype.
42
CONCLUSION
The basis for hypervirulence of serotype M3 GAS strains has been attributed to the acquisition of prophages encoding virulence factors and the subsequent recombination of phages. Herein, we describe a previously unrecognized mechanism for this hypervirulence in an M3 GAS isolate, MGAS315. Epidemiological studies have shown a considerable proportion of invasive GAS strains contain covR/S mutations such as MGAS315 which contains a glycine to valine substitution at position 457. By generating an isogenic derivative strain of MGAS315 where the mutated covS gene was restored to wild-type, we gained further insight into the effect of covS mutation on hypervirulence in MGAS315. First, MGAS315 has a high capacity to invade the skin, evade innate immune responses, and accumulate high systemic GAS loads, and we identified the virulence factor SsE as a major contributor in MGAS315 skin invasion and innate immune evasion. Second, replacement of the MGAS315 covS 1370T gene with the
MGAS2221 covS 1370G gene reduced skin invasion as well as the expression of the virulence genes hasA , spyCEP , and sse leading to enhanced neutrophil recruitment, attenuating the hypervirulence of MGAS315. Third, in trans expression of covS wt but not covS 1370T in MGAS2221 Δ covS reversed the effect of the covS deletion on the virulence gene expression in MGAS2221.
Lastly, repairing the RopB S103P mutation in MGAS315 also reduced the expression of hasA , spyCEP , and sse (data not shown) and restored
SpeB production even in the presence of the CovS G457V mutation. These observations are summarized in Table 1. We conclude that both the CovS G457V and RopB S103P mutations contribute to the hypervirulence of MGAS315.
43
Null covS mutations in invasive serotype M1 strains enhance the expression of multiple virulence genes and abolish SpeB production 85 . We show here a covS missense mutation that enhances expression of multiple virulence genes but has no effect on SpeB production in an M3 strain. These findings are unusual for a hypervirulent GAS strain as mutations within covR/S are often linked to the lack of SpeB in invasive GAS isolates 91 .
Our data suggest that in MGAS315 the SpeB-negative phenotype can be attributed to the mutation in ropB as replacement of RopB P103 with wild-type RopB S103 restored SpeB production. Surprisingly, it appears that both RopB S103P and CovS G457V mutations are required for enhanced expression of hasA , spyCEP , and sse in MGAS315 ; however, more detailed experiments are needed to verify this possibility. It is known that the functional RopB is required for SpeB production but is not involved in regulation of hasA , spyCEP , and sse in M1 strains, and, therefore, our results indicate that the regulation of virulence genes in MGAS315 is different from that in M1 strains. To our knowledge this is the first example of an invasive GAS isolate that is dependent on simultaneous covR/S and ropB mutations for increased virulence factor expression.
Table 1. Gene expression patterns and SpeB production in MGAS2221, MGAS315, and
MGAS315 isogenic Mutants.
44
As outlined below, our findings are consistent with a model wherein the introduction of point mutations in both covS and ropB are required to relieve repression of the virulence genes hasA , spyCEP , and sse ; however, only mutation in ropB is necessary for the abolishment of SpeB production (Fig. 8). The synergistic combination of enhanced virulence factor expression and absence of SpeB in MGAS315 leads to increased skin invasion, reduced neutrophil infiltration, and systemic GAS survival (Fig.
8). The work presented here offers an alternative explanation for the hypervirulence exhibited by MGAS315 as well as illustrates a complex regulatory relationship between
RopB and CovR/S.
45
Figure 8. Model of the effect of covS and ropB mutations on MGAS315 infection. Both the CovS 457V and RopB S103P mutations are necessary for increased expression of virulence factors hasA , spyCEP , and sse in MGAS315. Only RopB S103P mutation is required for the abolishment of SpeB. The combination of increased virulence factor expression and the lack of SpeB enhances skin invasion and innate immune evasion by MGAS315.
46
1.
REFERENCES CITED
Olsen R, Musser J. Molecular pathogenesis of necrotizing fasciitis. Annual
Review of Pathology-Mechanisms of Disease 2010;5:1-31.
