Board of Directors Meeting in Public 30 October 2014
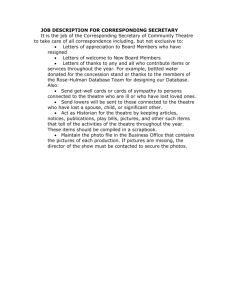
advertisement

Board of Directors Meeting in Public 30 October 2014 Board of Directors’ Meeting - In Public 30 October 2014 at 9:00am Education Centre AGENDA Item Item No. 14.214 Outcome Report type Apologies for absence Note Verbal 14.215 Declarations of interest Note Verbal 14.216 Minutes of public Board meeting 30 September 2014 Approve Enc 01 14.217 Matters arising from public Board meeting 30 September 2014 Note Verbal Quality Report Note Vin Diwakar, Chief Medical Officer and Michelle McLoughlin, Chief Nursing Officer Performance Report Note David Melbourne, Deputy Chief Executive & Chief Finance Officer Resources Report Note David Melbourne Deputy Chief Executive & Chief Finance Officer and Theresa Nelson, Chief Officer for Workforce Development Strategy Enc 02 Reflection and Review of our IT Strategy Adam Carson, Associate Director, ICT & PMO Transforming our Pathways of Care David Melbourne, Deputy Chief Executive / Chief Officer for Finance, Nick Barlow and Lucas Mol, Newton Executive Update and Issues Note Presentation Note Enc 05 Presentation Chief Executive’s Report Sarah-Jane Marsh, Chief Executive Chairman’s Report Christine Braddock, Chair Note Verbal Note Verbal Note Verbal Quality & Resources 14.218 14.219 14.220 14.221 14.222 14.223 14.224 Enc 03 Enc 04 AOB 14.225 Questions from members of the public BREAK 10.25 – 10.40 Next meeting of the Board of Directors: 27 November 2014, TBC UNCONFIRMED Item 14.216 Enc 01 BOARD OF DIRECTORS MEETING Minutes of the meeting held in public on 30 September 2014 at 09.00 in the Education Centre, Birmingham Children’s Hospital Present Attending Ref. 14.188 Christine Braddock Keith Lester Sarah-Jane Marsh Vin Diwakar Jon Glasby Colin Horwath Michelle McLoughlin Tim Atack David Melbourne Theresa Nelson Judith Smith Roger Peace Elaine Simpson Matthew Boazman Deborah Bannister Rebecca Alton CB KL SJM VD JG CH MM TA DM TN JS RP ES MB DB RA Chairman – Chair for the meeting Non-Executive Chief Executive Officer Chief Medical Officer Non-Executive Director Non-Executive Director Chief Nursing Officer Chief Operating Officer Deputy CEO and Chief Finance Officer Chief Officer for Workforce Development Non-Executive Director Non-Executive Director Non-Executive Director Director of Strategy and Planning Interim Company Secretary Executive Assistant to the Chairman, NEDs and Governors Item Action Apologies for absence No apologies for absence 14.189 Declarations of interest There were no declarations of interest. 14.190 Minutes of the Board meeting held in public on 31 July 2014 The minutes of the meeting held in public on 31 July 2014 were agreed as an accurate record, subject to removing Judith Smith from being in attendance. 14.191 Matters arising from the Board meeting held in public on 31 July 2014 There were no matters arising not covered by the agenda. 14.192 Chairman’s Report CB reported verbally as follows: • Joint development with the Birmingham Women’s Hospital (BWH) A number of meetings have been held looking at how the development will move forward and a lot of progress has been made. The joint development will come up through the business of the meeting today. • University Hospitals Birmingham NHS Foundation Trust (UHB) We have also been engaged quite heavily with UHB and BWH, in terms of looking at interconnections and work we can do together. We are now involved in a transport Page 1 of 10 UNCONFIRMED Item 14.216 Enc 01 Ref. 14.193 Item infrastructure development around the Edgbaston site. A lot of work has been undertaken, particularly trying to get the LEPS involved in understanding the implications of the transport infrastructure. • InTent This event which focussed on ‘Caring for Team BCH’ was hugely successful and was well attended by a good cross section of trust staff. SJM will discuss in more detail. • AGM One of the outcomes from the AGM in July was that the governors identified they wanted to host an informal session to look at their own development and their priorities going forward. This informal session took place on 18 September 2014 and a list of priorities have been identified. An Away Day is likely to be arranged for the governors before the end of the year. The governors are keen to get involved as they still do not feel as involved as they could be. • Well Led Board Over the summer, the board have moved forward with the self-assessment process and well led board development. Deloitte have now been appointed to work with us to complete the full process. They are clear that we are looking for an innovative and developmental review with the clear aim of improvement in the future. Once the review starts in January, it will take about 8 weeks to complete, depending on Deloitte’s access to the right people and documentation. The Board noted the verbal report. Chief Executive’s Report SJM reported verbally as follows: • InTent week – ‘Caring for Team BCH’ The idea behind the theme for InTent week came from the fact that we know the hospital is busier than ever before and this will continue into the future. We are reliant on staff working very hard day in day out to deliver our services. We need to help to support our staff to be as resilient as they possibly can, not just in the face of increased activity but also in the face of the complexity of some of the children we look after. We wanted to do this in practical ways so we; held focus groups for any members of staff, obtained input from an organisation called Chimp Management, held a leaders day and human factors training. The week was well received. 900 staff took part in the focus groups and 120 staff came to the leaders day. There have been some lovely stories since of people putting the things they had learnt into action, for example the theatre team are undertaking the 30 day appreciation challenge. The staff were challenged to think for themselves differently and not to wait for Page 2 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item management before putting good ideas into action. JS commented that she was encouraged by the next generation of consultant staff getting enthused about human factors. JG commented on the atmosphere which was warm, engaged and relaxed. People were talking about small things that were making a big difference, which was quite humbling. TN added that there had been a real emphasis on the staff taking care of themselves as a precursor to taking better care of patients. A focus next year will be on trying to engage with the staff that did not attend InTent this year to try and achieve even greater participation. • Internal Visits Lord Warner attended InTent week to look at how we engage with our staff. He is currently reviewing safeguarding and visited our Emergency Department and talked to staff there about the Multi-Agency Safeguarding Hub and how we approach safeguarding in the hospital. He spoke to MM and SJM about some of our ideas as to how we move the governance around safeguarding forward. It was good opportunity to influence some of things he might say around health in his review. • Una O'Brien, Permanent Secretary of the Department of Health, visited to look at staff engagement and complaints. SJM was also able to discuss funding of the new hospital project and how we have been able to identify alternative funding streams. She was able to discuss what help and support the DoH might be able to provide. • Lord Willis is currently reviewing the shape of caring on behalf of NHS England, which is particularly focused on nursing from education onwards. He is looking into how we get the workforce we need for the future (the next 10 to 15 years). He met with a whole range of staff and got to test out some of his ideas on them. His report will be published in February 2015. • • External Visits Vitality Partnership. DM and SJM visited the Vitality Partnership, a GP partnership operating in the West Birmingham area to look at ways of delivering primary care. It provided an opportunity to think about how we might develop some links, especially around the new hospital development and CAMHS. It also allowed us to consider how the shape of primary care might change across Birmingham. Royal Orthopaedic Hospital (ROH). SJM went on a partnership visit to ROH to discuss where they see themselves in 5 – 10 years time. The main players in specialised services in Birmingham are endeavouring to strategically come together on the same campus site but ROH are not part of that group. ROH have significant service overlap with us and UHB and we need to consider how this can work best in the future. Page 3 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item • Events • National Conference on Paediatric Palliative Care Systems. People from all over the country came to look at the systems and processes we use to plan around palliative care, and also the emotional well being of staff who deliver that service. Over 100 people were involved in this conference which took place last week. • Annual Memorial Walk and Picnic at the National Memorial Arboretum • KIDS 5th Birthday Party • ‘All About Play’ launched • Opening of new Ward 9, which has been refurbished at a cost of around £350,000 over the