Document 13332911
advertisement
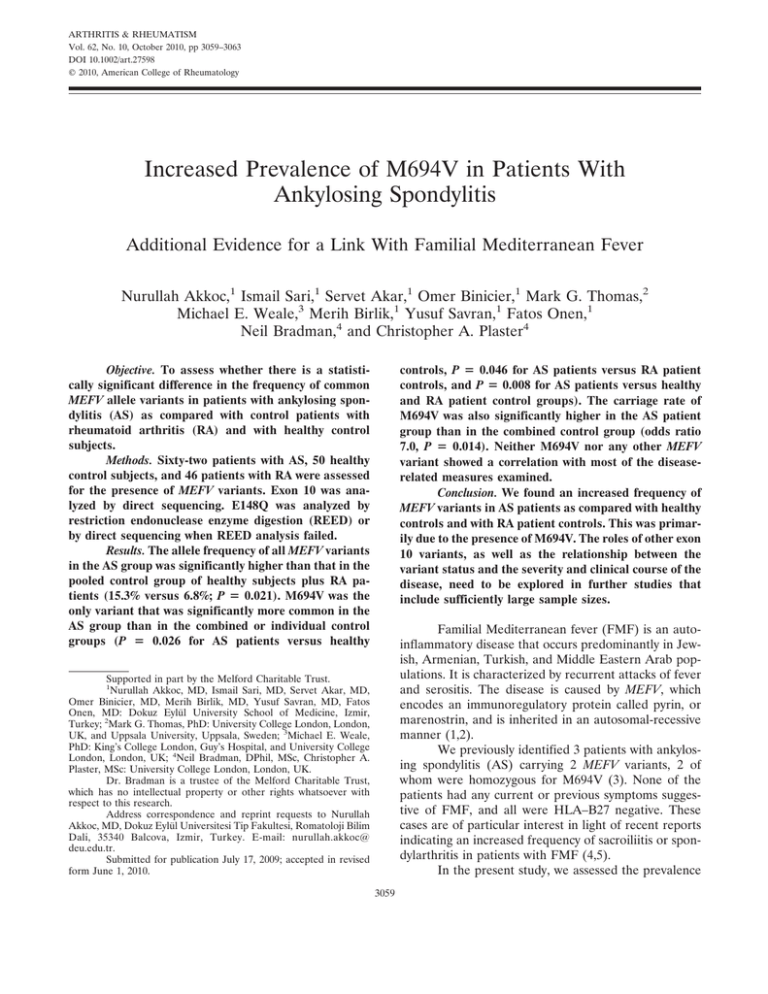
ARTHRITIS & RHEUMATISM Vol. 62, No. 10, October 2010, pp 3059–3063 DOI 10.1002/art.27598 © 2010, American College of Rheumatology Increased Prevalence of M694V in Patients With Ankylosing Spondylitis Additional Evidence for a Link With Familial Mediterranean Fever Nurullah Akkoc,1 Ismail Sari,1 Servet Akar,1 Omer Binicier,1 Mark G. Thomas,2 Michael E. Weale,3 Merih Birlik,1 Yusuf Savran,1 Fatos Onen,1 Neil Bradman,4 and Christopher A. Plaster4 controls, P ⴝ 0.046 for AS patients versus RA patient controls, and P ⴝ 0.008 for AS patients versus healthy and RA patient control groups). The carriage rate of M694V was also significantly higher in the AS patient group than in the combined control group (odds ratio 7.0, P ⴝ 0.014). Neither M694V nor any other MEFV variant showed a correlation with most of the diseaserelated measures examined. Conclusion. We found an increased frequency of MEFV variants in AS patients as compared with healthy controls and with RA patient controls. This was primarily due to the presence of M694V. The roles of other exon 10 variants, as well as the relationship between the variant status and the severity and clinical course of the disease, need to be explored in further studies that include sufficiently large sample sizes. Objective. To assess whether there is a statistically significant difference in the frequency of common MEFV allele variants in patients with ankylosing spondylitis (AS) as compared with control patients with rheumatoid arthritis (RA) and with healthy control subjects. Methods. Sixty-two patients with AS, 50 healthy control subjects, and 46 patients with RA were assessed for the presence of MEFV variants. Exon 10 was analyzed by direct sequencing. E148Q was analyzed by restriction endonuclease enzyme digestion (REED) or by direct sequencing when REED analysis failed. Results. The allele frequency of all MEFV variants in the AS group was significantly higher than that in the pooled control group of healthy subjects plus RA patients (15.3% versus 6.8%; P ⴝ 0.021). M694V was the only variant that was significantly more common in the AS group than in the combined or individual control groups (P ⴝ 0.026 for AS patients versus healthy Familial Mediterranean fever (FMF) is an autoinflammatory disease that occurs predominantly in Jewish, Armenian, Turkish, and Middle Eastern Arab populations. It is characterized by recurrent attacks of fever and serositis. The disease is caused by MEFV, which encodes an immunoregulatory protein called pyrin, or marenostrin, and is inherited in an autosomal-recessive manner (1,2). We previously identified 3 patients with ankylosing spondylitis (AS) carrying 2 MEFV variants, 2 of whom were homozygous for M694V (3). None of the patients had any current or previous symptoms suggestive of FMF, and all were HLA–B27 negative. These cases are of particular interest in light of recent reports indicating an increased frequency of sacroiliitis or spondylarthritis in patients with FMF (4,5). In the present study, we assessed the prevalence Supported in part by the Melford Charitable Trust. 1 Nurullah Akkoc, MD, Ismail Sari, MD, Servet Akar, MD, Omer Binicier, MD, Merih Birlik, MD, Yusuf Savran, MD, Fatos Onen, MD: Dokuz Eylül University School of Medicine, Izmir, Turkey; 2Mark G. Thomas, PhD: University College London, London, UK, and Uppsala University, Uppsala, Sweden; 3Michael E. Weale, PhD: King’s College London, Guy’s Hospital, and University College London, London, UK; 4Neil Bradman, DPhil, MSc, Christopher A. Plaster, MSc: University College London, London, UK. Dr. Bradman is a trustee of the Melford Charitable Trust, which has no intellectual property or other rights whatsoever with respect to this research. Address correspondence and reprint requests to Nurullah Akkoc, MD, Dokuz Eylül Universitesi Tip Fakultesi, Romatoloji Bilim Dali, 35340 Balcova, Izmir, Turkey. E-mail: nurullah.akkoc@ deu.edu.tr. Submitted for publication July 17, 2009; accepted in revised form June 1, 2010. 