2. Horn D, Zabriskie J, Austrian R, Cleary P, Ferretti J, Fischetti V, Gotschlich E,
Kaplan E, McCarty M, Opal S and others. Why have group A streptococci remained susceptible to penicillin? Report on a symposium. Clinical Infectious
Diseases 1998;26(6):1341-1345.
3. O'Loughlin R, Roberson A, Cieslak P, Lynfield R, Gershman K, Craig A,
Albanese B, Farley M, Barrett N, Spina N and others. The epidemiology of invasive group a streptococcal infection and potential vaccine implications:
United States, 2000-2004. Clinical Infectious Diseases 2007;45(7):853-862.
4. Sharkawy A, Low D, Saginur R, Gregson D, Schwartz B, Jessamine P, Green K,
McGeer A, Study OGAS. Severe group A streptococcal soft-tissue infections in
Ontario: 1992-1996. Clinical Infectious Diseases 2002;34(4):454-460.
5. World Health Organization. Dept. of Child and Adolescent Health and
Development. The current evidence for the burden of Group A Streptococcal diseases. Geneva: World Health Organization; 2005. 52 p. p.
6. Centers for Disease Control P. Outbreak of group A streptococcal pneumonia among Marine Corps recruits, 1 Nov–20 Dec, California 2002. 106-
109 p.
7. Lennon D, Stewart J, Farrell E, Palmer A, Mason H. School-based prevention of acute rheumatic fever: a group randomized trial in New Zealand. Pediatric
Infectious Disease Journal 2009;28(9):787-794.
8. Carapetis J, Currie B, Kaplan E. Epidemiology and prevention of group A streptococcal infections: Acute respiratory tract infections, skin infections, and their sequelae at the close of the twentieth century. Clinical Infectious Diseases
1999;28(2):205-210.
9. Carapetis J, Connors C, Yarmirr D, Krause V, Currie B. Success of a scabies control program in an Australian Aboriginal community. Pediatric Infectious
Disease Journal 1997;16(5):494-499.
10. Gardiner D, Sriprakash K. Molecular epidemiology of impetiginous group A streptococcal infections in Aboriginal communities of northern Australia. Journal of Clinical Microbiology 1996;34(6):1448-1452.
47
11. Carapetis J, Steer A, Mulholland E, Weber M. The global burden of group A streptococcal diseases. Lancet Infectious Diseases 2005;5(11):685-694.
12. Beall B, Facklam R, Thompson T. Sequencing emm-specific PCR products for routine and accurate typing of group a streptococci. Journal of Clinical
Microbiology 1996;34(4):953-958.
13. Facklam R, Martin D, Lovgren M, Johnson D, Efstratiou A, Thompson T, Gowan
S, Kriz P, Tyrrell G, Kaplan E and others. Extension of the Lancefield classification for group A streptococci by addition of 22 new M protein gene sequence types from clinical isolates: emm103 to emm124. Clinical Infectious
Diseases 2002;34(1):28-38.
14. Dey N, McMillan D, Yarwood P, Joshi R, Kumar R, Good M, Sriprakash K,
Vohra H. High diversity of group A streptococcal emm types in an Indian community: The need to tailor multivalent vaccines. Clinical Infectious Diseases
2005;40(1):46-51.
15. Abdissa A, Asrat D, Kronvall G, Shittu B, Achiko D, Zeidan M, Yamuah L,
Aseffa A. High diversity of group A streptococcal emm types among healthy schoolchildren in Ethiopia. Clinical Infectious Diseases 2006;42(10):1362-1367.
16. Steer A, Law I, Matatolu L, Beall B, Carapetis J. Global emm type distribution of group A streptococci: systematic review and implications for vaccine development. Lancet Infectious Diseases 2009;9(10):611-616.
17. Hollingshead S, Readdy T, Yung D, Bessen D. Structural heterogeneity of the emm-gene cluster in group A Streptococci. Molecular Microbiology
1993;8(4):707-717.
18. Bessen D, McGregor K, Whatmore A. Relationships between emm and multilocus sequence types within a global collection of Streptococcus pyogenes.
Bmc Microbiology 2008;8.