summer • Flu Campaign launched. Last year 86% off staff had the flu jab, which was one of the highest percentages in the NHS. It is important for us to protect ourselves and the children who cannot protect themselves. This campaign is going to be heavily pushed again this year and we are aiming to beat the % of our staff who were immunised last year. It is not just about the staff in patient facing roles, every member of staff is always two steps removed from a patient. The Board noted the verbal report. STRATEGY 14.194 Monitoring Mortality at BCH JM presented to the Board. Mortality is monitored to: • Enable us to measure the quality of care we deliver. • Enable comparison between institutions. • Help us to learn as individuals, as department and as an organisation. There is no perfect way of monitoring mortality, particularly in a children’s hospital. There are a relatively small number of deaths at BCH and we look at them in a number of different ways, including: • • • • • Absolute number of deaths Deaths per 1000 admissions PICANet Data (PICU Deaths only) Cumulative sum charts Hospital Standardised Mortality Ratio (HSMR) At BCH we investigate all deaths individually anyway. The figures above can act as triggers and Page 4 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item allow us to be able to cross check / triangulate any potential difficulties. Absolute number of deaths and Inpatient Deaths/1000 Admissions This looks at crude mortality and is very basic. There are no adjustments to the data to take into account specific factors such as co morbidities. The only adjustment that can be made is to standardise the data to link the number of deaths per 1000 admisisons. PICU Deaths In PICU there is a more complicated way of looking at mortality. Data is collected on every patient that is treated in PICU, using PIM2r. This data collected on first contact and includes: • A number of clinical metrics, to give an idea of how sick the patient is when they arrive • Reason for admission and whether it is elective • High and low risk diagnoses The data is submitted to PICANet to produce an annual report. This data is collated into charts and graphs, which enables us to compare ourselves with other units. In the most recent annual report, it is clear that we are the biggest single intensive care unit in the UK. If the hospital is plotted on the graph below the line, this represents an excess of survivors. If it sits above the line, there is an excess of deaths. With appropriate adjustment, BCH sits within the funnel plot. There are a number of problems: • A report is only produced annually • 30% of deaths occur on wards, so PICANet only looks at 70% of our deaths • It only looks at the patient on first PICU contact. PIM data does not tell us if we managed these patients appropriately before PICU admission. Cumulative Sum Charts (CUSUM) CUSUM charts provide real time data. These charts are replicated in the quality report. The black line on the graph represents cumulative excess deaths and the purple line represents cumulative excess survivors. If the black line starts to climb, this indicates that more patients are dying then we would expect. The risk adjusted models that we use change over time. PIM2r has been mentioned, but we are now actually onto PIM3r, which has been risk adjusted to take into account the developments and improvements in care. There are some patients that we would expect to survive today that would not have survived five years ago. This data is monitored in real time, so we have a much earlier warning if there are any concerns. If there is a spike in the data, this can trigger an investigation but it may also mean that the tool needs to be re-calibrated. CB asked about palliative care and where the statistic sits if the patient dies at home or in a hospice. MM commented that if the child or young person dies in their own home, it will come under the community data although there will be a link through to us. VD commented that in the individual reports of every patient who had died, we looked into whether the patient was appropriately offered palliative care. Cardiac Deaths Page 5 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item Deaths from cardiac causes accounts for the largest number of deaths by speciality therefore there is additional monitoring in place for this. The data only takes into account a specific procedure only and does not take into account other co-morbidities. The VLAD chart takes into account more variables. There are no control limits on this graph. If the line on the graph goes up, this is good. If the line goes down, this is bad. There are a number of downward moves recently and the cardiac department have confirmed from the data that they do not think this is statistically significant. This has acted as a trigger and all of these deaths will be reviewed at Cardiac M&M. VD explained that the “gold standard” for looking at deaths is individual case review. This happens in ICU and cardiac, and the two units do challenge each other. We have an overall trust wide mortality system that looks for specific triggers and then there are the statistical systems which compare ourselves to other units nationally. When there is no perfect statistic, the best way to look at it is from as many different angles as you can. HSMR This has been around since 2001, allowing for comparison between institutions. It is based on routinely collected administration data. It is the ratio of observed to expected deaths. This is risk adjusted for diagnosis only. This index is based on adult data, so there is essentially no risk adjustment for paediatrics. It is therefore largely meaningless. JG asked why this data was reported to board every month if it is meaningless. JM said that there was no value in reporting it to the Board, as even the institutions we try to compare ourselves too are very different to ours. JG queried whether we are therefore getting false assurance. VD commented that it would be difficult to defend taking this report out, as every other Trust reports it. TA confirmed that the CQC and regulators review this chart. KL added that this chart is in the public domain and he wants to see what everyone else sees. VD advised that work is ongoing with Jacqueline Cornish, National Clinical Director for Children and Young People. She has asked us to produce a national system for specialist children hospitals to produce a standard system. She will work with Sir Bruce Keogh, Medical Director for NHS England, so there is an agreement about what all of these Trust’s will actually use. All of the children’s hospitals in the North of England have been looked at and we are gradually working around the South trusts; this will be discussed at the Children’s Hospital Alliance on Friday. External Reviews There are various external reviews which provide the hospital with reassurance: • All BMT patients get discussed at a national level at an annual meeting • GOSH are invited to look through our cases • Coroner • Child Death Overview Panel, which reviews all unexpected deaths Way Forward There is a need to develop something that can compare us to other organisations. Alder Hay are keen to work with us on this. Using our MIST safety data collaborative we will be working with them to take this forward. CH commented that it is correct that we focus on survivability, however is the quality of life of Page 6 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. 14.195 Item the patient considered. Is the hospital assured that the patient has had the best possible outcome? VD explained that this is a big challenge and we do have some information/data. In terms of outcomes, there is work going on nationally. It is not at the level of maturity for Board time to be dedicated to it yet; however the liver and cardiac unit have published work which can be reported back to the Board if desired. From our work with the Children’s and Young Persons Outcome Form we strongly believe that a child’s school number and NHS number should be the same, so good work can be done in comparing educational outcomes with health outcomes. The Board noted and received the presentation. Next Generation Project – Update on the Management Restructure TN updated the Board. There are four key streams to the Next Generation Project: • • • • New facilities Patient pathways IT strategy People There are four main elements to the Next Generation – People Project: • • • • Clinical Groupings and Leadership Structure A revised Accountability & Leadership Culture Transformation of pathways and therefore new roles required Provision of more productive workforce for the new clinical block The focus today will be on clinical groupings and leadership structure and a revised accountability and leadership structure. The impact of changing a leadership structure can be quite significant, it is therefore important as to how we engage and communicate with people throughout the process. Why change the leadership structure? Operational • Lack of seamless decision making across directorates causing delays in service improvement e.g. play, pre-admission • Devolution of decision making to the front line. • Clinical synergies not exploited to manage resources better