The Elephant In The Room
advertisement
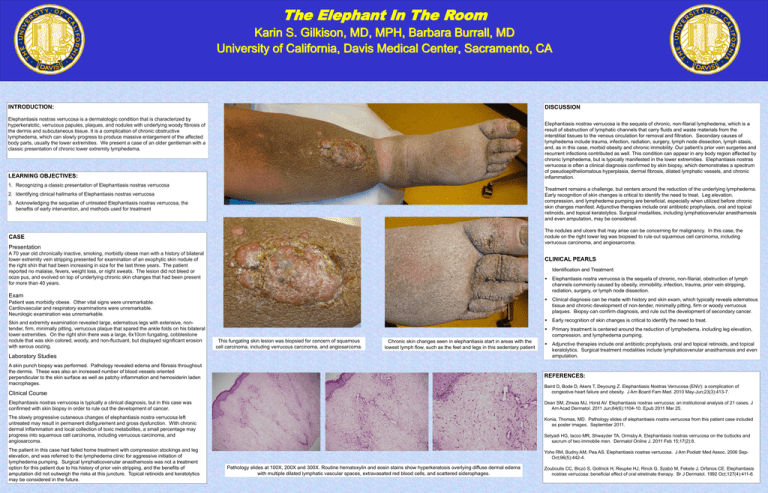
The Elephant In The Room Karin S. Gilkison, MD, MPH, Barbara Burrall, MD University of California, Davis Medical Center, Sacramento, CA INTRODUCTION: DISCUSSION Elephantiasis nostras verrucosa is a dermatologic condition that is characterized by hyperkeratotic, verrucous papules, plaques, and nodules with underlying woody fibrosis of the dermis and subcutaneous tissue. It is a complication of chronic obstructive lymphedema, which can slowly progress to produce massive enlargement of the affected body parts, usually the lower extremities. We present a case of an older gentleman with a classic presentation of chronic lower extremity lymphedema. Elephantiasis nostras verrucosa is the sequela of chronic, non-filarial lymphedema, which is a result of obstruction of lymphatic channels that carry fluids and waste materials from the interstitial tissues to the venous circulation for removal and filtration. Secondary causes of lymphedema include trauma, infection, radiation, surgery, lymph node dissection, lymph stasis, and, as in this case, morbid obesity and chronic immobility. Our patient’s prior vein surgeries and recurrent infections contributed as well. This condition can appear in any body region affected by chronic lymphedema, but is typically manifested in the lower extremities. Elephantiasis nostras verrucosa is often a clinical diagnosis confirmed by skin biopsy, which demonstrates a spectrum of pseudoepitheliomatous hyperplasia, dermal fibrosis, dilated lymphatic vessels, and chronic inflammation. LEARNING OBJECTIVES: 1. Recognizing a classic presentation of Elephantiasis nostras verrucosa 3. Acknowledging the sequelae of untreated Elephantiasis nostras verrucosa, the beneftis of early intervention, and methods used for treatment Treatment remains a challenge, but centers around the reduction of the underlying lymphedema. Early recognition of skin changes is critical to identify the need to treat. Leg elevation, compression, and lymphedema pumping are beneficial, especially when utilized before chronic skin changes manifest. Adjunctive therapies include oral antibiotic prophylaxis, oral and topical retinoids, and topical keratolytics. Surgical modalities, including lymphaticovenular anasthamosis and even amputation, may be considered. CASE The nodules and ulcers that may arise can be concerning for malignancy. In this case, the nodule on the right lower leg was biopsied to rule out squamous cell carcinoma, including verrucous carcinoma, and angiosarcoma. 2. Identifying clinical hallmarks of Elephantiasis nostras verrucosa Presentation A 70 year old chronically inactive, smoking, morbidly obese man with a history of bilateral lower extremity vein stripping presented for examination of an exophytic skin nodule of the right shin that had been increasing in size for the last three years. The patient reported no malaise, fevers, weight loss, or night sweats. The lesion did not bleed or ooze pus, and evolved on top of underlying chronic skin changes that had been present for more than 40 years. CLINICAL PEARLS Identification and Treatment Exam Patient was morbidly obese. Other vital signs were unremarkable. Cardiovascular and respiratory examinations were unremarkable. Neurologic examination was unremarkable. Skin and extremity examination revealed large, edematous legs with extensive, nontender, firm, minimally pitting, verrucous plaque that spared the ankle folds on his bilateral lower extremities. On the right shin there was a large, 6x10cm fungating, cobblestone nodule that was skin colored, woody, and non-fluctuant, but displayed