National Amyloidosis Centre News
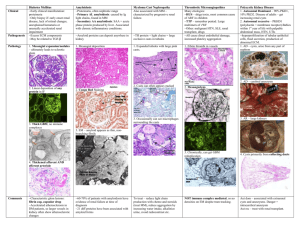
advertisement

National Amyloidosis Centre News Panel discussion held at the 6th UKAN Meeting (March 2014) on the place of stem cell transplantation and chemotherapy for AL amyloidosis. The discussion was chaired by Prof Philip Hawkins, Director of the NAC, far left. Panel members, from left to right: Dr Stefan Schoenland (Heidelberg, Germany), Dr Giovanni Palladini (Pavia, Italy) and Prof Ronjon Chakraverty (Professor of Haematology and Cellular Immunotherapy, Royal Free Hospital). Introduction The 6th Annual UK Amyloidosis Network (UKAN) Meeting, hosted by the NAC in March 2014, was well attended by doctors and researchers from around the UK, with guest lecturers from amyloid centres in Europe and the US. Lectures included state of the art updates on all types of amyloidosis and a lively panel discussion addressed the place of stem cell transplantation versus chemotherapy for AL amyloidosis. Patient members of the UK Amyloidosis Advisory Group (UKAAG) were present and later met with the NAC consultants for discussions on how the NAC can continue to excel in fulfilling patient needs. NAC consultants and scientists from the Wolfson Drug Discovery Unit attended and lectured at the XIV International Symposium on Amyloidosis, in Indianapolis, USA, from 27 April - 1 May 2014. Decades of world-leading research at the NAC have led to huge strides forward in understanding and treatment of amyloidosis. Doctors around the UK are increasingly aware that existing treatment options can improve symptoms and prolong life. Excitingly, more new treatments than ever before are now in various stages of development and trial. Our website includes recently updated information for patients on all the ongoing clinical trials at the NAC, many of which are currently recruiting patients. See http://www.ucl.ac.uk/amyloidosis/nac/clinical-research. This newsletter discusses some of the imaging scans available at the NAC and some recent clinical research studies. There is an update on the upcoming Land’s End to John O’Groats bike ride, scheduled for July, which will kick-start the ambitious project aiming to raise funds for a new MRI suite at the NAC. We are also happy to report on some of the successful fundraising for the UCL Amyloidosis Research Fund. This issue’s patient story tells Sandra Morgan’s inspiring tale of how a combined heart and kidney transplant 21 years ago gave her a chance to live a full life, despite a diagnosis of a rare type of amyloidosis at age 35. ISSUE 4: June 2014 IN THIS ISSUE Introduction 1 Strides in imaging 2 Conquering CAPS 4 Patient story: Sandra Morgan Professor Sir Mark Pepys’s perspective 5 Fundraising news 8 Donations National Amyloidosis Centre, UCL Division of Medicine, Royal Free Campus, Rowland Hill Street, London NW3 2PF, UK www.ucl.ac.uk/amyloidosis 6 12 National Amyloidosis Centre News 2 Issue 4: June 2014 Strides in imaging DPD scans The heart is in constant motion, contracting and relaxing as it pumps blood around the body. SAP scanning under routine conditions is not useful for assessment of amyloid deposits in the heart because the organ is moving, because it contains a lot of blood with the labelled tracer within it and because it takes some time for SAP to enter the cardiac amyloid deposits. heart tests appear normal. DPD scans are less useful for detecting and evaluating AL amyloid deposits in the heart, so we do not routinely perform DPD scans on patients who are known to have AL amyloid affecting the heart. At the NAC, the DPD tracer is scanned on the same Single Photon Emission Computerised Tomography (SPECT)/CT gamma camera as that used for the SAP scan. However, a different radioactive marker that does detect amyloid in the heart has recently been identified. This marker is called 99mTc-DPD, or just DPD. DPD is a “bone-seeking” tracer. When it is injected into the bloodstream it is mainly taken up by bones all through the body. It is taken up most strongly in bone regions in which there is disease or abnormality. In some countries in Europe DPD is used routinely in bone scans to detect a variety of bone illnesses. In the UK it was used for bone scans in the past, but at present other tracers are preferred. The procedure is as follows: • The DPD tracer is injected into the David Hutt, Lead Nuclear Medicine Technician at the NAC. Together with Professor Hawkins, David developed the DPD scan as a standard test for cardiac amyloidosis. Over the last 30 years there have been several case reports in which bone-seeking tracers appeared to home in on amyloid deposits in the heart, as well as detecting bone abnormalities. However, these were generally viewed as incidental findings occurring in patients who underwent bone scans for other reasons than amyloidosis. In recent years this approach has been investigated systematically for the first time. Since 2010 we have performed over 1000 DPD scans on patients at the NAC with suspected amyloid in the heart. They are also performed in some other European amyloidosis centres. The results have been impressive, and have contributed significantly to our ability to evaluate patients with cardiac amyloidosis. It turns out that DPD is very sensitive at detecting particular amyloid deposits in the heart. DPD scans are most useful when the amyloid deposits are of TTR type. Asymptomatic ATTR