Strategic • Failing to develop future clinical leaders – current roles are too big and complex • Executives involved in day to day operational issues too regularly, impacting on leadership accountability and development • Timing never perfect so important to make changes from a position of strength What work has been done so far? Before the consultation was launched at the end of June, we went through three months of engaging with our people. TA added that during this pre consultation phase the initial set of Page 7 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item clinical groupings was changed quite significantly to reflect conversations with the consultants. TA felt confident the clinical body felt fully involved and part of the consultation. We have worked hard on POC (programmes of care). These are pathways which cut across all clinical groupings. VD and his team have developed a process to bring teams together to manage the POC more efficiently. This was a fundamental principle from the critical care summit. Clinical Groupings There are seven main groupings. Each group is led by a clinician. The POC will work across each of these. A complexity tool has been designed to work out the leadership structure for each of these groupings. The change in structure is cost neutral. ES asked where ‘Play’ now sits as it used to be with Clinical Psychology. MM explained that in the new structure it sits in surgery and MM will still have oversight. VD explained that the groupings represent the key areas that the Board have identified as a priority and achieves what clinicians have asked for. Working Example This surgical pathway follows the path of the majority of children who are admitted for elective care. Current Directorate Structure Revised Clinical Groupings and Structure Child admitted into SDC which is managed by Clinical Support Now all departments in the one Child goes to Theatre which is managed by directorate making improvements to the surgical pathway much clearer. Specialised Services Child is operated on by a surgeon who is managed by Surgery Return to ward either SDC or surgical ward which is managed by CS or SS Under the current structure the patient would be managed by a number of directorates and where there is a blockage in the system, this is much more difficult to resolve. Under the new structure the patient is treated by the same directorate throughout. Operational Reporting Structure The Deputy Chief Nursing Officer, Deputy Chief Medical Officer and the new Deputy Chief Operating Officer, will be the three people involved in the daily operation of the organisation. Their roles are focused on facilitating and unblocking pathways. They will report to TA on a dya to day basis, but their professional accountability will remain with VD and MM. One of the key pieces of feedback from our staff was a request not to implement these changes during the winter which is a difficult time. Therefore, a decision has been made to fully implement from April 2015, but staff will be moved into their new posts over the next few weeks. How do we map our governance through to the Board? The Board need to consider: Page 8 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item • • • • If we are going to empower local clinical decision making how do we need to be different both at board and committee level – culture, challenge, assurance etc How do we ensure quality remains our guiding principle throughout How do we use information as a change agent How does the scheme of delegation and accountability framework support growth of our trust leaders The scheme of delegation and accountability framework will be subject to scrutiny by the Audit Committee next month. CB commented that an enormous amount of time had obviously been invested into the development of the restructure over a long period of time. There was discussion as to whether the NEDs were as sighted on this work as the executive team or as sighted as they needed to be at this stage. Overall, the development of this work has been through the correct processes but as it is such an important piece of work CB will consider with the NEDs whether this subject needed greater board time in the future. The issue will be considered by CB and the NEDs at their NED meeting and they will feed back to TN if they would like the matter brought back to board at this stage. It will inevitably come back as the implementation progresses in due course. The Board noted the presentation. QUALITY & RESOURCES 14.196 Quality Report JG commented that both quality reports were looked at in detail in Quality Committee last week. There were a couple of items that the committee focused on: • The changes in our position around mortality and the situation around cardiac, which JM has today covered this already in great detail. • The programme of work around breast feeding. This is a possible theme that Quality Committee may want to look at in the coming year. • Work around outliers. The Committee had been assured at the approach taken and that the Trust had pro-actively spotted it as a potential theme/issue, without having any concrete data. The Committee were also assured by the actions taken. • SJM and JG are meeting with the Chair of the Safeguarding Children Board tomorrow to discuss the role of the hospital in the broader city and the community. 14.197 The Board noted the report. Performance Report The Board noted the report. 14.198 Resources Report The Board noted the report. OTHER 14.199 Questions from the Public Carl Harris (staff governor) commented that in terms of leadership development, allied health professionals are keen to be part of the change. TN acknowledged this enthusiasm and Page 9 of 10 Action UNCONFIRMED Item 14.216 Enc 01 Ref. Item explained that the changes will afford them the opportunity to lead a directorate. Next Board Meeting: 30 October 2014, The Education Centre, BCH Page 10 of 10 Action Board of Directors Item 14.218 Report Title Sponsoring Directors Contributors Previously considered by 30th October 2014 Enc 02 Quality Report Dr Vin Diwakar, Chief Medical Officer & Michelle McLoughlin, Chief Nursing Officer Governance Services, Corporate Nursing, Education, Infection Prevention and Control, PICU & Cardiac Services SLT & CRAQA Situation The enclosed report provides an update on key clinical safety and quality topics. Background The report is collated from a number of information sources and provides assurance that key risks are being escalated and monitored until sufficient action has been taken to address the concerns. The report includes information on key risks, serious incidents, mortality data, cardiac arrest, respiratory arrest, other acute life threatening events, infection control data, Safety Thermometer data, Net Promoter Question results, and data from the PED database. Information on Never Events and other safety information is included by exception. The report now aligns information against Trust priorities and measures. Assessment Emerging trend on SDC with patients experiencing prolonged fasting times and perceptions that the theatre times are not communicated effectively. We will explore the data and provide a detailed analysis within the November Quality Report. General Overview Information – Quality Report October 2014 • 2 new SIRIs • 6 new complaints • 9 Closed complaints • Zero new Never Events for 18 months • 82% of Patient Experience Feedback is positive • Net promoter scores: Parent /carer - 89 Children & Young People – 87 The young person in-patient score has increased from an unusually low score of 78 in September. Recommendations • Review the enclosed report Risk Description Failure to correctly identify the greatest risks to the quality of care and safety of our patients. Key Risks Controls • Directorate Governance systems • Board Assurance Framework • Risk Register • Safety Strategy • Safety Dashboard Key Impacts Strategic Objective Strategic Priorities CQC Registration NHS Constitution Other Compliance Equality, diversity & human rights Assurances • • • • Monthly Board Safety Report Mortality Review Monitoring of incident trends Monitoring of complaints trends Every child and young person cared for by Birmingham Children’s Hospital will be provided with safe, high quality care, and a fantastic patient and family experience 3. Further develop our approaches to gaining feedback from staff, children, young people and families to ensure that their voice is heard at every level of the organisation. 