3059 3060 AKKOC ET AL of common MEFV variants (E148Q in exon 2 and exon 10 variants) and compared their frequencies in AS patients with those in healthy control subjects as well as in patients with a different inflammatory rheumatic disease. We also evaluated whether the variant status was correlated with clinical findings and disease-related measures. PATIENTS AND METHODS Selection of patients and controls. Sixty-four consecutive patients with AS diagnosed according to the modified New York criteria (6) were enrolled in the study. For comparison, 51 healthy control subjects and 46 disease controls with rheumatoid arthritis (RA) diagnosed according to the 1987 revised criteria of the American College of Rheumatology (formerly, the American Rheumatism Association) (7) were also included in the study. One AS patient (positive for M694V) and 1 RA patient (negative for MEFV variants) were excluded because they had first-degree relatives who were already enrolled in the study. The healthy control subjects were volunteers who had no history, symptoms, or signs of rheumatic disease. These subjects were recruited from blood donors, hospital staff, and another outpatient clinic associated with Dokuz Eylül University. None of the study subjects reported any symptoms suggestive of FMF, nor did any of them have a family history of FMF. All study subjects gave their informed consent to participate in the study, and ethics committee approval was obtained. Results of the baseline evaluations of the 62 AS patients (demographic, clinical, and laboratory features) are provided in Table 1. Genetic analysis. Peripheral venous blood (10 ml) was drawn into tubes containing EDTA and was stored at –20°C. MEFV exon 10 sequencing method. MEFV (exon 10) was amplified using the primers MEFV_Ex10B_U (5⬘TCCTTGTCTTTCCTTGTTGTCAG-3⬘) and MEFV_ Ex10C_L (5⬘-CGTGGGCACAGTAACTATTTTGT-3⬘). Se- Table 1. Baseline demographics and clinical features of the 62 study patients with ankylosing spondylitis* Age, mean ⫾ SD years Sex, no. male/female Disease duration, mean ⫾ SD years BASFI, mean ⫾ SD BASDAI, mean ⫾ SD Schober test, mean ⫾ SD cm Chest expansion, mean ⫾ SD cm Anti-TNF therapy, no. (%) of patients Uveitis, no. (%) of patients Hip prosthesis, no. (%) of patients HLA–B27 status, no. (%) of 45 patients tested Erythrocyte sedimentation rate, mm/hour C-reactive protein, mg/liter 42.8 ⫾ 12.5 41/21 10.9 ⫾ 7.2 4.4 ⫾ 2.5 3.4 ⫾ 2.2 2 ⫾ 1.5 3.5 ⫾ 1.5 16 (26) 7 (11) 4 (6) 37 (82) 46.4 ⫾ 28.4 45.7 ⫾ 55 * BASFI ⫽ Bath Ankylosing Spondylitis Functional Index; BASDAI ⫽ Bath Ankylosing Spondylitis Disease Activity Index; anti-TNF ⫽ anti–tumor necrosis factor. quencing was undertaken in both forward and reverse directions using the sequencing primers MEFV_Ex10U (5⬘TCCCTGTGCTCTCCCCTACCA-3⬘), and MEFV_Ex10Lseq (5⬘-GTCGGCATTCCGTGACTATT-3⬘), and the products were run on an ABI 3730xl DNA Analyzer (Applied Biosystems). Forward and reverse sequencing chromatograms were aligned with the human MEFV exon 10 Ensembl reference sequence using Sequencher 4.7 software (Gene Codes). A polymorphism was recognized if it appeared in both the forward and reverse sequences. Ambiguous chromatograms and nucleotides called from sequences in one direction that was not compatible with its complement in the other direction were resolved by reamplifying and resequencing the sample. If after 3 rounds of amplification and sequencing the genotype of the sample was unresolved, the sample was excluded. MEFV exon 2 E148Q genotyping assay and quality control. Polymerase chain reaction (PCR) amplification of a 277-bp fragment containing the E148Q polymorphism was performed by using the primers MEFV-EXON2-13F (5⬘ATCATTTTGCATCTGGTTGTCCTTCC-3⬘) and MEFVEXON2-17R (5⬘-GAGGCTTGCCCTGCGCG-3⬘). PCR products were digested by restriction enzyme Bst