amyloid deposits can be detected in the heart by DPD scans at an early stage, when other patient’s vein. • It is necessary to wait 3 hours after injection of the tracer before we can begin scanning. • For each scan, the patient lies down on the scanner and there is a scan consisting of a “whole body sweep”, which shows the entire body. • The scanning camera is rotated and a type of scan called SPECT of the heart is performed while the patient remains in the same position. At the same time a routine high resolution X-ray CT scan is obtained. The combination of the 3D SPECT DPD scan and the standard X-ray 3D CT provide detailed, 3dimensional information, showing both the anatomy (structure) of the heart and the pathology (amyloid deposits) in the heart. Since DPD scans can detect ATTR amyloid deposits in the heart before other tests, they may be helpful in guiding treatment decisions, including timing of liver transplantation in: • • Asymptomatic patients who are known to carry mutations in the TTR gene that cause familial amyloid polyneuropathy. Patients with early familial amyloid polyneuropathy who do not yet have heart failure symptoms. DPD scanning and SPECT are safe tests. There is some exposure to radiation from the tracer and from the CT scan, but the exposure is minimal and is comparable with the annual background radiation people are exposed to in some parts of the country. National Amyloidosis Centre News CMR (cardiac magnetic resonance) scans CMR is a method whereby a magnetic field and radio waves are used to obtain detailed pictures of the heart. Information provided by CMR is more detailed and accurate compared with echocardiography. Further, in some patients, echocardiography may not be able to determine whether heart wall thickening is due to amyloidosis or to another cause such as hypertension. In such patients, CMR can distinguish between these different causes of heart wall thickening. In CMR imaging, a non-radioactive tracer called gadolinium is used to enhance the images. Amyloid deposits in the heart produce a very characteristic appearance after a short delay ‘late gadolinium enhancement’ (LGE) . Other patterns of LGE occur in other types of heart disease, for example if there is fibrosis, or scarring of the heart muscle. Experienced doctors can recognise the particular pattern of LGE which is associated with cardiac amyloid deposits, and researchers at the NAC have developed sophisticated new methods using the gadolinium tracer to quantify the precise amount of amyloid in the heart. A new scoring system to improve diagnosis of cardiac amyloid A recent NAC study showed that CMR imaging may help doctors to tell whether amyloid deposits in the heart are of AL or ATTR type. These are the two types of amyloidosis that most frequently affect the heart. In the past, the vast majority of patients with amyloid in the heart had AL amyloidosis, but in the last 5 years we have seen a marked increase in new cases of ATTR amyloid affecting the heart amongst patients referred to the NAC. Over the same time period, CMR has become more widely available. AL and ATTR amyloidosis are different diseases with very different treatments, so it is crucial to distinguish between these conditions. The NAC team, together with colleagues from St George’s University Hospital, London, looked at CMR scans from 100 cardiac amyloid patients, about half with AL amyloidosis and half with ATTR amyloidosis. The scans had been performed in 46 different hospitals around the UK. As discussed above, amyloid deposits in the heart cause a characteristic CMR finding called LGE. The researchers developed a new scoring system based on the LGE patterns they observed. They called it the Query Amyloid Late Enhancement (QALE) score. When used together with other clinical and CMR features, the Issue 4: June 2014 3 QALE score was very accurate in distinguishing between ATTR and AL amyloid. This could prove helpful to a growing number of patients, because of the increasing availability of CMR. Echocardiography is also widely available, but does not always reliably distinguish between amyloid and non-amyloid cardiomyopathy, and cannot distinguish between AL and ATTR amyloid. The DPD scan which can help distinguish between AL and ATTR amyloid in the heart, is only available at the NAC, where personnel have sufficient experience in scan performance and interpretation, and has only been studied in a relatively limited number of patients so far. CMR is now available in hospitals all around the UK, and the scans analysed in this study were performed in centres without specialist amyloid protocols. So QALE scoring may become helpful in diagnosis and management of many patients, although it will not replace biopsy as the gold standard diagnostic test. In the future it may also be possible to use MR to accurately measure the size of the amyloid deposits within both the heart wall and other body tissues. Such measurements could then be repeated to follow the build-up of amyloid deposits and their regression with treatment. Before the scan, contrast material may be injected into the patient’s vein. During the scan, patients lie still inside a closed “tunnel” type of scanner for up to one hour. The pictures produced by the computer can then be examined by doctors. CMR is safe and painless, and does not involve any exposure to radiation. CMR is not currently available in the NAC, so we refer patients to another hospital for this type of scan if necessary. The success of our research has led to an ever increasing need for this new investigation. The Land’s End to John O’Groats bike ride, planned for July 2014 (details on page 10) will kick off our fundraising efforts for a new MRI suite at the NAC. This will reduce the need for patients to travel, shorten waiting times for scans and allow us to scan more patients. 