4. Further innovate our systems to promote and enhance patient safety and reduce avoidable harm. Standard 16 - Assessing & monitoring the quality of service provision could be affected by a failure to manage risks highlighted by the report. Risks to compliance with other standards may be highlighted by the reports. Patient Rights • Quality of Care and Environment • Treatments, Drugs • Respect • Consent and Confidentiality • Informed Choices • Complaint and Redress The report supports compliance with NHSLA and Monitor requirements Right to life Quality Report: Safety & Patient Experience October 2014 Vin Diwakar, Chief Medical Officer Michelle McLoughlin, Chief Nurse 1 New Events & Concerns There have been no new Never Events since 15/4/13 There have been 2 new SIRIs 14/15:43 Patient attended the Emergency Department and was diagnosed with a suspected viral respiratory infection. This patient was discharged after an hour in the department, then represented several hours later with severe sepsis requiring admission to PICU. 14/15:39 An incorrectly recorded weight was used to generate the patient’s prescription. The child’s mother had given the weight in pounds and ounces and it had been recorded in kg. The patient received an overdose of gentamicin on two occasions. Patient is attending Physiotherapy but Mother claims they have "failed to provide her daughter with a satisfactory pain management programme" Father disagrees with Emergency Department Clinical Lead response and the reasons his daughter was discharged from ED. There have been 6 new Formal Complaints No. Complaints 25 20 15 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 May-13 Jun-13 Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14 Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 10 Mum is concerned that there was a lack of 5 information about waiting times in ED, that they 0 experienced considerable delay which resulted in her self-discharging her son, and there is a difference in the pathway between referrals and walking straight into ED. Concerns about the quality of care on PICU and Ward 15. Patient Experience database – Father feels that he was not listened to and all treatment options were not considered. A vascuport port extension had Family state that a Consultant was very been left in for 2 weeks and 3 days, dismissive. without being changed, where is The family state that the Consultant indicated should have been only 7 days, as per that she would do a blood test but “it was hospital policy. The child suffered stupid as the results would come back normal from a pseudomonas infection. and she would be discharged in any event.” The family were also asked if they wanted a chromosome test without explanation. Need to Improve comments Emerging trend on SDC with patients experiencing prolonged fasting times and perceptions that the theatre times are not communicated effectively. We will explore the data and provide a detailed analysis within the November Quality Report. Closed SIRIs There were 4 closed SIRIs in September Summary 14/15: Failure to identify NAI before discharge resulting in a patient being put at risk of further injury. Findings There were no clear systems failures which contributed to this incident. The decision to rule out NAI was made by a competent person and there was no information which should have been available to support this decision which was not available. 14/15:21 Excoriation injury to buttock. This is believed to be a chemical burn caused by the patient’s faeces. The patient is a very complex cardiac patient and had been suffering with gut motility problems. Records show that the patient was promptly cleaned after each episode of diarrhoea. Findings On balance the skin injury was caused by a septic embolus and that this being such an unusual circumstance was not predictable or preventable. 14/15:07 Haematology handover sheet was found outside the entrance to another hospital. 14/15:01 Burns Handover sheet containing some patient identifiable details was found on the site of another organisation. Key Actions This case will be used as an example of how subtle NAI can be. This will be built into safeguarding training and will be used as part of the ED and General Paeds Peer review process to share the learning widely across the teams. We will highlight this case to a wide audience so that they are aware of this potential risk. • While we continue to work towards an electronic handover solution we will develop the handover sheet to include a watermark and so that it is printed on a specific colour which will act as visual cues to prompt staff about the importance of keeping these documents safe. Posters have been displayed across the Trust reminding staff about the importance of document security. • Specific guidance has been added to the Information Governance Policy in relation to the practice of taking handover sheets off site. This guidance has been publicised across the entire organisation via a joint letter from the Chief Nurse and Chief Medical Officer. • Each specialty must risk assess their handover sheet practice to ensure that we are minimising the risks of confidentiality breaches. Awareness of this risk will be raised across the Trust. 3 Closed Complaints There were 9 Closed Complaints in September Summary Concerns about the lack of information provided by Endocrinology. Mother believed her son has been prescribed the incorrect emergency injection for adrenal crisis. NHS England expressed concerns about a discharge summary produced by the Emergency Department that was sent to a Health Visitor. Key Actions • • Explanation provided in relation to prescribed medicine Literature now available for families • • ED Doctor to write a letter of clarification for the GP New ED IT System has been purchased to allow free text to enable additional explanations, in addition to automated text from codes, when formulating discharge letters • • • • Concerns about length of wait for steroids and concerns that • • patient was provided with incorrect breast milk. • • Concerns that a consultant had not arranged for MRI of brain • and spine to be done under General Anaesthetic together and for Lumbar Puncture to be done whilst under General Anaesthetic - as discussed with parents previously. Concerns about a delay in diagnosis including a delay with an • • MRI scan and obtaining the results of the scan. • • • Concerns that a Consultant Nephrologist did not listen to her • and made assumptions when diagnosing. The Contractor has held discussions with all drivers to remind them of the no smoking requirements BCH and Contractor have created a Charter based on the Trust Values Contract amended to ensure that 100% of journeys arrive on time with penalties in place Amendment to contract to include Daily Communication between the contractor and the Trust Guidelines on the roles and responsibilities of teams when care is shared between teams Implementation of Safer Handover Toolkit Refresh all nursing staff on handling, storing and administration of Expressed Breast Milk (EBM) Undertake a review of Trust Policy and processes for handling, storing and administration of EBM New system implemented to ensure that if a scan request is received from different specialties, each request is reviewed in terms of specific requirements for the patient, and not just one request as had happened in this case Father received a Did Not Attend (DNA) letter although they • had attended the appointment and have not received the results of the MRI and CT scan. Explanation and apology provided to family in relation to the DNA letter being incorrectly sent and information provided in relation to the results. Concerns about the taxi service from BCH. Observations included rudeness, inefficiency and smoking on arrival. Concerns about communication between Consultants and G.P.s - appointment changed 3 times. General concern that the hospital were not taking his concerns about the patient's health seriously. • • • Extension of hours within the cross-sectional radiology team to encompass 6 day working Additional MRI sessions instigated Additional Consultant staff recruited to manage the increasing demand for imaging Additional Radiographer staff are being recruited to allow for further extension to service Mobile MRI scanners have been used to increase capacity Explanation provided in relation to diagnosis. Meeting arranged with the family and clinicians to discuss and resolve issues raised Explanation provided about the information shared with the GP following clinic appointments Apology provided for the delay in one of the clinic letters being sent to the GP 4 Complaints Quarter 2 2014/15 Key facts: •23 Formal Complaints in Q2 •82 individual issues were identified within the 23 complaints received in Q2 •In Q2, there were no referrals to the Ombudsman •111 Formal Complaints Received in 2011/12 •73 Formal Complaints Received in 2012/13 •110 Formal Complaints Received in 2013/14 Frequency of Complaints since 2005/06 to date 50 40 30 20 10 0 Complaints per 1000 admissions Complaints According to Theme Q2 3 25 Waiting, delays, cancellations and access to services 45 19 28 Staff Attitude Quality of treatment Communication Other 50Pattern since Q4 2010/11 40 Waiting, delays & cancellations Staff Attitude 30 20 Quality of Treatment 10 Communication 0 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 1011 1112 1112 1112 1112 1213 1213 1213 1213 1314 1314 1314 1314 1415 1415 Other PALS Contacts – Quarterly Analysis – Q2 Waiting, delays & cancellations Quality of Treatment Quality of Medical Care e.g. concerns about treatment received to include misdiagnosis Staff Attitude Communication Oral Communication e.g. lack of information about delays, treatment, procedure and conflicting information between medics Other Outpatient/Inpatient delays and cancellations e.g. delays and cancellations of appointments, cancellations of surgery and difficulties in obtaining surgery date Enhancing Patient Experience Prioritising person-centred care The report presents information from different sources including, including feedback cards, e mail, ward walkabouts, verbal feedback; all collated on the Patient experience Database (PED), the Friends and Family (F&F) Questionnaire, the Feedback App, Patient Opinion and more qualitative feedback from patient experience and participation projects such as patient stories and quality walkabouts. Each method brings its strengths and weaknesses and therefore utilising a toolkit approach enables the Trust to better understand the patient and family experiences and helps prioritise where to focus efforts on action planning for improvements. Ensuring responsiveness • All feedback information from the PED, Friends & Family, the app and any other source are sent on a monthly basis to ward managers, Lead Nurses and Heads of Nursing for analysis and action. • We liaise immediately and directly with the relevant managers over any detractor or need to improve comments requiring action and monitor action progress against the comments ……the top category of need to improve comments relate to 18% • Patient feedback influences the quality walkabout choice of ward. a clean, comfortable and safe environment, including food – Combined PED and Friends & Family data….. 