NI. Digestion product sizes were resolved by electrophoresis through a 3% agarose gel. Digestion of the 277-bp PCR product yields fragments of 160, 79, 21, and 17 bp if the G allele (glutamic acid codon) is present and fragments of 97, 79, 63, 21, and 17 bp if the C allele (glutamine codon) is present. To assess genotyping accuracy, 22 chromosomes (17 G and 5 C) were confirmed by sequencing. No errors in genotyping were observed. Samples that failed the initial E148Q restriction fragment length polymorphism assay more than 3 times had their genotypes determined by direct sequencing of the PCR fragment in both the forward and reverse directions (20 chromosomes), using the PCR primers on an ABI 3730xl DNA Analyzer. No differences in forward and reverse sequences were observed. One sample could not be successfully sequenced in either direction. Statistical analysis. A chi-square test or Fisher’s exact test was used, when appropriate, to asses the difference in the prevalence of MEFV variants between AS patients and healthy controls or RA patient controls. Odds ratios were calculated as a measure of the strength of the association. Spearman’s rho test was used to describe correlations. All P values were 2-tailed, and confidence intervals (CIs) were set at 95%. P values less than 0.05 were considered significant. RESULTS Genotyping of E148Q failed for 1 AS patient, and genotyping of exon 10 failed for 1 healthy control. Consequently, the statistical analysis was performed on the remaining 158 subjects with complete data for E148Q and exon 10: 62 AS patients (41 men and 21 women with a mean ⫾ SD age of 42.8 ⫾ 12.5 years), 46 RA patients (13 men and 33 women with a mean ⫾ SD age of 54.4 ⫾ 12 years), and 50 healthy controls (34 men and 16 women with a mean ⫾ SD age of 32.0 ⫾ 10.0 years). PREVALENCE OF M694V IN AS AND EVIDENCE OF A LINK WITH FMF 3061 Table 2. Distribution of MEFV variants in patients with AS as compared with control groups of healthy subjects and patients with RA* Controls No. homozygous or compound heterozygous E148Q/E148Q M694V/M694V M694V/M680I M680I/V726A M694V/E148Q No. heterozygous E148Q M694V V726A M680I(G/A) P760P K695R Total patients with MEFV gene variants AS patients (n ⫽ 62) Healthy subjects (n ⫽ 50) RA patients (n ⫽ 46) All controls (n ⫽ 96) 5 0 1 2 1 1 9 2 4 2 0 1 0 14 2 2 0 0 0 0 5 0 1 2 1 0 1 7 0 0 0 0 0 0 4 1 1 1 0 1 0 4 2 2 0 0 0 0 9 1 2 3 1 1 1 11 * AS ⫽ ankylosing spondylitis; RA ⫽ rheumatoid arthritis. The distribution of alleles according to disease status is shown in Table 2. There were 14 AS patients with 19 allelic variants, 4 RA patients with 4 allelic variants, and 7 healthy controls with 9 allelic variants. The prevalence of total allelic variants was significantly increased in the AS patient group in comparison with the RA control patients (P ⫽ 0.013, OR 3.98 [95% CI 1.31–12.14]) but not in comparison with the healthy controls (P ⫽ 0.222, OR 1.83 [95% CI 0.79–4.24]) (Table 3). The allele frequency of MEFV variants in the healthy control subjects as compared with the RA patient controls was very similar (P ⫽ 0.75); therefore, the AS group was also compared with the combined control group. AS patients had a significantly increased variant allele frequency as compared with the combined control groups (P ⫽ 0.021, OR 2.5 [95% CI 1.2–5.2]). There was also a significant excess of AS patients carrying 2 exon 10 variants as compared with the combined controls (P ⫽ 0.008) (Table 2). Analysis of individual variant rates revealed a significant increase in the frequency of M694V in the AS patient group as compared with the combined control groups (P ⫽ 0.008) or with the individual control groups (P ⫽ 0.026 versus healthy controls and P ⫽ 0.046 versus Table 3. Allele frequencies and carriage rates of MEFV variants in patients with AS as compared with control groups of healthy subjects and patients with RA Allele frequency, % E148Q M694V Other exon 10 variants