4 Issue 4: June 2014 National Amyloidosis Centre News Conquering CAPS: An NAC success story How NAC research led to effective treatment for a rare cause of amyloidosis NAC doctors recently published a report of the impressive success they have had in treating a condition which can lead to development of AA amyloidosis. Cryopyrin-Associated Periodic Syndrome (CAPS) is a very rare, inherited disease, usually diagnosed in childhood. Untreated, patients with CAPS experience daily flu-like symptoms from early childhood, and sometimes go on to develop AA amyloidosis. In 2001, ground-breaking research by the NAC team, led by Professor Philip Hawkins and Dr Helen Lachmann, the fever syndrome specialists, led to identification of the gene family, mutations in which cause CAPS. Based on this new understanding of the disease, Professor Hawkins went on to identify the first ever effective treatment for CAPS. This is a very rare achievement for any doctor and is vitally important even though it is such a rare disease. Subsequently the NAC doctors played a crucial role, in collaboration with the pharmaceutical company, Novartis, in development of a new drug, canakinumab, which effectively ‘switches off’ the underlying disease process causing CAPS symptoms. Patients treated with canakinumab injections every 2 months have found that this incredibly effective drug has turned their lives around. In addition to significantly improving their day to day quality of life, long term canakinumab treatment will prevent the development of the most serious complication of CAPS - AA amyloidosis. The NAC doctors share a specialist paediatric fever clinic with Dr Paul Brogan and Professor Nigel Klein at the Great Ormond Street Hospital for Children, where they collaborate in treatment of children with CAPS. The NAC and Great Ormond Street doctors recently published a report of the impressive success of this profoundly effective treatment in relieving the symptoms of patients with CAPS. Response of rash to canakinumab in a patient with the Cryopyrin-Associated Periodic Syndrome (CAPS) Immediately before the administration of the initial dose of canakinumab, this patient had a typical urticarial rash (Panel A). With 24 hours after the administration of a single dose of canakinumab, the rash had almost completely disappeared (Panel B). From Lachmann H J et al. Use of Canakinumab in the Cryopyrin-Associated Periodic Syndrome. N Eng J Med, 2009; 360: 2416-2425 (Copyright © 2009 Massachusetts Medical Society). Reprinted with permission. National Amyloidosis Centre News Issue 4: June 2014 5 Patient story: Sandra Morgan “My heart and kidney transplant gave me 21 years of life … and counting” It was in September 1989 when I was 32 years old that I first noticed my feet and ankles beginning to swell. I went to see my GP a few times about this, before he referred me to the Renal Unit at the Royal Devon and Exeter Hospital. From here I was referred in April 1990 to the Immunological Medicine Unit at London’s Hammersmith Hospital, which was then the national referral centre for amyloidosis. Here I was seen by Professor Mark Pepys, and Dr Philip Hawkins (now Professor) and underwent numerous blood tests and scans. Up until then I had not felt unwell at all. I just had swelling of the feet and ankles and was retaining fluid. After a few more trips and tests at Hammersmith, plus tests on my family in Devon, I was diagnosed with ApoAI amyloidosis, as was my father, who had had a stroke and heart defect a few years earlier. I was told I would need a kidney transplant at some point in the future as they had found amyloid in the kidneys. In 1991 the fluid problem was getting worse and I was struggling to walk, getting very breathless, and had collapsed a few times. I was admitted to the Hammersmith Hospital for more tests, where they discovered I had heart failure due to amyloid. I was told in September 1991 that I now needed a combined heart and kidney transplant. Professor Pepys then undertook a campaign to get me on to the heart transplant list at Harefield Hospital. Initially they were reluctant to take me on as they had never tried to transplant an amyloid patient and they did not know if it would work. Current thinking at the time was that the amyloid would re-appear in the transplanted organs immediately. I was 35 with a young 12 year old daughter, and Professor Pepys fought long and hard for my case to be brought to the forefront. This was 22 years ago when amyloid was not as well known as it is today. In February 1992 I was put on the transplant list for a combined heart and kidney transplant. In July of 1992 I was admitted to Hammersmith Hospital with right-sided heart failure due to excessive water retention. I needed to be drained through a catheter and had an intravenous drip of diuretic. I was in hospital for five weeks, and during that time I was sent to Harefield Hospital again to be assessed for transplant. I