82% …overall satisfaction with staff, providing safe, high quality care. at BCH and Parkview; (a food survey and walkabout was undertaken– see focus on food), noise at night, activities for older children and breast feeding equipment. Need to improve Positive Staff nurse Dan was fantastic – I don’t know how we would have got through this without him - Parent (SDC) There were some concerns about being short staffed raised in a number of areas. A couple of comments specifically mentioned a shortage at night and weekends. Provide a better service at HDU seemed to be understaffed whereas in most weekends E.g. have more doctors hospitals it is seen that there is always a nurse available for treatment. (Young present, that is not the case at BCH. person Ward 7) More staff on shift especially the night shift (young person Ward 10) Friends and family questionnaire Monthly adult scores (in-patient) MSep-14 Overall Trust Discharges 1132 Total number of responses in period 261 Number of promoters 236 Number of passives 20 Number of detractors 5 Neither likely or unlikely 3 Unlikely 0 Extremely Unlikely 2 Net Promoter Score Monthly young people scores (inpatient) Overall Trust Discharges 215 Total number of responses in period 69 Number of promoters 60 Number of passives 9 Number of detractors 0 I Disagree a bit 0 I Disagree alot 0 Undecided 0 89 Response Score (20% Target) 23% Net Promoter Score Sep-14 Net promoter in-patient scores: Parent /carer scores are improved but Children & Young People scores are lower again than last month. The number of passive comments remains higher than expected. We will continue to monitor this Reasons for young people passive responses More food choice 87 Response Score (20% Target) Monthly adult ED scores Sep-14 32% Monthly Young people ED scores Sep-14 Overall Trust Discharges 2937 Overall Trust Discharges 627 Total number of responses in period 502 Total number of responses in period 132 Number of promoters 430 Number of promoters 96 Number of passives 62 Number of passives 34 Number of detractors 10 Number of detractors 2 Neither likely or unlikely 6 I Disagree a bit 1 Unlikely 2 I Disagree alot 1 Extremely Unlikely 2 Undecided 0 Net Promoter Score Response Score (15% Target) 84 17% Net Promoter Score Response Score (15% Target) 71 21% More staff at night needed It would be better if there were no teachers and no needles! ED CQUIN target responses met for September, reflecting the work and focus by ED on improving their responses More TV’s In-patient CQUIN Target responses achieved for both parent/ carer &CYP Feedback App & Social Media Improving our reputation! - Update Finalist App comment ‘Too many staff from Birmingham children's hospital are walking around the city or on public transport either in uniform and/or with ID badges on it is a disgrace.’ A staff uniform monitor rota is in place. A letter has been drafted to give out to all staff where there has been non-compliance observed in relation to the uniform policy – including if the uniform is partially visible. It is the job of the ward manager to then address the breach as they will be informed . There are posters in the ward staff rooms for information about how to ensure compliance with the uniform policy. On the first day there were no staff to report and the staff who were entering or leaving were complying with policy. Social Media Facebook & Twitter comments continue to be predominantly positive – 82 positive comments in September …2 need to improve - 1 FB and 1 twitter Security issues raised…. After being here 12 months as a mum alone late at night I among other parents feel intimidated by men daily asking for money cigarettes etc as this is a hard enough time for us all and would really appreciate security been around. A response has been sent asking the parent to contact the Welcome Desk and discuss their concerns with the Operational Security Manager. Security staff are aware and will be extra vigilant about the issue. 10 Focus on Food Patient Experience and Participation Food Survey Report - October 2014 Wards: 5, 7, 9, 10, 12, Participants: 24 (16 Parents/Carers, 8 Patients) The survey was conducted on two separate occasions by a BCH patient experience volunteer. Each time, the survey was conducted at 12:30pm, just after lunch. Each participant was asked the following 11 questions: Patient response – 8 participants The response on the surveys was overall a positive one, particularly around food choice, temperature of food and the friendliness and helpfulness of staff: •All 8 respondents said that they had been given a choice of food, that the food was at the right temperature and that the serving staff were friendly and helpful. •7 participants said that they were happy with the choice of food and 7 participants also said that they knew when the meal times were. Areas for improvement: •The availability of snacks as only 4 patients said that snacks were available if they were hungry between meal times. •The majority of patients also said that they had not been given choice over food if they were in need of it due to religious or dietary reasons; 5 said they hadn’t been given a choice compared to 3 who felt they had. In addition, the majority of patients (6 participants) had ordered their food using the MAPLE and said that they would prefer to eat their meals in their bed rather than in a group on the ward. The feedback on the appearance of the food was mixed: •4 patients said their food looked ‘nice’, ‘good’ or ‘very good’ •2 patients said their food looked ‘alright’ or ‘OK’ •1 patient said their food looked ‘bad’ •1 patient said their food looked ‘sloppy’ The feedback on the taste of the food was overall positive: •2 patients said their food tasted ‘really nice’ or ‘excellent’ •2 patients said their food tasted ‘good’ or ‘nice’ •2 patients said their food was ‘edible’ or ‘OK’ Parent/Carer response – 16 participants •15 participants said that they were given a choice of food and that they were happy with that choice. •14 participants said they felt they had been given a choice over food if they were in need of it due to religious or dietary reasons. Only 1 parent/carer said they felt they hadn’t been given that choice. •13 participants said they were happy with the food temperature compared to 1 participant who said they were not. •13 participants said that they felt serving staff were friendly and helpful, compared to 1 participant who said they were not. Areas for improvement: •The availability of snacks as 4 parents/carers said that their child had not been offered snacks in between meals if they were hungry. However, 11 parents/carers said they had. •5 parents/carers said that they were not aware of the times that the meals were due, compared to 11 parents/carers who said they were. Similarly to the patients, the parents/carers also thought that having meals served at the patient’s bed rather than on the ward was better, as only 2 participants said they should be eaten in a group on the ward. One comment was that eating on the ward was ‘not practical’. As well as this, 11 parents/carers had used the MAPLE system to order food, whereas 4 hadn’t. The feedback on the appearance of the food was overall positive: •6 participants said that the food looked ‘good’ •4 participants said that the food looked ‘as expected’, ‘OK’ or ‘fine’ •3 participants said that the food looked ‘nice’, ‘tasty’ or ‘yummy’ •1 participant said that the food looked ‘very good’ The feedback on the taste of the food was also positive: •9 participants said that food tasted ‘good’, ‘nice’ or ‘tasty’ •4 participants said that the food tasted ‘OK’ Overall, the one area to improve on that was highlighted by both patients and parents/carers was the availability of snacks in between meal times. An additional comment that was mentioned was that one participant felt that long term patients needed a greater variety of food. Ward 7 – Quality Walkabout Review noise at night. All staff reminded and plans to raise