Carl Nathan The public takes for granted that the phar-
advertisement
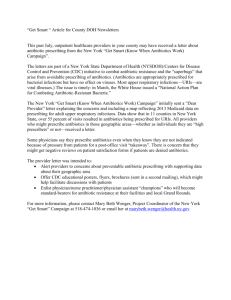
21.10 Commentary 899 NEW MH 18/10/04 3:50 pm Page 899 commentary Antibiotics at the crossroads The public takes for granted that the pharmaceutical industry can anticipate society’s medical needs and meet them. This faith is nowhere more evident than in the expectation that antibiotics are readily available to treat bacterial infections. After all, infectious diseases are the second-leading cause of death worldwide and the third-leading cause of death in economically advanced countries. But surprisingly, despite growing bacterial resistance to existing drugs, antibiotic development in the pharmaceutical industry is steeply declining (see chart, right)1–3. This new problem is converging with an old one — the scarcity of antibiotics to treat diseases prevalent mainly in poorer regions. The emerging crisis in wealthy nations and the long-standing crisis in poor nations result from the same causes — economic, regulatory and scientific — each exacerbated by the problem of antibiotic resistance. Government agencies and professional societies have addressed the latter problem3–6, but little has changed. We need new approaches, beginning with the recognition that the antibiotic crises of wealthy and poor nations are the same. The challenge is this: what can we do about the level of antibiotic research and development, which has long been insufficient to meet the needs of most populations, and now is plummeting? Causes of this decline are reviewed below, followed by ‘blue sky’ proposals for a more constructive approach to the permanent struggle with infectious disease. The focus is on drugs, but vaccination has a major role to play in reducing dependence on antibiotics. Economic pressures With respect to profit margins, financial markets hold the pharmaceutical business to a higher standard than almost any other industry. The demand for blockbuster drugs pressures companies to focus on long-term treatment of chronic conditions in preference to brief treatments for bacterial infections7. Most of the antibiotics that major firms make are designed for broadspectrum activity, so that they can be used by as many patients as possible. This shortens the market life of an antibiotic — as widespread use of an antibiotic hastens the emergence of resistance against it. To ward off resistance, physicians are urged to spare their use. With profits thus restrained in the medical arena, pharmaceutical firms send roughly half their antibiotic output to the The lack of new drugs leaves children in developing countries especially vulnerable to disease. Total number of new antibacterial agents 16 14 12 10 8 6 4 2 0 1983– 1988– 1993– 1998– 2003– 1987 1992 1997 2002 2004 food industry5. Pork, fowl, fish and dairy producers use antibiotics to maintain stock and foster growth. This selects for resistant bacteria, which can find their way into human populations — hastening the demise of the drug and making once-treatable infections incurable4–9. Industry’s retreat from developing new antibiotics is leading to a loss of expertise in both practical and theoretical aspects of antibiotic biology1. As industry reassigns or retires its microbiologists, academia will in turn train fewer5. When wealthy societies demand a resumption of antibiotic research,it will take years to rebuild the knowledge base. Better business models The Global Alliance for Tuberculosis Drug Development, a not-for-profit agency, is building a case to persuade industry that moderate profits can be made by developing NATURE | VOL 431 | 21 OCTOBER 2004 | www.nature.com/nature antibiotics for a disease prevalent in poor regions10. AstraZeneca has opened a research centre for anti-tuberculosis drug development in India (www.astrazenecaindia.com) and GlaxoSmithKline has assembled a team to work on drugs for tuberculosis and malaria (www.gsk.com/financial/reps02/CSR02/ GSKcsr-7.htm). Although these are positive steps, these initiatives are not enough to equip us to treat infections endemic in poor regions, nor do they address the emerging shortage of antibiotics for bacterial infections in wealthy nations. Academic scientists are making rapid advances in the chemical biology of infectious diseases. But they lack access to medicinal chemistry, pharmacology and the expertise to turn ‘hits’ into drug leads, or those leads into drugs. What is needed is a new player on the scene: a not-for-profit drug company. The profit sector could provide leadership. Encouraged by tax incentives,industry could give sabbaticals to its scientists and executives to work at a not-for-profit firm in rotation. Many in the pharmaceutical industry would like nothing better than to contribute personally to an endeavor in which their company (as a whole) is constrained from engaging. A not-for-profit firm could pursue research differently, protecting its intellectual property by filing patents, but also advertising its work openly,with the goal of licensing the intellectual property gratis to any company or agency that commits to produce and distribute the resulting drugs on a basis that would serve the needs of patients and society. For example, distribution in low-income