had had enough of hospitals as I had been away from home now for over five weeks. Thankfully I was sent home to await the outcome of their decision. While I was at home waiting I went into the Royal Devon and Exeter Hospital where I was told I was suffering from kidney failure. I had turned yellow and was bloated out with fluid. They took me in to the Renal Unit to be fitted for peritoneal dialysis but the catheter was put into the wrong place and did not work. The following day, while waiting to go to theatre for the re-fitting of the catheter, I was told they had found a match for me in Harefield, and I was rushed by ambulance from Exeter to Harefield. On arrival they took me straight in and got me ready for the transplants. This was the 14th October 1992. After the operation I found out from my husband that I had three professors in the theatre with me: Professor Sir Magdi Yacoub doing the heart, Professor Peter Morris from Oxford doing the kidney and Professor Pepys, watching and taking notes and samples. The next thing I remember is coming round three days later in ITU. During this time I was on a cocktail of painkillers and other drugs that gave me terrible nightmares and weird dreams. For the next five weeks I had biopsies through the neck every week for the heart, plus kidney biopsies. I had to travel from Exmouth to Harefield every two weeks for the first 6 months, then once a month for the next six months. This was a strain on the family as I was away for two days each time. They took heart biopsies by entering through my neck. National Amyloidosis Centre News 6 Issue 4: June 2014 Since then the heart and kidney have all been good. There have been a few little drug adjustments and the side effects of the medications have caused me all kinds of problems from gout to skin cancers, facial bloating from steroids, facial hair and more, often resulting in more medication! The skin cancers are now appearing more frequently and I have regular visits to the dermatologist for a head to toe examination. I have had over twenty lesions cut out and my skin is very thin due to all the medication. I have been to see the eye specialist as there is amyloidosis in my eyes. I have lived a full life: I have been on holidays to Florida and Los Angeles, I have learnt to drive, I enjoy walking and have great times with all my grandchildren. My transplanted kidney has now come to the end of its life and I am on the transplant list for another kidney. My sister Janice is a good match and we are hoping to get the transplant done in the near future. I have had a fantastic 21 plus years of life. This would not have been possible without the determination of Professor Pepys and his team who pushed for me to have the transplants. I would like to give Professor Sir Mark Pepys a huge thank you for giving me my life back. Just after writing this, Sandra received her second kidney transplant from her sister, and Sandra, the new kidney and her sister are all doing well! Professor Sir Mark Pepys’s perspective “I phoned the heart transplant team every single week to push for Sandra’s transplant” I became interested in amyloid and amyloidosis in 1976, when I was Head of the Immunology Department at the Royal Free Hospital School of Medicine. When I moved to the Royal Postgraduate Medical School at Hammersmith Hospital in 1977 and set up the Immunological Medicine Unit there, I started to see patients with amyloidosis. In 1986 I invented the SAP whole body scan for diagnosing and monitoring amyloidosis and showed that it worked experimentally. Philip Hawkins joined me soon afterwards to study for his PhD degree and for his project I assigned him to establish the method in human patients. Under my supervision he first developed it further in experimental models and then rapidly and successfully transferred the technology to patients. It is worth noting that it is fortunate that we did this in 1986-7 because current regulations and constraints in medical research, intended to prevent harm to patients, incur such huge development costs that this harmless and amazingly helpful test would never have become available for clinical use. In fact we have safely performed over 29,000 SAP scans, with immense benefit to many thousands of patients. During the course of his studies Philip did wonderful work in developing and perfecting the SAP scan and also gained great experience in diagnosing and managing patients with amyloidosis. By the time he got his PhD degree in 1989 I had no hesitation in appointing him to a Consultant Physician post and putting him in charge of looking after all the amyloidosis patients who were then being referred to me. Having the SAP scan enabled us for the first time to understand properly the natural history of amyloidosis and its response to treatment, uniquely better than anywhere else in the world. As a result more and more patients were referred and we became the de facto national referral centre for this disease. Eventually, when we moved back to the Royal Free Hospital, by then a part of University College London, I established the UK NHS National Amyloidosis Centre in 1999, with Philip as the ideal person to head it. He has done this with great skill and success, so that he is now the leading clinical specialist in amyloidosis in the world and runs the world’s leading centre for amyloidosis. Sandra Morgan is one of our most remarkable