Total exon 10 variants Total MEFV variants Carriage rate, % E148Q M694V Any exon 10 variants Total MEFV variants AS patients (n ⫽ 62) Healthy subjects (n ⫽ 50) P* RA patients (n ⫽ 46) P† All controls (n ⫽ 96) P‡ OR (95% CI)§ 2.4 7.3 5.6 12.9 15.3 4 1 4 5 9 0.703 0.026 0.758 0.063 0.222 1.1 1.1 2.2 3.3 4.3 0.638 0.046 0.307 0.015 0.013 2.6 1.0 3.1 4.2 6.8 0.99 0.008 0.385 0.008 0.021 0.9 (0.2–3.9) 7.4 (1.6–35) 1.9 (0.6–5.6) 3.4 (1.4–8.2) 2.5 (1.2–5.2) 4.8 12.9 19.4 22.6 4.0 2.0 10.0 14.0 0.99 0.041 0.196 0.331 2.2 2.2 6.5 8.7 0.635 0.075 0.089 0.069 3.1 2.1 8.3 11.5 0.68 0.014 0.052 0.075 1.6 (0.3–8.1) 7.0 (1.4–34) 2.6 (1–6.9) 2.3 (0.9–5.4) * For the comparison of ankylosing spondylitis (AS) patients versus healthy control subjects. † For the comparison of AS patients versus rheumatoid arthritis (RA) control patients. ‡ For the comparison of AS patients versus the combined group of controls. § Odds ratios (ORs) and 95% confidence intervals (95% CIs) are relative to the 2 control groups combined. 3062 AKKOC ET AL RA patient controls). The carriage rate of M694V was also higher in AS patients than in the combined control group (P ⫽ 0.014). The prevalence of other exon 10 variants and E148Q was not different between the patients and controls (P ⬎ 0.05). However, we noted that the power to detect individual variant effects was low because of the low numbers observed. The observed allele frequencies for individual variants in the combined control group ranged from 0.5% to 2.7%. Power calculations based on these observed control allele frequencies in 62 patients and 96 controls indicated that allelic odds ratios in the range of 4.1 to 11.2 are required to achieve 80% power. The observed allelic odds ratio for M694V was 7.4 (Table 3). The HLA–B27 status was available for 45 of the 62 AS patients, of whom 37 were B27 positive (82%). Sixteen AS patients had been treated with an anti-TNF agent (Table 1). Clinical and laboratory parameters did not correlate with the presence of MEFV variants (P ⬎ 0.05). DISCUSSION MEFV is located on chromosome 16p (1,2). Recent studies have indicated that pyrin participates in a complex interplay with the pyrin-domain protein superfamily and lipopolysaccharides via the Toll-like receptor family and procaspase 1 activation. Pyrin is implicated in the control of inflammation through leukocyte apoptosis and interleukin-1 and NF-B activation. Therefore, it may be speculated that MEFV might have a modifying effect on the expression of certain inflammatory diseases. Consistent with this hypothesis, MEFV variants have been reported to be associated with susceptibility to a number of inflammatory rheumatic disorders, such as Behçet’s disease (8) and palindromic rheumatism (9). In the present study, we found an increased prevalence of MEFV variants in AS patients in comparison with a pooled control group of healthy subjects and RA patients. RA patients were chosen to serve as controls, because the prevalence of MEFV variants in RA has previously been shown to be similar to that in healthy subjects (10), a finding that was confirmed in this study. The difference in the frequency of variants between AS patients and controls was a consequence of M694V, which was the only MEFV variant that was significantly more frequent in the AS patients than in the individual control groups or in the control groups combined. The allele frequency and the carriage rate of M694V in the AS group were 7.3% and 12.9%, respec- tively, which were significantly higher than the corresponding values in the pooled control group (1.0% and 2.1%, respectively). Other than M694V, our results did not reveal any significant difference in the prevalence of exon 10 variants between the AS patients and the controls. However, our sample size may not have been large enough to establish the contribution of other exon 10 variants, all of which are less common than M694V. It should be noted that the number of patients