19. McGregor K, Spratt B, Kalia A, Bennett A, Bilek N, Beall B, Bessen D.
Multilocus sequence typing of Streptococcus pyogenes representing most known emm types and distinctions among subpopulation genetic structures. Journal of
Bacteriology 2004;186(13):4285-4294.
20. Bessen D, Lizano S. Tissue tropisms in group A streptococcal infections. Future
Microbiology 2010;5(4):623-638.
48
21. Martin J, Barbadora K. Continued high caseload of rheumatic fever in western
Pennsylvania: Possible rheumatogenic emm types of Streptococcus pyogenes.
Journal of Pediatrics 2006;149(1):58-63.
22. Linder J, Bates D, Lee G, Finkelstein J. Antibiotic treatment of children with sore throat. Jama-Journal of the American Medical Association 2005;294(18):2315-
2322.
23. Bisno A. Primary care: Acute pharyngitis. New England Journal of Medicine
2001;344(3):205-211.
24. Centers for Disease Control P. Nosocomial group A streptococcal infections associated with asymptomatic health-care workers–Maryland and
California, 1997. 1999. 163-166 p.
25. Ralph A, Carapetis J. Group A streptococcal diseases and their global burden.
Host-Pathogen Interactions in Streptococcal Diseases 2013;368(1):1-22.
26. Centers for Disease Control P. 2013 October 13. Scarlet Fever: A Group A
Streptococcal Infection. Accessed 2013 October 13.
27. Cunningham M. Pathogenesis of group A streptococcal infections. Clinical
Microbiology Reviews 2000;13(3):470-+.
28. Carapetis J, McDonald M, Wilson N. Acute rheumatic fever. Lancet
2005;366(9480):155-168.
29. Vos Q, Lees A, Wu Z, Snapper C, Mond J. B-cell activation by T-cellindependent type 2 antigens as an integral part of the humoral immune response to pathogenic microorganisms. Immunological Reviews 2000;176:154-170.
30. Svensson N, Oberg S, Henriques B, Holm S, Kallenius G, Romanus V, Giesecke
J. Invasive group A streptococcal infections in Sweden in 1994 and 1995:
Epidemiology and clinical spectrum. Scandinavian Journal of Infectious Diseases
2000;32(6):609-614.
31. Factor S, Levine O, Schwartz B, Harrison L, Farley M, McGeer A, Schuchat A.
Invasive group A streptococcal disease: Risk factors for adults. Emerging
Infectious Diseases 2003;9(8):970-977.
32. Tajiri T, Tate G, Akita H, Ohike N, Masunaga A, Kunimura T, Mitsuya T,
Morohoshi T. Autopsy cases of fulminant-type bacterial infection with necrotizing fasciitis: Group A (beta) hemolytic Streptococcus pyogenes versus
Vibrio vulnificus infection. Pathology International 2008;58(3):196-202.
49
33. Mehta S, McGeer A, Low D, Hallett D, Bowman D, Grossman S, Stewart T.
Morbidity and mortality of patients with invasive group A streptococcal infections admitted to the ICU. Chest 2006;130(6):1679-1686.
34. Stevens D. Streptococcal toxic-shock syndrome - spectrum of disease, pathogenesis, and new concepts in treatment. Emerging Infectious Diseases
1995;1(3):69-78.
35. Tilanus A, de Geus H, Rijnders B, Dwarkasing R, van der Hoven B, Bakker J.
Severe group A streptococcal toxic shock syndrome presenting as primary peritonitis: a case report and brief review of the literature. International Journal of
Infectious Diseases 2010;14:E208-E212.
36. Herman A, Kappler J, Marrack P, Pullen A. Superantigens - mechanism of T-cell stimulation and role in immune responses. Annual Review of Immunology
1991;9:745-772.
37. Hackett S, Stevens D. Streptococcal toxic shock syndrome - synthesis of tumor necrosis factor and interleukin-1 by monocytes stimulated with pyrogenic exotoxin A and streptolysin O. Journal of Infectious Diseases 1992;165(5):879-
885.
38. Fast D, Schlievert P, Nelson R. Toxic shock syndrome-associated Staphylococcal and Streptococcal pyrogenic toxins are potent inducers of tumor necrosis factor production. Infection and Immunity 1989;57(1):291-294.