patients. We diagnosed her hereditary apolipoprotein AI amyloidosis on her referral to us in 1990. It was already quite advanced, despite her young age of only 35, and over the next couple of years she rapidly deteriorated into heart and kidney failure. Apart from support for the function of failing organs, the only treatment for National Amyloidosis Centre News amyloidosis, then and now, is to try to reduce the abundance of the precursor protein which forms the amyloid fibrils that cause the disease. If this can be achieved, accumulation of amyloid is halted and organ function may be stabilised, unless the damage is already too severe. ApoAI is produced by the liver and the small intestine and unfortunately no treatment or intervention is available to reduce it. All that could be done for Sandra was to replace the functions of her failing organs and fortunately both kidney and heart transplantation are possible. Given her young age and the fact that she had a young daughter I thought that she was an ideal candidate for transplantation, even though this had never been done in such patients before. Firstly it would save her life and secondly, although it was certain that amyloid would be deposited in the transplanted organs, I did not believe that there was any reason why this should not take as long to terminally damage them as it had from her birth, that is up to 30 years. Philip and I therefore referred Sandra to Harefield, the UK’s leading heart transplantation centre and they put her on the transplant list. Her condition continued to deteriorate and she was in grave kidney and heart failure, an extremely difficult and challenging situation to manage. However I was determined that she should get the chance that the transplants would provide and from April 1992 I phoned the heart transplant team, either Sir Magdi Yacoub or his colleagues, every single week, telling them of her desperate situation and the urgent need for transplantation, until finally we heard on 14 October 1992 that suitable donor organs had finally become available. While they rushed Sandra to the hospital, Professor Sir Magdi Yacoub, one of the world’s leading cardiac surgeons, and Professor Sir Peter Morris, the Regius Professor of Surgery at Oxford University, arrived to perform the operations. Two surgeons were needed, one for the heart and the other for the kidney. I arrived at Harefield at 11.30 pm to watch the operation and to receive Sandra’s old amyloid laden heart when it was removed to be replaced by the new healthy donor organ. They started with the heart transplant and Sir Magdi completed this uneventfully in 45 minutes, from start to finish. Amazing! Sir Peter then went to work on the kidney transplant which, in theory, is a very simple operation. However patients with systemic amyloidosis usually have amyloid in the walls of their blood vessels so that there is often much bleeding when they undergo operations, and this can be very difficult to control. Issue 4: June 2014 7 Indeed this was the case in Sandra and the kidney transplant was only completed at about 4 am the next morning. Quite an ordeal for Sir Peter and the whole team but fortunately no problem for Sandra! Sir Peter and I still remember it vividly whenever we meet but Sandra immediately had adequate kidney function and continued to have it until recently, 21 years later. As Sandra tells in her story, she has lived a full and rewarding life with reasonable quality, although complicated by the many unpleasant side effects of the drugs required to protect the transplants from rejection. She has just received a second kidney transplant from her sister and should continue to be well for many years to come. From the medical side, we have learned a lot from Sandra, both from her amyloid laden heart which was removed, and from her long and complicated clinical course. This knowledge has greatly benefited other patients. She was and still is a model patient and it has been a great pleasure to know her, and a privilege for Philip and me to have been able to look after her successfully. Despite this success story, amyloidosis of all types remains a serious unmet medical need. We badly need treatments that can eliminate the damaging amyloid deposits from the tissues and organs, so that organ failure requiring transplantation is no longer required. I have been working towards this since 1984 and finally, in 2005, invented a new approach which works very well in experimental models, eliminating massive amyloid loads from vital organs without having any adverse effects. GlaxoSmithKline, one of the world’s largest leading international pharmaceutical companies, licensed this invention in February 2009 and we have been working very closely with them to develop it for clinical testing since then. The first clinical trial, to show safety and tolerability of the treatment in amyloidosis patients, is currently in progress and the results so far, including in a patient with apoAI amyloidosis, are very encouraging. The process of drug development is extremely complex, extremely slow and extremely expensive, so it will be a while before we know for sure that our approach will be effective and safe, and can then become available for routine treatment. However we hope that in future, the combination of earlier diagnosis of amyloidosis, before there is irreversible organ damage, and availability