with any 2 exon 10 variants was significantly greater in the group with AS than in the combined control group. E148Q in exon 2 is the most common MEFV variant in healthy subjects in populations in which FMF is prevalent. However, some individuals who are homozygous for this variant are known to be disease-free, which was true for 2 of the healthy subjects included in this study. Thus, it is as yet unclear whether E148Q is a disease-causing variant with low penetrance or an allelic variant with no pathologic consequences (11). No significant difference in the frequency of E148Q between the AS patients and the controls was observed in this study. The presence of MEFV variants in AS patients has been evaluated in some recent studies from other regions of Turkey. One study from the middle region of Turkey analyzed the 8 most common MEFV variants and detected an increased M694V prevalence in a group of 95 AS patients (12). Unfortunately, that study did not include a control group, but the finding of a 23% carriage rate of M694V was markedly higher than the previously published 3% carriage rate of M694V in a Turkish population (13). One major concern about that study (12) is the very low prevalence of HLA–B27 in the patient population (32%). Moreover, 8% of the patients in that study had no evidence of radiologic sacroiliitis, even though the modified New York criteria were used as the case definition. Another study from the Black Sea region of Turkey revealed no significant difference in the frequency of MEFV variants between AS patients and unrelated, population-matched healthy controls (14). The statistical analysis, however, was based on all variants taken together, which led the investigators to miss a significantly higher frequency of M694V in the AS patients, with an OR of 3.9 (95% CI 1.03–14.75, P ⬍ 0.045) (15). A study from Istanbul (16) found a significantly higher prevalence of M694V in 193 AS patients as compared with 103 healthy controls (OR 4.73 [95% CI 1.39–16.12]). That study, which tested the same hypothesis in a different set of patients, provides independent PREVALENCE OF M694V IN AS AND EVIDENCE OF A LINK WITH FMF support for our study, the results of which, in isolation, may not be considered conclusive because of its small sample size and limited power. The relationship between the presence of an MEFV variant and clinical features was assessed in all 4 studies in Turkey (the present study and the above 3 studies), with somewhat contradictory results. However, these studies have low statistical power because of their small sample sizes and the low frequency of MEFV variants. Further studies with larger populations will be required to confirm these findings suggesting an association of M694V with AS and to clarify its influence on the disease course. Our findings are of particular interest in the context of the existing literature (mostly in the form of case reports) suggesting a link between AS and FMF. An increased frequency of sacroiliitis, which is a hallmark of AS, has been reported in different studies assessing patients with FMF. In the most recent study (4), sacroiliitis was found in 18 of the FMF patients (32.7%), but the most striking finding was a 94% prevalence of M694V in patients with sacroiliitis as compared with a 45% prevalence in those without sacroiliitis. The results of our present study, along with the published literature, indicate that M694V may be an additional susceptibility factor for AS. Its contribution to the development of AS will obviously be limited to populations that carry M694V. However, it should be noted that in some populations in which FMF is uncommon, some novel MEFV variants, such as P646L and L649P, have been identified among patients with seronegative polyarthropathies (9). In this particular study, 4 uncommon MEFV variants were detected with higher allele frequencies in patients with palindromic rheumatism than in either