39. Musser J, Hauser A, Kim M, Schlievert P, Nelson K, Selander R. Streptococcus pyogenes causing toxic shock-like syndrome and other invasive diseases - clonal diversity and pyrogenic exotoxin expression. Proceedings of the National
Academy of Sciences of the United States of America 1991;88(7):2668-2672.
40. Demers B, Simor A, Vellend H, Schlievert P, Byrne S, Jamieson F, Walmsley S,
Low D. Severe invasive group A Streptococcal infections in Ontario, Canada -
1987-1991. Clinical Infectious Diseases 1993;16(6):792-800.
41. Proft T, Sriskandan S, Yang L, Fraser J. Superantigens and streptococcal toxic shock syndrome. Emerging Infectious Diseases 2003;9(10):1211-1218.
42. Stoolmiller A, Dorfman A. The biosynthesis of hyaluronic acid by Streptococcus.
Journal of Biological Chemistry 1969;244(2):236-&.
43. Dougherty B, Vanderijn I. Molecular characterization of a locus required for hyaluronic acid capsule production in group A Streptococci. Journal of
Experimental Medicine 1992;175(5):1291-1299.
50
44. Dougherty B, Vanderijn I. Molecular characterization of hasA from an operon required for hyaluronic acid synthesis in group A Streptococci. Journal of
Biological Chemistry 1994;269(1):169-175.
45. Dougherty B, Vanderijn I. Molecular characterization of hasB from an operon required for hyaluronic acid synthesis in group A Streptococci - demonstration of
UDP-glucose dehydrogenase activity. Journal of Biological Chemistry
1993;268(10):7118-7124.
46. Crater D, Dougherty B, Vanderijn I. Molecular characterization of hasC from an operon required for hyaluronic acid synthesis in group A Streptococci - demonstration of UDP-glucose pyrophosphorylase activity. Journal of Biological
Chemistry 1995;270(48):28676-28680.
47. Cywes C, Stamenkovic I, Wessels M. CD44 as a receptor for colonization of the pharynx by group A Streptococcus. Journal of Clinical Investigation
2000;106(8):995-1002.
48. Hynes W. Virulence factors of the group A streptococci and genes that regulate their expression. Frontiers in Bioscience 2004;9:3399-3433.
49. Wessels M, Bronze M. Critical role of the group A Streptococcal capsule in pharyngeal colonization and infection in mice. Proceedings of the National
Academy of Sciences of the United States of America 1994;91(25):12238-12242.
50. Liu M, Zhu H, Zhang J, Lei B. Active and passive immunizations with the streptococcal esterase Sse protect mice against subcutaneous infection with group
A Streptococci. Infection and Immunity 2007;75(7):3651-3657.
51. Zhu H, Liu M, Sumby P, Lei B. The secreted esterase of group A Streptococcus is important for invasive skin infection and dissemination in mice. Infection and
Immunity 2009;77(12):5225-5232.
52. Stock A, Grabar P, Uriel J. Esterase in extracellular concentrates of group A
Streptococci and homologous antibody. Nature 1961;192(480):434-&.
53. Liu M, Zhu H, Li J, Garcia C, Feng W, Kirpotina L, Hilmer J, Tavares L, Layton
A, Quinn M and others. Group A Streptococcus secreted esterase hydrolyzes platelet-activating factor to impede neutrophil recruitment and facilitate innate immune evasion. Plos Pathogens 2012;8(4).
51
54. Edwards R, Taylor G, Ferguson M, Murray S, Rendell N, Wrigley A, Bai Z,
Boyle J, Finney S, Jones A and others. Specific C-terminal cleavage and inactivation of interleukin-8 by invasive disease isolates of Streptococcus pyogenes. Journal of Infectious Diseases 2005;192(5):783-790.
55. Middleton J, Neil S, Wintle J, ClarkLewis I, Moore H, Lam C, Auer M, Hub E,
Rot A. Transcytosis and surface presentation of IL-8 by venular endothelial cells.
Cell 1997;91(3):385-395.