as part of induction of new staff. Explore solutions to a lack of ventilation in sluice. Review role of Mental Health Liaison Nurse. Pending Estates have been asked to review. Ensure nurse staffing board is kept up to date. Staff reminder • Working with pharmacy to continuously monitor temperatures • Recorded on the risk register Explore the solution to temperature issues in the treatment room. Improve completion of F&F Questionnaires. Questionnaire now attached to discharge paperwork. Monitoring Infection control September 2014 Infection No. MRSA Bloodstream Infections (BSI) 0 MSSA BSI (pre 48 hour) 3 MSSA BSI (post 48 hour) 2 E. Coli bacteraemia (pre 48 hour) 1 E. Coli bacteraemia (post 48 hour) 2 Glycopeptide-resistant enterococci 0 C. Difficile 0 MSSA pre 48 Hours 2011/12 MSSA pre 48 Hours 2013/14 MSSA pre 48 Hours 2012/13 MSSA pre 48 Hours 2014/15 5 4 3 2 1 0 MSSA post 48 hours 2011/12 MSSA post 48 hours 2013/14 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 April May June E-Coli - pre 48 hours 2011/12 E-Coli - pre 48 hours 2013/14 5 4 3 2 1 0 E-Coli - pre 48 hours 2012/13 E-Coli - pre 48 hours 2014/15 July Aug Sept MSSA post 48 hours 2012/13 MSSA post 48 hours 2014/15 Oct Nov Dec Jan Feb March E-Coli - post 48 hours 2011/12 E-Coli - post 48 hours 2012/13 E-Coli - post 48 hours 2013/14 E-Coli - post 48 hours 2014/15 5 4 3 2 1 0 14 Respiratory Arrests, ALTEs and Unplanned Admissions to PICU Explanation of Data Unplanned admissions to PICU are a measure of how well we are monitoring patients on the wards. Good monitoring on the wards means that we will pick up deteriorating patients more quickly, allowing us to admit them to PICU when required. A combination of high levels of unplanned admissions and low levels of cardiac arrests, respiratory arrests and acute life threatening events (ALTEs) means that we are monitoring and escalating clinical deterioration in a timely manner. Details of Cardiac Arrests In September there was 1 cardiac arrests outside PICU in theatres. It was not predictable or preventable. There were 6 cardiac arrest on PICU one of which was potentially predictable and preventable which is being reviewed through the M&M process. None of the others were predictable and preventable. Number of Emergency Events No of Cardiac Arrests (ex PIC) No of Respiratory Arrests No of Cardiac Arrests (PICU) No of ALTEs 19 18 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14 Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 15 Safeguarding Key Figures Child Protection Training ( includes Adults) Level 1 98.4 Level 2 81.2 Level 3 81.6 There has been 0 Safeguarding SIRI There has been 0 new Safeguarding Complaint There has been 0 “Position of Trust’ case There have been no new recommendations from Serious Case Reviews 100% of BSCB Meetings attended by BCH Executive lead or representative 90% of cases which require peer review /clinical supervision have had this There has been 0 child deaths related to suspected physical abuse/neglect There has been 0 reported cases for Female Genital Mutilation. • Safeguarding CQUIN: •We have completed 9 Qualitative Audit Proformas for Quarter 2 as agreed. Care Quality Commission: Inspection for services for looked after children and safeguarding in Birmingham Monday 29th September 2014: The Emergency Department and CAMHS Tier 3 and 4 were part of the inspection. We are awaiting formal feedback via the Clinical Commissioning Group. A child’s Journey through the Safeguarding Process: •A 12 yr. old was admitted to the Burns Unit with injuries consistent with an aerosol burn. However, concerns were raised due to late presentation and inconsistencies. •Detailed history taken by the Burns Consultant from the YP on his own. •This was discussed with the Consultant General Paediatrician and the Trust Safeguarding Team. •Liaison took place between the GP and School. •A referral was made to Social Care and a Strategy Meeting took place. This was attended by BCH professionals . •A Child and Young Persons Assessment was opened which would be completed by the Social Worker. •YP was seen by the Consultant Paediatrician who listened to his views. These were recorded in the referral. He wished to be discharged home and agreed a CAMHS follow up on discharge. His Social Care assessment ensured that his needs were being met holistically and his safety assured •This case was discussed in the Monthly Burns Peer Review: Reflective Practice: It is important to speak to child / YP on their own and they should be given this opportunity. All staff were aware of the safeguarding procedures and were satisfied with the outcome for the child. Mortality Past Harm Mortality data is presented in a number of ways, and an overall picture can only be gained by using a number of indicators. These are: •Absolute number of deaths per time period. •Number of deaths per time period per 1000 admissions. •Standardised mortality ratio (See next slide) •Cumulative sum (CUSUM) charts. •Review of individual deaths. Inpatient deaths per 1000 admissions This is a simple calculation to overcome any variations in admission numbers over time (e.g. the hospital may have more admissions in the winter months) or between hospitals of different sizes. Data can be compared between organisations by this method as it allows for different admission numbers but it is limited as a tool for comparison as there is no modification for case mix. The graph on the right shows the number of inpatient deaths per 1000 inpatient admissions at BCH since June 2012. Please note that the data does not include deaths which occurred in the Emergency Department. Absolute Number of Deaths The simplest way to represent mortality is as an absolute number of deaths in a particular time period; however it does not take into consideration either the number of admissions to the hospital or the case mix of patients. It is useful only as a sense guide to other data as it has not been modified in any way. Data cannot be compared between organisations in this format. 16 Deaths Deaths per 1000 Admissions 14 12 10 8 6 4 2 0 17 Standardised Mortality Ratio (SMR) In order to account for differences in case mix for different organisations the idea of standardised mortality ratios has been developed. This attempts to account for differences in patients, such as diagnosis, age and pre-existing medical problems, and allows for comparisons between hospitals. A standardised mortality ratio (SMR) is the ratio of the actual number of deaths in a hospital within a given time period, to the number that might be expected if the hospital had the same death rates as a larger reference population (e.g. all English Hospitals). The SMR scores can be presented in a number of ways. Run Chart This shows how the standardised mortality rate of a hospital changes over time. If there are a small number of deaths in each time period then the month to month variation can be quite wide (as is the case with BCH where there are on average 4-12 deaths a month). 18 Bar chart presenting data comparing a number of hospitals: This shows the position of an individual hospital in comparison with its peer group. It is easy to understand but does not give much information about whether our outcomes are unusual. The graph presented below shows 6 months’ worth of data rather than 12 as previously presented. Our SMR has risen slightly from 161.67 to 159.92 Movement in last month Funnel plot This shows the standardised mortality ratio on the Y axis, and the number of expected deaths on the X axis. Control limits can be applied, so that it is possible to see how likely that the variation from a score of 100 is by chance only. In the example below an amber dot occurs if there is between a 0.3% (1 in 330) and 5% (1 in 20) likelihood that the score is different from 100 by chance and a red dot if there is less than a 0.3% likelihood that the score is different from 100 by chance. Such warnings should be investigated as to cause. The funnel plot below is presented using 6 months’ worth of data. We are in the red section of the funnel plot. 19 Deaths in the Paediatric Intensive Care Unit (PICU) CUSUM Charts Another way of representing outcome data is by cumulative sum charts. These can be used where there is a score available to give a risk of mortality for each individual patient. Currently this method is in use at BCH for intensive care. The charts use data from all patients, not just deaths, so are more powerful than SMR in detecting problems. For BCH, the PICU CUSUM is a good reflection of overall hospital mortality as over 70% of deaths at the hospital occur on PICU. There is no evidence of systemic care failures which could have contributed to deaths on PICU. 20 Deaths in Cardiac Services CUSUM Chart One of the Trust’s highest risk specialties is Cardiac Services. The nature of the activity means that proportionally more of our mortality is related to that specialty than others. The team carefully monitors clinical outcomes to ensure that that we are providing high quality care. The CUSUM chart is a graphical representation of the outcome data for the specific procedures which are nationally monitored (70-80% of our patients fall into this group). In addition, the team also monitors overall mortality for