markets could be on a for-cost basis whereas distribution in wealthy markets could remain for-profit. Biotechnology firms are beginning to ‘translate’ the ideas of academic researchers into drugs, but it is difficult for small firms to mount a world-class effort at medicinal chemistry and pharmacology, especially now that expertise in antibiotic development is scarce. A not-for-profit drug company could perform these services in exchange for a share of revenues from sales in highincome countries, coupled with a commitment that the drugs be distributed on a not-for-profit basis elsewhere. The best established way to delay the emergence of antibiotic resistance is to use one or more drugs in combination — known as combination therapy. A potential source of income for a not-for-profit, industry-supported drug company could there899 ©2004 Nature Publishing Group C. MOLLOY/SPL; SOURCE: CLIN. INFECT. DIS. Carl Nathan A. CRUMP, TDR, WHO/SPL Are we making the right choices to bring new drugs to the marketplace? 18/10/04 3:50 pm Page 900 I. MUKHERJEE/AFP/GETTY IMAGES 21.10 Commentary 899 NEW MH AstraZeneca's research operation in Bangalore brings much-needed investment and expertise to India in the search for anti-tuberculosis drugs. fore be contract work for private firms to identify effective drug combinations at an early stage. In fact, a not-for-profit firm could test the idea that shared knowledge allows early identification of targets (usually microbial enzymes) whose combined inhibition is lethal to the bacteria. The majority of the funding for a nonprofit firm would probably have to come from government and foundations. Tax incentives could encourage the for-profit sector to furnish services in kind or at cost, including equipment, supplies, chemicals, clinical development, and regulatory and legal services. Manufacturing could be contracted to factories in low- and middleincome countries. One can foresee many problems, such as back-flow of drugs from poor regions to wealthy ones. Such problems will be easier to manage than asking twenty-first century societies to accept nineteenth-century death rates from infection3. Regulatory obstacles Another major disincentive in the development of new antibiotics is the current system of regulatory requirements that discriminate against their approval1,5. In the United States, companies must demonstrate that a new antibiotic is superior to existing agents when used against infections caused by drug-sensitive strains. Existing agents are so effective against drug-sensitive strains that a new antibiotic is unlikely to be much better than an older one. Yet testing new antibiotics against infections caused by antibiotic-resistant bacteria is exceptionally difficult, as patients with serious drug-resistant infections have usually been treated with other antibiotics before resistance is documented. In short, the regulatory system is geared to generic standards of safety and efficacy — it makes no allowance for the specific case of antibiotic resistance. Companies have withdrawn from developing products against which they believe the regulatory system discriminates. Smarter regulations In agreement with recent recommendations3 of the Infectious Disease Society of America (see news feature on page 892), I believe regulatory requirements and patent incentives should be revised to encourage the pharmaceutical industry to develop new antibiotics. New antibiotics should be approved if they meet three tests. First, the safety profile is acceptable for the severity of the infection; second, the drug is effective in patients against antibiotic-sensitive bacteria; and third, the drug is effective in vitro against bacteria that are resistant to one or more existing antibiotics used to treat that infection. After a new antibiotic is approved, its clinical efficacy should be monitored in patients who are infected with bacteria resistant to previously approved antibiotics. This information should be posted on the Internet as it is collected. Unless new antibiotics are used in combination, resistance8 against them will quickly arise.A new pre-approval test should be developed for antibiotics intended to treat persistent or recurrent infections,such as tuberculosis and malaria, which require sustained administration.The manufacturer should run preclinical tests to determine how the new agent interacts with existing antibiotics used to treat that disease (one from each class).This information, combined with the drug’s pharmacokinetic profiles,should help regulators to develop new post-approval requirements for treating patients. First, the manufacturer should specify lists of agents, at least one of which should be used together with the new drug.Second,the manufacturer should monitor clinical efficacy and incidence of drug resistance when such combinations are used in practice. Patent life should be extended for antibiotics of new chemical classes directed at new targets2,analogous to US patent extensions for drugs developed to treat rare genetic diseases. In addition, all new antibiotics should be banned from widespread administration to healthy animals. It remains for the rest of the world to embrace an enforceable version of the ban enacted in the European Union in 