of a treatment to eliminate existing amyloid deposits, may greatly improve the outlook for this serious disease. National Amyloidosis Centre News 8 Issue 4: June 2014 Fundraising News The Big McCycle 2014 — My Comeback Tour A 500 mile patient journey from Dunfermline to London to raise awareness and funds for the UCL Amyloidosis Research Fund By Mark McConway Two conversations in March 2011, separated by a fortnight, changed my life! Returning on the train to Scotland, I considered what I had been told about treatment and, for the first time since becoming ill, some of the clouds began to lift. Whilst there were no guarantees on offer, there was sufficient reason to be optimistic about the future. Yes, chemotherapy might be unpleasant but I pledged myself to ‘co-operating’ with the treatment fully and without complaint. I also pledged myself to getting well enough to ride my bicycle back to London for my appointment at the NAC two years hence. Mid-March 2011, Dunfermline at Queen Margaret Hospital, “The kidney biopsy has tested positive for amyloidosis. It’s a very rare and serious blood disease. In fact, it’s potentially life shortening. I’m sorry to tell you that it’s incurable at the moment.” “What do you mean by life-shortening?” “Without treatment, the average life expectancy is around 15 months. We're referring you to the National Amyloidosis Centre in London.” End of March 2011 at the NAC, Royal Free Hospital, Hampstead, London “There is a heavy load of amyloid present in your liver, kidneys, heart and spleen. It's systemic AL amyloidosis which means that it's being produced in your bone marrow. Whilst we can't offer you a cure, we are confident that we can halt the progress of the disease and treat the organs that have been affected. To get you back to ‘near normal’ will take a couple of years but you'll need to start chemotherapy straight away.” By the time that second conversation took place, my body was filled with fluid, my limbs and stomach were swollen, my cholesterol had gone through the roof at 25; I was being violently sick regularly and I could walk less than 50 feet without assistance or being pushed in a wheelchair. Given that my muscles had weakened to the extent that I couldn’t lift a few bath-towels without becoming exhausted – and I needed to sleep for several hours every day - the notion that I would be able to ride 500 miles in 24 months time seemed ridiculous to all but a few people who knew me. My fifth cycle of chemotherapy finished in July 2011. In October of that year, I did my first bike ride of 5 miles. Inevitably, it was exhausting – but fun. As the weeks went on, I increased the mileages and, within another few months, I could cycle 30-50 miles on a mountain bike in winter conditions, without distress. I decided that, with training, I could make the ride to the NAC in London in May 2013. At this stage, I floated the idea past my friend and cycling buddy, Tom McLucas, who had just recently retired from the fire service. He agreed to do it with me and we started training properly. Fate decreed that May 2013 would not be my time for doing the ride as I got a virus in December 2012 which laid me low until the start of April 2013. There was no time left to restart the interrupted training. Instead, I visited the NAC by train, as normal, in May and was told that there had only been a very small decrease in the amount of amyloid in my affected organs. Notwithstanding this, I felt hugely improved and was beginning to regain some much-needed muscle. National Amyloidosis Centre News Issue 4: June 2014 9 In order to keep the project alive for another twelve months, we resolved to continue the training, extending our 3-4 hour rides to 5-6 hours and spending the winter nights on turbo trainers in front of a projector screen with ‘Sufferfest’ training videos. Fast forward to February 2014. By this time, we had a name for our project - “The Big McCycle” - and had enlisted the support of my brother, Matt, who would become our logistics support with his van and ‘navigator of last resort’ with his collection of OS Maps. Early April saw our JustGiving site go live and we were in the final stages of preparation, getting bikes serviced, cycling tops printed and longer days in the saddle. Our Route We set out from Cairneyhill in Fife on April 29th and followed a scenic route down the East Coast of Scotland and North East England as far as South Shields, before heading inland towards York, then dropping South to Lincoln, Peterborough and ultimately, London. On arriving at the Royal Free Hospital, we were met by Professor Philip Hawkins. Along with his team at the NAC – and with Professor Sir Mark Pepys at the Wolfson Drug Discovery Unit – Professor Hawkins is at the forefront of the pioneering research to find a cure for amyloidosis. In summary, we cycled 507 miles (if you include the wrong turns, diversions, etc) in 6 days and 2 hours. The weather was mixed with us being shrouded in fog and battered by wind and rain on two days. We averaged 80 miles a day and had three long days of 11 hours each, where the weather, terrain and traffic made progress slow. Wherever we went, our printed cycling tops got people talking about amyloidosis and a few gave us ‘on the spot’ donations. We’ve raised £2,000 so far for the UCL Amyloidosis Research Fund, between on and off-line donations (www.justgiving.com/Mark-McConway) and