all surgical patients. An upward movement in the chart means that the outcome for a specific patient was better than expected. A large increase means that the outcome was significantly better A downward movement means that the outcome for a specific patient was worse than expected, again the size of the decrease is a measure of how much worse the outcome was than expected This series of 3 downward movements represents 3 specific patients experiencing a worse than expected outcome in a relatively short period. This series of outcomes will be reviewed as part of the Cardiac M&M meeting and future data monitored closely. Overall our outcomes are better than expected. However, please note that the baseline will be reset on a regular basis, so we do not expect to move further and further from the x-axis 21 Deaths in Liver Transplant CUSUM Chart 7 month lag time Another of the Trust’s higher risk activities is Liver transplantation. Although we do not carry out a large number of these, the team monitors the outcome rates posttransplant. The graphs below show that our outcome rates are comfortably within acceptable limits. Interpretation of the charts The O-E chart is a useful tool for observing performance over time. A downward trend indicates a lower than expected rate of mortality compared with the baseline period, whereas an upward trend points to an observed mortality rate that is higher than expected. To identify statistically significant changes the tabular CUSUM chart is used to complement the O-E chart. A significant shift in the underlying mortality rate is evident when the chart crosses the limit and generates a signal. The tabular CUSUM chart can be used to forewarn of possible future signals as the chart approaches the limit. Such ‘signals’ may be due to one of a number of different reasons. A signal may be due to transplantation of patients of higher risk than previously, a short run of adverse events, or it may occur just by chance with no underlying cause (i.e. a false positive result). 22 Item 14.219 Board of Directors Thursday 30th October 2014 Enc 03 Strategic Objective/ Enabler Every child and young person requiring access to care at BCH will be admitted in a timely way, with no unnecessary waiting along their pathway Report Title Performance – Sep 2014 Performance Report Sponsoring Director Deputy Chief Executive Author(s) Head of Health Informatics, Performance Manager Previously considered by Finance and Resources Committee Situation This report provides the September update on the Trust Performance supporting improving our patient experience. The report highlights performance and in particular where performance is not being met and any concerns and improvements planned. The attachment provides further details on our current and comparative performance Background Performance to August 2014 As previously reported there have been four areas of particular concern regarding operational performance in 2014/15 to date • Diagnostic waits including MRI, where we have been breaching the target of 99% of patients to be seen in 6 weeks, although the actions taken had been starting to improve the position, with total breaches reducing over the year. • 18 weeks waiting times have been met, but by a narrow and diminishing margin, in part due to increasing demand including from outside the Birmingham area. We have reported that meeting this target in future would remain a challenge. • The hospital’s available physical capacity has been impacted upon by increasing length of stay and delayed discharges, in turn leading to fewer available beds and cancelled operations. • Total Trust cancelled operations and those nationally reportable are high. We have been struggling to successfully re-schedule all children and young people within 28 days and have had breaches of the 28 day standard We noted last month that the position in August had markedly improved, due to a combination of factors including reduced demand for services through the holiday season and management and clinical initiatives to address issues. Assessment Summary of Performance in September 2014 Performance in most areas remains steady this month, although we haven’t performed against all of our targets as well as in August in part because the level of demand for our care increased following the end of the school holidays. The key highlights include; • • • • • • • nationally reportable cancelled operations continued to decrease with 26 reported this month (28 last month), and are now well below the recent BCH average; there are no 28 day breaches regarding the rescheduling of cancelled operations for the second month running; all the key ED performance targets have been met; the number of long stay ‘bed blocking’ patients have remained the same as last month. For CAMHS there has been no movement in these patients since last month. Bed availability issues have reduced and are no longer causing significant numbers of cancelled operations; only four tertiary and urgent patients were not found a bed; only 2 KIDS patients could not be supported in our PICU; and CAMHS continue to meet 18 weeks targets, although performance has fallen again to 93.9%, and 11 patients could not be found a bed. Regarding the target to see diagnostic tests in 6 weeks, performance has improved in September with 22 breaches compared to 29 last month. We are projecting to carry 27 general anaesthetic (GA) breaches in October. This is higher than projected in the August paper (15), the rise stems largely from a technical issue with the method for extracting data from the Radiology Information System (RIS.) As a result the likely no.of breaches was under-estimated. This has now been resolved. Plans are being put in place regarding additional anaesthetic capacity, which if successful and with normal levels of demand experienced the target should be met in November 2014. RTT and 18 weeks continues to remain a concern, although we have again met our national targets for the month by a small margin. (a) Access to Services Diagnostic waits including MRI There were 22 patients (17 MRI and 5 CT) at the end of September who had been waiting over 6 weeks for a diagnostic test. This amounts to 96.1% of all patients seen versus a target of 99%. The breaches were all for general anaesthetic (GA) cases. Non GA cases are being managed going forward with the help of additional capacity at Aston Brain Centre using their 3T scanner and radiographers. Standard of image is good and the staff are former BCH employees. Aston sessions are booked for 22nd and 29th October and there will be 1 or 2 days a week available every week from November onwards. Given reasonable levels of demand this should allow for the non GA list to be managed within target. Managing the GA cases within 6 weeks is our current difficulty. Scanner capacity is not the issue, rather it is anaesthetic staffing that is in short supply. However an additional staff member starts in November, and as we start to meet the non GA demand more successfully thanks to Aston, we should be able to switch some capacity at BCH from non GA to GA cases. In this manner it is planned to create an additional 11 GA sessions, which is circa 44 operating slots, in November. All other things being equal, this ought to be enough capacity to bring our performance in line with the target. However currently we are projecting 35 breaches for November, and 32 for December, without this additional capacity factored in. Of further interest is that demand (slide 8 of the Powerpoint attachment) has again shown weeks where it is high and above the average. This will need to be monitored carefully in terms of its impact on demand. Also clinical changes can have an impact, for example regarding CT demand. The new CT scanner has allowed for better clinical practice eg the ability for us to carry out advanced coronary scans, replacing the need for catheters. These changes, though welcome, will create more demand on the Radiology service. 