56. DiVietro J, Smith M, Smith B, Petruzzelli L, Larson R, Lawrence M.
Immobilized IL-8 triggers progressive activation of neutrophils rolling in vitro on
P-selectin and intercellular adhesion molecule-1. Journal of Immunology
2001;167(7):4017-4025.
57. Zinkernagel A, Timmer A, Pence M, Locke J, Buchanan J, Turner C, Mishalian I,
Sriskandan S, Hanski E, Nizet V. The IL-8 protease SpyCEP/ScpC of Group A
Streptococcus promotes resistance to neutrophil killing. Cell Host & Microbe
2008;4(2):170-178.
58. Kapur V, Topouzis S, Majesky M, Li L, Hamrick M, Hamill R, Patti J, Musser J.
A conserved Streptococcus pyogenes extracellular cysteine protease cleaves human fibronectin and degrades vitronectin. Microbial Pathogenesis
1993;15(5):327-346.
59. Kapur V, Majesky M, Li L, Black R, Musser J. Cleavage of interleukin-1-beta
(IL-1-beta) precursor to produce active IL-1-beta by a conserved extracellular cysteine protease from Streptococcus pyogenes. Proceedings of the National
Academy of Sciences of the United States of America 1993;90(16):7676-7680.
60. Egesten A, Olin A, Linge H, Yadav M, Morgelin M, Karlsson A, Collin M. SpeB of Streptococcus pyogenes differentially modulates antibacterial and receptor activating properties of human chemokines. Plos One 2009;4(3).
61. Berge A, Bjorck L. Streptococcal cysteine proteinase releases biologically active fragments of Streptococcal surface proteins. Journal of Biological Chemistry
1995;270(17):9862-9867.
62. Raeder R, Woischnik M, Podbielski A, Boyle M. A secreted streptococcal cysteine protease can cleave a surface-expressed M1 protein and alter the immunoglobulin binding properties. Research in Microbiology 1998;149(8):539-
548.
52
63. Aziz R, Pabst M, Jeng A, Kansal R, Low D, Nizet V, Kotb M. Invasive M1T1 group A Streptococcus undergoes a phase-shift in vivo to prevent proteolytic degradation of multiple virulence factors by SpeB. Molecular Microbiology
2004;51(1):123-134.
64. Almengor A, Walters M, McIver K. Mga is sufficient to activate transcription in vitro of sof-sfbX and other Mga-regulated virulence genes in the group A streptococcus. Journal of Bacteriology 2006;188(6):2038-2047.
65. Beckert S, Kreikemeyer B, Podbielski A. Group A streptococcal rofA gene is involved in the control of several virulence genes and eukaryotic cell attachment and internalization. Infection and Immunity 2001;69(1):534-537.
66. Chaussee M, Sylva G, Sturdevant D, Smoot L, Graham M, Watson R, Musser J.
Rgg influences the expression of multiple regulatory loci to coregulate virulence factor expression in Streptococcus pyogenes. Infection and Immunity
2002;70(2):762-770.
67. Caparon M, Scott J. Identification of a gene that regulates expression of M protein, the major virulence determinant of group A Streptococci. Proceedings of the National Academy of Sciences of the United States of America
1987;84(23):8677-8681.
68. Ribardo D, McIver K. Defining the Mga regulon: comparative transcriptome analysis reveals both direct and indirect regulation by Mga in the group A streptococcus. Molecular Microbiology 2006;62(2):491-508.
69. Luo F, Lizano S, Banik S, Zhang H, Bessen D. Role of Mga in group A streptococcal infection at the skin epithelium. Microbial Pathogenesis
2008;45(3):217-224.
70. Lyon W, Gibson C, Caparon M. A role for Trigger Factor and an Rgg-like regulator in the transcription, secretion and processing of the cysteine proteinase of Streptococcus pyogenes. Embo Journal 1998;17(21):6263-6275.
71. Carroll R, Shelburne S, Olsen R, Suber B, Sahasrabhojane P, Kumaraswami M,
Beres S, Shea P, Flores A, Musser J. Naturally occurring single amino acid replacements in a regulatory protein alter streptococcal gene expression and virulence in mice. Journal of Clinical Investigation 2011;121(5):1956-1968.