the webpage remains open until the end of July 2014. Bespoke poems in aid of amyloidosis By Chloe Bullock I write bespoke poems for any occasion: birthdays, anniversaries, births, christenings, marriages, Mother's/Father's/Valentine's Day, farewells, memorial services, or anything else you like! I can also provide poems for use by organisations and causes for marketing purposes. I write the poems in exchange for a donation to the UCL Amyloidosis Research Fund. My mother suffers from amyloidosis, and I wanted to use my creativity in order to raise money for this charity on an on-going basis. My poems have always proved popular with friends and family, so I decided to widen my audience and raise some much-needed funds for this important cause at the same time. My poems are likely to bring a tear to your eye but will hopefully raise a smile too! How does it work? Contact me by email: hellobespokepoems@gmail.com then I will organise to get back in touch with you by Skype, email or phone to find out the exact nature and purpose of the poem you are looking for. I will ask for specific details about the person/organisation/occasion for which it is required in order to tailor it perfectly to your needs. Once I have enough information I will put pen to paper, then email/call you with the draft poem once it is ready. We can then tweak it together, according to your personal requirements. When you are happy with the finished article I ask that you make a donation via our page on justgiving.com of minimum £15 per poem. Once you have donated I will send you your poem by email. If you have a Facebook account type: "Bespoke poems in aid of amyloidosis" into the search bar. When you reach the page, click on "about" and you will find samples of my poems and reviews there. National Amyloidosis Centre News 10 Issue 4: June 2014 Channel distance swim for amyloidosis in Horsham pool By Pat Pinchin Those who know Martin Bolton-Smith well might have known a knee injury sustained during training for the Brighton Marathon in 2013 would not stop him from taking on a very different fundraising challenge for the UCL Amyloidosis Research Fund. Martin’s recent new challenge was closer to home in Horsham swimming pool. Martin, no stranger to starting intensive preparation for his sporting challenges from scratch, believes this was the toughest one yet. With his characteristic perseverance and determination, and with the help and advice of Alastair, his swimming instructor at Horsham Pool, Martin spent an arduous 6 months learning how to swim front crawl. This also involved learning correct breathing, stroke and turning techniques needed to swim the 22 miles distance of the English Channel (Dover to Calais) in 9 weeks, starting on December 2nd and finishing on January 30th. Martin had to build up his endurance and confidence too in order to complete the 120 x 25 metre lengths each week, 1408 in total. Just days into the challenge, Martin was already finding that the swim was the hardest challenge he had ever done both mentally and physically. There was nothing in the swimming pool to take his mind off how much it was hurting. Water, chlorine and walls of the pool are not in the least inspiring as compared with interesting countryside and cheery greetings from passers-by when out running. The words of a friend “EVERY STROKE IS A STROKE NEARER TO A CURE FOR AMYLOIDOSIS” helped keep Martin focused on the 40-45 minutes it took to cover the 64 lengths of each mile. In mid-January, with “the coast of France in sight” and just 12 miles left to go, Martin admitted that it took this venture to enable him to understand just how challenging long distance swimming is, but that this particular venture would be memorable for years to come. To his great relief, the countdown had begun and by now Martin was ticking off the days. On January 30th, 24 days ahead of his original 12 week schedule, Martin had completed his 22 miles, feeling a sense of deep satisfaction that this particular fundraising journey had been successful. Most importantly, he had also raised £804.00 for the UCL Amyloidosis Research Fund. Amyloidosis MRI Cycling Challenge: Land’s End to John O’Groats The Land’s End to John O’Groats (or End to End) is one of the classic long distance cycle challenges. It is called LEJOG if ridden north, and JOGLE if ridden south. There are many routes and it has been cycled, walked, hopped, roller-skated and even driven on lawn mowers! On the 6 July 2014 a team comprising staff and patients from the NAC, led by John Plant (patient), Thirusha Lane (Lead Nurse) and David Hutt (Lead Nuclear Medicine Technician), will be cycling from Land’s End to John O’Groats to help raise funds towards the purchase of an MRI scanner. This epic challenge will cover 977 miles, climbing 50,300 feet (almost twice the height of Mount Everest), arriving in John O’Groats 14 days later on the 19 July. National Amyloidosis Centre News Issue 4: June 2014 11 We have made great progress in developing new MRI techniques to specifically diagnose and quantify amyloid deposits non-invasively, crucially including amyloid within the heart, which has not been possible previously. This research is already facilitating the development of new treatments, and avoiding the need for potentially dangerous biopsies in many patients. Currently our patients have to travel to another London hospital to undergo MRI. We wish to create our own MRI facility in order to greatly reduce the travel burden and the waiting time involved, and to enable us to scan many more patients. How can you help? 1. Would you like to join the team for part of the ride? If so, contact John Plant (john.h.plant@gmail.com). There are still places available for people to join for a day or two. You don’t need a carbon fibre racing bike to join part of the ride - many have ridden successfully and comfortably on light hybrid bicycles. 