1998 (ref. 6), or alternatively, to provide tax incentives with the same effect. Stalled science It would be simplistic to blame market forces and regulatory requirements alone for the antibiotic crisis. There is another and more surprising cause — industrial research and development has mainly produced variants of older antibiotics, when new drugs are sorely needed. Over the past few decades, only two new chemical entities have entered clinical practice as antibacterial agents, and only one whose target is in a new biochemical class1,2,8,9. It is surprising that the well has gone dry, despite heavy investment to dig it deeper using combinatorial chemistry and computational biology. Although genomic analyses are revealing hundreds of potential targets in pathogens, it remains a fact that almost all agents used to treat bacterial infections either have unknown enzymatic targets or target just four classes of enzymes — those involved in synthesis of protein, nucleic acids, cell walls or folate8. How did yield decline while knowledge grew and tools improved? NATURE | VOL 431 | 21 OCTOBER 2004 | www.nature.com/nature 900 ©2004 Nature Publishing Group 21.10 Commentary 899 NEW MH 18/10/04 3:50 pm Page 901 The answer may lie in a set of premises that were so successful that they hardened into dogmas. In a time of rapid intellectual expansion, dogmas are constraints. Fresh approaches There is no longer any reason to confine ourselves to drugs that inhibit the synthesis of protein, nucleic acids, cell walls and folate simply because such drugs have been so successful. We must find new microbial targets. First, synthesis offers too narrow a set of targets. Macromolecules such as DNA and protein have life cycles. Birth need not be the only point of intervention, as processing, repair and degradation are also points of vulnerability. This is the rationale behind efforts to target the proteasome in Overuse of antibiotics in livestock has led to an Mycobacterium tuberculosis12. increase in resistant bacterial strains. Another broad set of targets are the enzymes of core metabolism (intermediary conditions defining essentiality are multiple. metabolism, energy generation and For example, many infections, including micronutrient acquisition) in the bacteria. A tuberculosis, enter phases of latency — a third set of targets (overlapping the other state of equilibrium between the bacterium two) are the enzymes that enable the and the host response. The agents now used pathogen to resist the defences of the host. to treat tuberculosis kill rapidly growing After all, evolution has had more time than bacteria in culture within hours. In contrast, scientists to select chemicals to kill treatment of tuberculosis in people takes pathogens; the host has reactive oxygen at least 6–9 months of daily combination intermediates, reactive nitrogen intermedi- therapy, because the microbial targets that ates and pore-forming peptides in its arsenal. are essential in exponential growth phase Of course, evolution has also strengthened may not be so critical during latency or microbial defences against the host’s persistence5. chemistries. But we can aid the host’s Systematic studies in yeast teach us that immunity by using mutations in many antibiotics that disable genes are only pathogens’ resistance lethal when commechanisms12,13. bined with mutations in others16. This The goal of antibiotic development is is also true for inhibition of essential pathogens. We should enzymes — those the therefore target gene pathogen needs to surproducts which are vive. But survive essential together, where? Traditionally, even when they are tests to determine not essential individwhat enzymes are ually. For example, essential have been M. tuberculosis has in rich, highly two genes encodoxygenated culing isocitrate lyase ture medium. The enzymes, each of conditions facing Society’s ongoing struggle against infectious disease. which is capable of pathogens in the supporting lipid host during many infections — especially metabolism. Disruption of both genes in those that are persistent — can be drastically combination, but neither alone, causes rapid different from and more demanding than bacterial decline in vivo(J.McKinney,personal such conditions in vitro. Not only do meta- communication). Why not target both lyases bolic niches in vivo differ from culture broth at once? This idea will require fundamental in many ways (for example, in oxygen, iron, changes in scientific and regulatory pH and carbon source), but the immune approaches. First, antibiotic development system acts to suppress the pathogen’s repli- needs to be cooperative, not competitive — cation and damage many of its molecules. an approach that a not-for-profit drug comSuccessful pathogens adapt by expressing a pany could pursue using drug candidates different set of genes than they do in from different manufacturers. Second, when a culture14. Accordingly, a different repertoire successful combination therapy involves a of genes is essential in vivo than in vitro9,11,15. new unapproved drug, regulatory agencies In short, essentiality is conditional and the should allow approval of the combination to NATURE | VOL 431 | 21 OCTOBER 2004 | www.nature.com/nature proceed based