53
72. Graham M, Smoot L, Migliaccio C, Virtaneva K, Sturdevant D, Porcella S,
Federle M, Adams G, Scott J, Musser J. Virulence control in group A
Streptococcus by a two-component gene regulatory system: Global expression profiling and in vivo infection modeling. Proceedings of the National Academy of
Sciences of the United States of America 2002;99(21):13855-13860.
73. McCleary W, Stock J. Acetyl phosphate and the activation of two-component response regulators. Journal of Biological Chemistry 1994;269(50):31567-31572.
74. Churchward G. The two faces of Janus: virulence gene regulation by CovR/S in group A streptococci. Molecular Microbiology 2007;64(1):34-41.
75. Trevino J, Perez N, Ramirez-Pena E, Liu Z, Shelburne S, Musser J, Sumby P.
CovS simultaneously activates and inhibits the CovR-mediated repression of distinct subsets of Group A Streptococcus virulence factor-encoding genes.
Infection and Immunity 2009;77(8):3141-3149.
76. Alam F, Turner C, Smith K, Wiles S, Sriskandan S. Inactivation of the CovR/S virulence regulator impairs infection in an improved murine model of
Streptococcus pyogenes naso-pharyngeal infection. Plos One 2013;8(4).
77. Horstmann N, Sahasrabhojane P, Suber B, Kumaraswami M, Olsen R, Flores A,
Musser J, Brennan R, Shelburne S. Distinct single amino acid replacements in the control of virulence regulator protein differentially impact streptococcal pathogenesis. Plos Pathogens 2011;7(10).
78. Sumby P, Whitney A, Graviss E, Deleo F, Musser J. Genome-wide analysis of group A streptococci reveals a mutation that modulates global phenotype and disease specificity. Plos Pathogens 2006;2(1):41-49.
79. Shea P, Beres S, Flores A, Ewbank A, Gonzalez-Lugo J, Martagon-Rosado A,
Martinez-Gutierrez J, Rehman H, Serrano-Gonzalez M, Fittipaldi N and others.
Distinct signatures of diversifying selection revealed by genome analysis of respiratory tract and invasive bacterial populations. Proceedings of the National
Academy of Sciences of the United States of America 2011;108(12):5039-5044.
80. Ikebe T, Ato M, Matsumura T, Hasegawa H, Sata T, Kobayashi K, Watanabe H.
Highly Frequent Mutations in Negative Regulators of Multiple Virulence Genes in Group A Streptococcal Toxic Shock Syndrome Isolates. Plos Pathogens
2010;6(4).
54
81. Miyoshi-Akiyama T, Ikebe T, Watanabe H, Uchiyama T, Kirikae T, Kawamura
Y. Use of DNA Arrays to identify a mutation in the negative regulator, csrR, responsible for the high virulence of a naturally occurring type M3 group A streptococcus clinical isolate. Journal of Infectious Diseases 2006;193(12):1677-
1684.
82. Beres S, Sylva G, Barbian K, Lei B, Hoff J, Mammarella N, Liu M, Smoot J,
Porcella S, Parkins L and others. Genome sequence of a serotype M3 strain of group A Streptococcus: Phage-encoded toxins, the high-virulence phenotype, and clone emergence. Proceedings of the National Academy of Sciences of the United
States of America 2002;99(15):10078-10083.
83. Green N, Zhang S, Porcella S, Nagiec M, Barbian K, Beres S, LeFebvre R,
Musser J. Genome sequence of a serotype m28 strain of group A Streptococcus:
Potential new insights into puerperal sepsis and bacterial disease specificity.
Journal of Infectious Diseases 2005;192(5):760-770.
84. Liu M, Hanks T, Zhang J, McClure M, Siemsen D, Elser J, Quinn M, Lei B.
Defects in ex vivo and in vivo growth and sensitivity to osmotic stress of group A
Streptococcus caused by interruption of response regulator gene vicR.
Microbiology-Sgm 2006;152:967-978.
