Determining Correlation between IVC-CI and CVP in Hypotensive and Intubated
advertisement

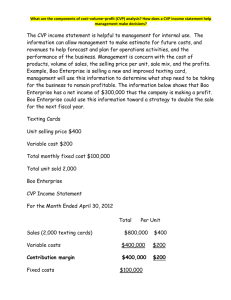
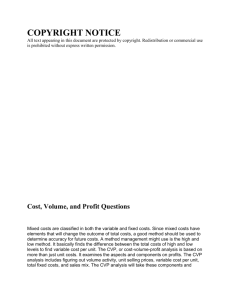
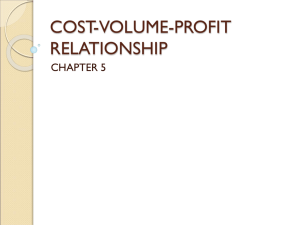
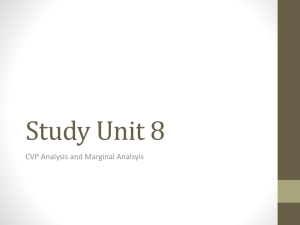
Determining Correlation between IVC-CI and CVP in Hypotensive and Intubated Patients with Central Lines David Price, M.D., Nicholas Stollenwerk, M.D. University of California, Davis Medical Center; Sacramento, CA BACKGROUND DISCUSSION Figure 2. Correlation between IVC-CI and CVP Figure 1. Linear Trendline with Increased CVP 80 70 60 50 r IVC-CI Assessing fluid status in ICU patients is challenging 1996 Connors shows mortality associated with routine use of pulmonary artery catheters IVC-CI determined by ultrasound offers a non-invasive alternative to assess fluid status CVP is an imprecise tool to assess fluid status Ultrasound is a cumbersome tool for routine use in the ICU The goal of this study is to assess correlation between IVC-CI and CVP in hypotensive and intubated patients to find range of CVP with maximal correlation to preclude need for ultrasound IVC-CI (%) RESULTS 40 30 20 STUDY DESIGN 10 0 0 5 10 15 20 25 30 > 12 8-12 <8 CVP CVP Patient identified by EMR search, talking to primary team, or while caring for ICU patients IMAGES CVP recorded at beginning of ultrasound evaluation Ultrasound evaluation performed by study authors Figure 3. Sub-Costal View of IVC Entering Right Atrium Figure 4. M-Mode View Showing IVC Max and Min Diameter AREAS FOR FUTURE STUDY Study authors review ultrasound images together within 24 hours to assess for image quality, correct anatomical structures, and measurement confirmation Pearson correlation coefficient used to determine correlation between CVP and IVC-CI Our study demonstrated a weak correlation between IVC-CI and CVP in hypotensive patients on mechanical ventilation with a CVP < 8 Strengths of Study: Literature on using ultrasound evaluation of IVC in this patient population is sparse. Study performed by intensivist and resident, not experienced echocardiographer, making results generalizable to MDs willing to learn ultrasound Weaknesses of Study: Sample size small Does not control for other variables such as mean airway pressure, PEEP, and cause of hypotension Intensivist and resident performing exams not certified in echocardiography Conclusion: As IVC-CI is a validated measurement of fluid status, our data shows that in hypotensive and intubated patients, clinician can trust their CVP more when the value is less than 8, but that in general CVP is an inaccurate tool for fluid assessment in this patient population. Future of this study Collect data on 74 patients Multivariable analysis accounting for effect of mean airway pressure, PEEP, and type of mechanical ventilation Calculate success rate of novice echocardiographers in obtaining adequate view to assess volume status. Does IVC-CI accurately predict volume responsiveness in septic patients throughout their hospital course? REFERENCES Bendjelid K, Romand J, et al. Journal of the American Society of Echocardiography. 2002;15,9: 944-949 Brennan J, Blair J, Goonewardena S, et al. J Am Soc Echocardiogr. 2007;20:857–861 Connors A, Speroff T, Dawson N, et al. JAMA. 1996;276:889–897 Dalen J, Bone RC. JAMA. 1996;276:916-918 Feissel M, Michard F. Intensive Care Medicine. 2004; 30,9: 1834-1837 Gunst M, Ghaemmaghami V, et al. Journal of Trauma-Injury Infection & Critical Care. 2008;65,3: 509-516 Jue J, Chung W, Schiller NB. J Am Soc Echocardiogr. 1992;5:613–619 Mitaka C, Nagura T, et al. Crit Care Med. 1989;17:205–210 Stawicki P, Braslow B, et al. Journal of the American College of Surgeons. 2009;209,1:55-61