significant erosion with serous oozing. This fungating skin lesion was biopsied for concern of squamous cell carcinoma, including verrucous carcinoma, and angiosarcoma. Chronic skin changes seen in elephantiasis start in areas with the lowest lymph flow, such as the feet and legs in this sedentary patient Laboratory Studies A skin punch biopsy was performed. Pathology revealed edema and fibrosis throughout the dermis. These was also an increased number of blood vessels oriented perpendicular to the skin surface as well as patchy inflammation and hemosiderin laden macrophages. Elephantiasis nostra verrucosa is the sequela of chronic, non-filarial, obstruction of lymph channels commonly caused by obesity, immobility, infection, trauma, prior vein stripping, radiation, surgery, or lymph node dissection. Clinical diagnosis can be made with history and skin exam, which typically reveals edematous tissue and chronic development of non-tender, minimally pitting, firm or woody verrucous plaques. Biopsy can confirm diagnosis, and rule out the development of secondary cancer. Early recognition of skin changes is critical to identify the need to treat. Primary treatment is centered around the reduction of lymphedema, including leg elevation, compression, and lymphedema pumping. Adjunctive therapies include oral antibiotic prophylaxis, oral and topical retinoids, and topical keratolytics. Surgical treatment modalities include lymphaticovenular anasthamosis and even amputation. REFERENCES: Clinical Course Baird D, Bode D, Akers T, Deyoung Z. Elephantiasis Nostras Verrucosa (ENV): a complication of congestive heart failure and obesity. J Am Board Fam Med. 2010 May-Jun;23(3):413-7. Elephantiasis nostras verrucosa is typically a clinical diagnosis, but in this case was confirmed with skin biopsy in order to rule out the development of cancer. Dean SM, Zirwas MJ, Horst AV. Elephantiasis nostras verrucosa: an institutional analysis of 21 cases. J Am Acad Dermatol. 2011 Jun;64(6):1104-10. Epub 2011 Mar 25. The slowly progressive cutaneous changes of elephantiasis nostra verrucosa left untreated may result in permanent disfigurement and gross dysfunction. With chronic dermal inflammation and local collection of toxic metabolites, a small percentage may progress into squamous cell carcinoma, including verrucous carcinoma, and angiosarcoma. Konia, Thomas, MD. Pathology slides of elephantiasis nostra verrucosa from this patient case included as poster images. September 2011. The patient in this case had failed home treatment with compression stockings and leg elevation, and was referred to the lymphedema clinic for aggressive initiation of lymphedema pumping. Surgical lymphaticovenular anasthamosis was not a treatment option for this patient due to his history of prior vein stripping, and the benefits of amputation did not outweigh the risks at this juncture. Topical retinoids and keratolytics may be considered in the future. Setyadi HG, Iacco MR, Shwayder TA, Ormsby A. Elephantiasis nostras verrucosa on the buttocks and sacrum of two immobile men. Dermatol Online J. 2011 Feb 15;17(2):8. Yoho RM, Budny AM, Pea AS. Elephantiasis nostras verrucosa. J Am Podiatr Med Assoc. 2006 SepOct;96(5):442-4. Pathology slides at 100X, 200X and 300X. Routine hematoxylin and eosin stains show hyperkeratosis overlying diffuse dermal edema with multiple dilated lymphatic vascular spaces, extravasated red blood cells, and scattered siderophages. Zouboulis CC, Biczó S, Gollnick H, Reupke HJ, Rinck G, Szabó M, Fekete J, Orfanos CE. Elephantiasis nostras verrucosa: beneficial effect of oral etretinate therapy. Br J Dermatol. 1992 Oct;127(4):411-6.