2. Would you like to meet the team as it comes through major towns? This is where we really need the help of patients and relatives. Are you able to contact local media (newspapers, radio, and television) to raise interest? We would be happy to provide information or be interviewed. This will also give patients and relatives an opportunity to meet one another. If you are able to meet the team as they ride through a town near you, and if you would be happy to share your story, please get in touch. A few small media events have been set up but we still need more coverage in the bigger cities listed below. The more media coverage we can get the more people will become aware of amyloidosis and the work of the NAC. 3. Would you like to help by fundraising locally? You could organise a local event or appeal to local businesses. Some of our collaborators in the pharmaceutical and related industries (Isis Pharmaceuticals, Alnylam Pharmaceuticals and The Binding Site) have agreed to sponsor us and we will be happy to wear sponsor logos on our jerseys, in order to advertise. 5. Please sponsor us at our JustGiving page at http://www.justgiving.com/nac-mri-cycling-challenge. You can also text your donation by texting TDJP99, followed by the amount you wish to give (e.g. £10), to 70070. If you would prefer to send a cheque please make it payable to “UCL Amyloidosis Research Fund” and send it to Beth Jones at the address on the following page. Find out more about the Amyloidosis MRI Cycling Challenge and follow our blog at http://amyloidosismri.blogspot.co.uk/. We will be using a programme called Buddy Beacon which allows people to follow the ride. It uses GPS and updates every 20 minutes. There will be a link to this on the blog page. We will blog and upload pictures along the way, where possible. Interested people could follow the blog and send messages (which would be nice for the team!). We have also set up a twitter account (Thirusha Lane @lejog4amyloid) which we will attempt to update daily. The route in brief Day 1 2 3 4 5 6 7 8 9 10 11 12 13 14 / Date Start 6 July 7 July 8 July 9 July 10 July 11 July 12 July 13 July 14 July 15 July 16 July 17 July 18 July 19 July Land’s End Fowey Moretonhampstead Glastonbury Monmouth Clun Runcorn Conder Green Keswick Moffat Balloch Glencoe Inverness Lairg / The Crask Passes Penzance Ends St Austell Plymouth Exeter Taunton Wells / Chepstow Bristol / Tintern Hereford Shrewsbury Chester Warrington Bolton Lancaster / Ambleside Windermere Carlisle Gretna Glasgow Crianlarich Fort William Spean Bridge Bonar Bridges Altnaharra Thurso Fowey Moretonhampstead Glastonbury Monmouth Clun Runcorn Conder Green Keswick Moffat Balloch Glencoe Inverness Lairg / The Crask John O’Groats National Amyloidosis Centre News 12 Issue 4: June 2014 Donations To ensure that your donations go directly and exclusively to the NAC, please send directly to us or contact Beth Jones on 020 7433 2802 or beth.jones@ucl.ac.uk. All university based medical research depends on funds that are fought for in open competition (grants) from the Government-funded Medical Research Council and other charitable bodies. Their renewal depends on a successful research programme and the NAC has an excellent track record in this respect. However, there are constant shortfalls and every penny from other sources is received with sincere gratitude, and is used specifically and in its entirety for amyloidosis research. You can make an online donation at: http://www.ucl.ac.uk/amyloidosis/support-us or make a donation by post. A gift aid form is included here and is also available online or from: Beth Jones National Amyloidosis Centre Division of Medicine, Royal Free Campus University College London Rowland Hill Street London NW3 2PF UK UCL Medical School is part of University College London (UCL) which is a registered charity. Due to changes in the Budget nearly all gifts given to UCL now qualify for the Gift Aid Scheme. This increases the amount of the gift by 25% without any extra cost to the donor. It does so by allowing UCL to claim back the basic rate tax paid by the donor. To qualify for Gift Aid the donor must be a UK taxpayer and his/her combined income and capital gains tax bill must equal or exceed the amount UCL claims back on the gift. The gift can be for any amount and applies to one-off gifts and regular gifts made over a number of years. For UCL to claim the tax benefits the donor must make a "Gift Aid Declaration". One declaration will cover all future gifts and may be cancelled at any time. Cheques should be drawn in favour of "UCL Development Fund". This money is then transferred to the Amyloidosis Research Fund together with the reclaimed tax. If a donor does not qualify for the Gift Aid Scheme or does not wish to contribute in this way, cheques should be made payable to: "UCL Amyloidosis Research Fund". Newsletter funded by a bequest from Laura Lock