on clinical tests of the combination itself, rather than insisting on approval for each individual component as they do now. Another premise that handicaps antibiotic development is that targets in the pathogen must have no equivalent (homologue) in the host. This is to avoid harming the host. Yet most classes of targets inhibited by antibiotics do have host homologues, except those involved in cell wall synthesis. It is time to abandon the premise.Contemporary structural, computational and chemical biology should be able to engineer compounds that can harm the pathogen without harming the host17. Conventional antibiotic development has reached an impasse, partly because it demands that new agents have broadspectrum activity. This imposes severe limitations, as targets must be widely conserved across pathogens — and even then only the most conserved subsites can be targeted. In contrast, it is medically preferable and will preserve the utility of the drugs longer, if antibiotics are highly specific, so that each one is used less often8. Treating infections with pathogen-specific rather than broad-spectrum antibiotics (whenever possible) will require prior,rapid, accurate and specific diagnosis. It makes no sense to use twenty-first century technology to develop drugs targeted at specific infections whose diagnosis is delayed by nineteenth-century methods. Advances in PCR, mass spectroscopy, quantum dot-enhanced immunoassays, nanotechnology, instrumentation and other technologies should be used to develop diagnostics. With further investment, doctors could expect to submit patient specimens (such as throat swabs, blood or urine) to analysis, and receive diagnoses in many cases within minutes to hours. Today, diagnosis usually takes a day or more. Without minimizing the challenge, we should acknowledge that pretreatment diagnosis is key to minimizing the use of broad-spectrum agents and keeping even in the endless race against drug resistance8. It is time to start applying new technologies to antibiotic development. Here are three examples. First, conventional gene disruption in the pathogen does not allow one to test the role of a gene during a given stage of infection, such as latency. If disruption of the gene precludes growth in vitro, then the gene-deficient mutant cannot be studied at all9. To determine whether a given target is essential in vivo we need ‘conditional gene inactivation’. This allows the investigator to turn a gene off at a particular time after infection has begun, and thereby model the effect of treating the infection with an antibiotic directed against the gene product. Second, we must not rely exclusively on screening chemical libraries against enzymes isolated from the bacteria. Although this 901 ©2004 Nature Publishing Group D. LEAH/SPL commentary 21.10 Commentary 899 NEW MH 18/10/04 3:50 pm Page 902 BSIP, CHASSNET/SPL P. DUMAS/EURELIOS/SPL commentary approach identifies chemical compounds that inhibit specific targets, it cannot reveal whether they would affect that target inside the bacterium, or even if they would get into the pathogen. We need to identify up front those compounds that can enter the bacterium and inhibit the target in its natural setting. For example, we could replace an endogenous gene encoding a potential target with a ‘conditional hypomorphic allele’, allowing reduction but not complete elimination of the target (which could kill it). Then we could screen chemical libraries to find compounds to which the ‘weakened’ mutant is particularly sensitive9. Third, innovative chemistry can allow us to find more potent inhibitors more quickly and cheaply. Drug development usually starts with inhibitors that work at nanomolar concentrations. Conventional screening of compounds rarely yields inhibitors active New approaches to screening chemical libraries below the micromolar range. It can take are needed to develop antibiotics. teams of chemists months to make a micromolar inhibitor a up and running. Each is thousand-fold more active. devoted to one or a small But the target enzyme number of infectious itself may be able to diseases. Their growing select weakly binding success22 suggests that compounds that are it is possible to mutually and covainvolve private lently reactive from industry in work two separate but comthat society needs, plementary chemical but the market does libraries.The enzyme not competitively can then catalyse their reward. covalent reaction into a One model, funded in single new compound that substantial part by the Bill inhibits the enzyme with higher and Melinda Gates Foundation affinity18. and the Rockefeller Foundation, Finally, we must exploit microbial diver- involves small, not-for-profit drug companies sity better. Many drug leads have been natur- that are virtual and physically distributed. The for Malaria Venture al products developed from one bacterial Medicines order, Actinomycetales19. But most of the (www.mmv.org) takes ideas, hits or leads, microbial universe remains unexplored, mainly from academic scientists, and uses a contract mechanism to fund because most microbial species medicinal chemistry and pharremain to be cultured. For “It makes no sense to example, studies of the use twenty-first century macology