Spanish FMF patients or healthy subjects. It must also be borne in mind that MEFV may not be a susceptibility factor for AS, but could be in linkage disequilibrium with an unknown variant located close to exon 10 on chromosome 16p. Interestingly, in a study investigating genetic determinants of clinical manifestations of AS, Brown et al (17) found strong linkage with chromosome 16p and disease activity, as determined by the Bath Ankylosing Spondylitis Disease Activity Index. Future studies with sufficiently large sample sizes are needed to investigate the role of M694V and other MEFV variants in susceptibility to AS and the course of the disease. AUTHOR CONTRIBUTIONS All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved 3063 the final version to be published. Dr. Akkoc had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design. Akkoc, Sari, Onen, Bradman. Acquisition of data. Akkoc, Sari, Thomas, Binicier, Savran, Onen, Bradman, Plaster. Analysis and interpretation of data. Akkoc, Sari, Akar, Weale, Birlik, Onen, Bradman, Plaster. REFERENCES 1. French FMF Consortium. A candidate gene for familial Mediterranean fever. Nat Genet 1997;17:25–31. 2. International FMF Consortium. Ancient missense mutations in a new member of RoRet gene family are likely to cause familial Mediterranean fever. Cell 1997;90:797–807. 3. Akar S, Birlik M, Sari I, Onen F, Akkoc N. M694V mutation may have a role in susceptibility to ankylosing spondylitis. Rheumatol Int 2009;29:1259–60. 4. Kasifoglu T, Calisir C, Cansu DU, Korkmaz C. The frequency of sacroiliitis in familial Mediterranean fever and the role of HLAB27 and MEFV mutations in the development of sacroiliitis. Clin Rheumatol 2009;28:41–6. 5. Langevitz P, Livneh A, Zemer D, Shemer J, Mordechai P. Seronegative spondyloarthropathy in familial Mediterranean fever. Semin Arthritis Rheum 1997;27:67–72. 6. Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 1984;27:361–8. 7. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. 8. Touitou I, Magne X, Molinari N, Navarro A, Quellec AL, Picco P, et al. MEFV mutations in Behçet’s disease. Hum Mutat 2000;16:271–2. 9. Canete JD, Arostegui JI, Queiro R, Gratacos J, Hernandez MV, Larrosa M, et al. An unexpectedly high frequency of MEFV mutations in patients with anti–citrullinated protein antibody–negative palindromic rheumatism. Arthritis Rheum 2007;56:2784–8. 10. Rabinovich E, Livneh A, Langevitz P, Brezniak N, Shinar E, Pras M, et al. Severe disease in patients with rheumatoid arthritis carrying a mutation in the Mediterranean fever gene. Ann Rheum Dis 2005;64:1009–14. 11. Ben-Chetrit E, Lerer I, Malamud E, Domingo C, Abeliovich D. The E148Q mutation in the MEFV gene: is it a disease-causing mutation or a sequence variant? Hum Mutat 2000;15:385–6. 12. Cinar M, Dinc A, Simsek I, Erdem H, Koc B, Pay S, et al. The rate and significance of Mediterranean fever gene mutations in patients with ankylosing spondylitis: a three-month, longitudinal clinical study. Rheumatol Int 2008;29:37–42. 13. Yilmaz E, Ozen S, Balci B, Duzova A, Topaloglu R, Besbas N, et al. Mutation frequency of familial Mediterranean fever and evidence for a high carrier rate in the Turkish population. Eur J Hum Genet 2001;9:553–5. 14. Durmus D, Alayli G, Cengiz K, Yigit S, Canturk F, Bagci H. Clinical significance of MEFV mutations in ankylosing spondylitis. Joint Bone Spine 2009;76:260–4. 15. Akkoc N, Gul A. Comment on the article by Durmus, et al. Clinical significance of MEFV mutations in ankylosing spondylitis [letter]. Joint Bone Spine 2010;77:281. 16. Cosan F, Ustek D, Oku B, Duymaz-Tozkir J, Cakiris A, Abaci N, et al. Association of familial Mediterranean fever–related MEFV variations with ankylosing spondylitis. Arthritis Rheum. In press. 17. Brown MA, Brophy S, Bradbury L, Hamersma J, Timms A, Laval S, et al. Identification of major loci controlling clinical manifestations of ankylosing spondylitis. Arthritis Rheum 2003;48:2234–9.