85. Li J, Zhu H, Feng W, Liu M, Song Y, Zhang X, Zhou Y, Bei W, Lei B.
Regulation of inhibition of neutrophil infiltration by the two-component regulatory system CovRS in subcutaneous murine infection with Group A
Streptococcus. Infection and Immunity 2013;81(3):974-983.
86. Lei B, Mackie S, Lukomski S, Musser J. Identification and immunogenicity of group A Streptococcus culture supernatant proteins. Infection and Immunity
2000;68(12):6807-6818.
87. Bradley P, Priebat D, Christensen R, Rothstein G. Measurement of cutaneous inflammation - estimation of neutrophil content with an enzyme marker. Journal of Investigative Dermatology 1982;78(3):206-209.
88. Ma Y, Bryant A, Salmi D, Hayes-Schroer S, McIndoo E, Aldape M, Stevens D.
Identification and characterization of bicistronic speB and prsA gene expression in the group A streptococcus. Journal of Bacteriology 2006;188(21):7626-7634.
89. Zhou Y, Hanks T, Feng W, Li J, Liu G, Liu M, Lei B. The sagA/pel locus does not regulate the expression of the M protein of the M1T1 lineage of group A
Streptococcus. Virulence 2013;4(8):1-9.
55
90. Sumby P, Zhang S, Whitney A, Falugi F, Grandi G, Graviss E, DeLeo F, Musser
J. A chemokine-degrading extracellular protease made by group A Streptococcus alters pathogenesis by enhancing evasion of the innate immune response.
Infection and Immunity 2008;76(3):978-985.
91. Kansal R, McGeer A, Low D, Norrby-Teglund A, Kotb M. Inverse relation between disease severity and expression of the streptococcal cysteine protease,
SpeB, among clonal M1T1 isolates recovered from invasive group A streptococcal infection cases. Infection and Immunity 2000;68(11):6362-6369.
92. Kansal R, Datta V, Aziz R, Abdeltawab N, Rowe S, Kotb M. Dissection of the molecular basis for hypervirulence of an in vivo-selected phenotype of the widely disseminated M1T1 strain of Group A Streptococcus bacteria. Journal of
Infectious Diseases 2010;201(6):855-865.
93. Hollands A, Aziz R, Kansal R, Kotb M, Nizet V, Walker M. A naturally cccurring
Mutation in ropB suppresses SpeB expression and reduces M1T1 Group A
Streptococcal systemic virulence. Plos One 2008;3(12).
94. Kappeler K, Anbalagan S, Dmitriev A, McDowell E, Neely M, Chaussee M. A naturally cccurring Rgg variant in serotype M3 Streptococcus pyogenes does not activate speB expression due to altered specificity of DNA binding. Infection and
Immunity 2009;77(12):5411-5417.
95. Musser J, Kapur V, Kanjilal S, Shah U, Musher D, Barg N, Johnston K,
Schlievert P, Henrichsen J, Gerlach D and others. Geographic and temporal distribution and molecular characterization of two highly pathogenic clones of
Streptococcus pyogenes expressing allelic variants of pyrogenic exotoxin A
(scarlet fever toxin). Journal of Infectious Diseases 1993;167(2):337-346.
96. Sitkiewicz I, Nagiec M, Sumby P, Butler S, Cywes-Bentley C, Musser J.
Emergence of a bacterial clone with enhanced virulence by acquisition of a phage encoding a secreted phospholipase A(2). Proceedings of the National Academy of
Sciences of the United States of America 2006;103(43):16009-16014.
97. Cole J, Pence M, von Kockritz-Blickwede M, Hollands A, Gallo R, Walker M,
Nizet V. M protein and hyaluronic acid capsule are essential for in vivo selection of covRS mutations characteristic of invasive serotype M1T1 Group A
Streptococcus. Mbio 2010;1(4).
56
98. Olsen R, Laucirica D, Watkins M, Feske M, Garcia-Bustillos J, Vu C, Cantu C,
Shelburne S, Fittipaldi N, Kumaraswami M and others. Polymorphisms in regulator of protease B (RopB) alter disease phenotype and strain virulence of serotype M3 Group A Streptococcus. Journal of Infectious Diseases
2012;205(11):1719-1729.