in the labs of other academics or pharmaceutical microbes in soil8,19 and water technology to develop firms21. Similar approaches are and the viruses that prey on drugs targeted at 20 them could reveal many com- specific infections, taken by the Global Alliance for Tuberculosis Drug Development pounds and enzymes that may whose diagnosis is (www.tballiance.org) and the help a given species compete delayed by nineteenthDrugs for Neglected Diseases with others in its environment. century methods.” Initiative (www.dndi.org)21. These natural products can teach us a great deal about microbial vulnerA second model of public–private abilities and how to exploit them. partnerships involves on-site research and development funded by a major pharmaceuImpossible? Think again tical company in conjunction with a public Is it hopelessly unrealistic to imagine partner, such as The Novartis Institute for not-for-profit drug companies working in a Tropical Diseases. This is funded jointly by smart regulatory environment, applying Novartis and the Singapore Economic Develfresh scientific approaches to antibiotic opment Board (www.nitd.novartis.com). A development? Perhaps the most challenging third model, also funded in substantial part aspect of this three-part vision is the notion by the Gates Foundation, is represented by of a not-for-profit drug company. Yet, at The Institute for OneWorld Health least three models of public–private partner- (www.oneworldhealth.org). This agency ships for development of anti-infectives21 are uses donated intellectual property to operate a small, on-site, not-for-profit drug company that prepares vaccines or drugs for malaria, leishmaniasis, trypanosomiasis, helminth infections and diarrhoeal diseases. Finally, the biotechnology industry appears to be positioning itself to contribute to the public–private partnership model through another Gates Foundation-funded initiative, BIO Ventures for Global Health (www.bvgh.org). All sectors of society, including the pharmaceutical industry, have a major stake in the control of infectious diseases, not only for medical reasons, but also for global economic development and security23. It is in the interest of both rich and poor societies that initiatives such as those described above grow by orders of magnitude and broaden their scope to include all major infectious diseases that the pharmaceutical industry does not adequately address. ■ Carl Nathan is in the Department of Microbiology & Immunology, Weill Cornell Medical College, and Programs in Immunology and Molecular Biology, Weill Graduate School of Medical Sciences of Cornell University, 1300 York Avenue, New York 10021, USA. 1. Projan, S. J. Curr. Opin. Microbiol. 6, 427–430 (2003). 2. Wenzel, R. P. N. Engl. J. Med. 351, 523–526 (2004). 3. Infectious Diseases Society of America. Bad Bugs, No Drugs; www.idsociety.org/Template.cfm?Section=Home&CONTENT ID=7455&TEMPLATE=/ContentManagement/ContentDisplay. cfm (2004). 4. Centers for Disease Control and Prevention. A Public Health Action Plan to Combat Antimicrobial Resistance; www.cdc.gov/drugresistance/actionplan/html/index.htm (2000). 5. Coates, A., Hu, Y., Bax, R. & Page, C. Nature Rev. Drug Discov. 1, 895–910 (2002). 6. World Health Organization Draft Global Strategy for the Containment of Antimicrobial Resistance ; www.who.int/ emc/amr.html (2001). 7. Service, R. F. Science 303, 1796–1799 (2004). 8. Walsh, C. Nature Rev. Microbiol. 1, 65–70 (2003). 9. Miesel, L., Greene, J. & Black, T. A. Nature Rev. Genet. 4, 442–456 (2003). 10. Global Alliance for Tuberculosis Drug Development. The Economics of TB Drug Development; www.tballiance.org/ 7_6D_Publications.asp (2001). 11. Chopra, I., Hodgson, J., Metcalf, B. & Poste, G. J. Am. Med. Assoc. 275, 401–403 (1996). 12. Darwin, K. H., Ehrt, S., Gutierrez-Ramos, J. C., Weich, N. & Nathan, C. F. Science 302, 1963–1966 (2003). 13. Bryk, R., Lima, C. D., Erdjument-Bromage, H., Tempst, P. & Nathan, C. Science 295, 1073–1077 (2002). 14. Schnappinger, D. et al. J. Exp. Med. 198, 693–704 (2003). 15. Sassetti, C. M., Boyd, D. H. & Rubin, E. J. Mol. Microbiol. 48, 77–84 (2003). 16. Tong, A. H. et al. Science 303, 808–813 (2004). 17. Fidock, D. A., Rosenthal, P. J., Croft, S. L., Brun, R. & Nwaka, S. Nature Rev. Drug Discov. 3, 509–520 (2004). 18. Manetsch, R. et al. J. Amer. Chem. Soc. 126, 12809–12819(2004). 19. Keller, M. & Zengler, K. Nature Rev. Microbiol. 2, 141–150 (2004). 20. Liu, J. et al. Nature Biotechnol. 22, 185–191 (2004). 21. Nwaka, S. & Ridley, R. G. Nature Rev. Drug Discov. 2, 919–928 (2003). 22. Vennerstrom, J. L. et al. Nature 430, 900–904 (2004). 23. World Health Organization, Commisssion on Macroeconomics and Health Macroeconomics and Health: Investing in Health for Economic Development; www.cmhealth.org (2001). Acknowledgements Thanks to A. Apt, K. Deitsch, H. Djaballah, B. Ganem, W. Jorgensen, T. Kapoor, M. MacCoss, V. Mizrahi, S. Projan, L. Quadri, K. Rhee, M. Rosenberg, D. Russell, D. Scheinberg, D. Schnappinger, D. Tan, T. Templeton and P. van Helden for stimulating discussions. Special thanks are due to P. Davies, S. Ehrt, M. Glickman, B. Kelly, J. McKinney and S. Nwaka. NATURE | VOL 431 | 21 OCTOBER 2004 | www.nature.com/nature 902 ©2004 Nature Publishing Group