18 weeks waiting time The 18-week standards were met in September with the non-admitted performance being only just above the target at 95.02%. Performance for admitted patients was 90.3% and for incomplete pathways 92.5%. There has been significant emphasis placed in September 14 on reducing our backlog of long waiters in the Trust. This has had an impact on our performance around the targets for completed clocks, and the slide on page 5 of the Performance Report shows this. The ‘Patients Not Treated Within 18 Weeks’ chart shows many more non admitted clock stops over 18 weeks than usual. As a result we only just met our target. However this will help us with future positions once the backlog is cleared, and also fits in with the requirements of our commissioners. The chart on slide 6 of the Performance Report shows an increase in the numbers of patients who have yet to receive a TCI date after 14 weeks on the list, or whose TCI will take them over 18 weeks. This remains at historically high levels and is a key indicator of the difficulty we will have to manage within 18 weeks over the next month. Slide 7 shows that there are 73 patients either waiting over 30 weeks at the end of September, or whose clock stopped after 30 weeks in month. Again the reduction since the peak of May 2014 is indicative of our focus on reducing the number of long waiting children and young people. The total inpatient waiting list continues to be high with 4114 patients on the list at the end of September (4168 at the end of last month). However we have seen a good reduction in the size of the outpatient waiting list again partly as a result of our emphasis on bringing in long waiters. This has fallen by 500 since its peak in July 14. Nationally there is increased scrutiny on RTT and weekly reporting is now required to Monitor and Commissioners on our backlog of RTT patients who are awaiting a clock stop. It has been announced that ‘resilience’ funding will be made available to support organisations to meet the targets and Commissioners have agreed monies to fund any contract over-performance that occurs as a result of BCH clearing the current 18 week backlog and continuing to meet the performance standards. Based on our modeling work we project that we will continue to meet the standards for 18 week clock stops in the months of October and November, although addressing the ‘over 18 week and still waiting’ backlog means it will be tight. The backlog overall will come down to around 480 by the end of November, approximately 94% of the list will then be within 18 weeks. We anticipate that Orthopaedics would have the most over 18 week waiters at that point, followed by Plastics and ENT. As noted last month the short term workload is about ensuring detailed planning and scheduling are in place to make sure all existing capacity is used to its full potential wherever possible. The surgical flow project with Newton’s will make a contribution to this. However step changes in capacity are currently some time off, either via a mobile theatre (not until Spring 2015 if implemented) and then eventually the building work associated with Next Generation. Therefore looking forward, based on current assumptions and forecasts meeting the 18 week standards will continue to be a challenge. Access to services – other areas Access to BCH has remained good during September for the other pathways into our hospital. Emergency Department 96.4% of patients were seen within 4 hours and there were 148 breaches. This is well above the target of 95%, but it is the highest number of breaches for a month in 2014/15 so far, even though overall activity for September was not particularly high. Tertiary referrals and Home Referrals Performance in this area remains good. • Of the 163 referrals, only 2 were not found a bed in September. • Only 16 patients waited over 24 hours for a bed (one more than last month) and is the second lowest figure since February 2013. • When comparing actual time of admission against recommended time for admission, 90.5% of requests were met in target time compared to 91.9% last month. PICU (Paediatric Intensive Care Unit) referrals The West Midlands PICU service is provided by BCH, University Hospitals of North Staffordshire NHS (UHNS) Trust and the KIDS (Kids Intensive Care Decision Support) service run by BCH. Performance remains steady as only one West Midlands (WM) patient (compared to one last month) and three non WM patient (compared to one last month) could not be supported due to hospital reasons. This is much lower than the historical average. CAMHS referrals The CAMHS Tier-4 (Child & Adolescent Mental Health Service) West Midlands service is provided by BCH and other providers (some private) with BCH providing the assessment of all requests, ideally within 4 weeks. The time taken to undertake assessment now stands at 7.9 weeks (compared to 5.9 weeks last month and 4.3 weeks in 2013/14). Assessment of CAMHS patients within four weeks has reduced to 46% from 54% last month, so that performance is worse than for 2013/14 at 52%. This was a result of a shortfall in capacity. A capacity planning exercise has been undertaken to ensure all job plan slots are being delivered and CAMHS are about to trial telephone calls to patients failing to respond to their first invitation letter to reduce the wait time to first appointment. Due to capacity and urgency, eleven tier 4 patients could not be supported by BCH CAMHS in September; (compared to six in August). There continues to be significant capacity pressures across the West Midlands and nationally for Tier 4 beds. (b) Utilisation of Facilities Cancelled operations In September, 26 patients or 1.13% of all operations were nationally reportable e.g. cancelled on the day of operation or after admission by the hospital for a non-medical reason. This is less than previous month (at 28) and September 2013 (at 54). More than half these (14) were as a result of theatre capacity being lost to Trauma or other emergency cases (including 5 due to liver transplants. Bed shortages accounted for only 6 cancellations and are therefore not a significant concern this month. 22 of the 26 (85%) of cancellations affected the Surgical directorate. There were no breaches of the 28 day standard for the second month due to active management of breaches. Bed shortages were not an issue that led to cancellations in September, and this is indicative of there being slightly more scope to schedule patients and this helps with achievement of this standard. Regarding the Trauma cases, in mid month 2 elective lists were switched to Trauma, which should have a positive effect on both cancellations and patient experience. A Trauma coordinator is now in place to assist in identifying lists and beds for these patients. Similarly we have created a surgical flow co-ordinator post for 6 months to help ensure we utilise as much capacity as possible in a time of growing demand for our services. Bed Availability - Long stayers and delayed discharges The overall numbers of long stay patients remained steady in September 2014. The six CAMHS patients from last month were still awaiting placements and were delayed for 975 days in total. In September, there were four children who were fit for discharge but waiting for non-hospital related actions before they could be discharged (two for a care package, one for social care and one to be discharged to DGH). The total number of bed days relating to these delays is 333 days compared to 418 last month. Recommendations The challenges going forward remain the same as last month and are; - to continue to put in place the arrangements needed to meet the diagnostic wait target. Latest plans suggest this will be met in November 2014 unless there are unanticipated issues with demand and or capacity. - explore all avenues to maintain elective throughput and continue to meet our 18 weeks RTT performance; - continue to maintain the other levels of access to services and utilisation of facilities seen in September when demand for services continues to pick up further into the Autumn, aided by the winter plan and associated funding. Regarding this to note the slight dips in performance for the ED standards and for CAMHS access in September and review again in the October report. The Board is asked to note the performance and plans for further improvement. Key Risks Risk Description Controls Assurances Escalating demand for our Discussions with Maintaining scrutiny on services, potential risk of commissioners to be held performance against various failing access targets about demand management RTT targets Bids against operational resilience moneys Insufficient capacity in place Appropriate escalation to meet service demands systems in place Validation of waiting lists stepped up Daily, weekly and monthly reporting in place. MRI capacity being identified Revised capacity plans being including mobile van and produced. Aston for non GA and more GA capacity on site Specialty recovery plans and plans for additional capacity being put in place as part of response to ‘Operational Resilience’ Capacity plans being renewed and developed. This includes modelling capacity/demand between now and 2020 (new hospital) Key Impacts Strategic Objectives CQC Registration outcome) NHS Constitution Other Compliance This reports covers progress against meeting the strategic objectives linked to supporting improving our patient experience. (state 4: Care and welfare Yes – treatment within 18-weeks is a requirement within the NHS Constitution. (e.g. Many of the indicators are local or national standards NHSLA, Information monitored by the Department of Health, Monitor and our Commissioners. Governance, Monitor) Equality, diversity & human The report considers any particular impact on patients with learning disabilities, and on different ethnic groups. rights Trust contracts Non-delivery of NHS standards can result in financial penalties Other Meeting the strategic objectives raises the profile of Trust locally, regionally and nationally Operational Performance Report Month 6 2014/15 Performance for September 2014 David Melbourne Paul Franklin Pragati Raithatha Deputy Chief Executive Officer and Chief Finance Officer Head of Health Informatics Performance Manager 1 Operational Performance Indicators How our patients access care ED - time in ED 18 weeks performance (incomplete) PICU – non WM patients supported (6 patients) ED – time to seen 18 weeks performance (admitted) PICU – non WM patients not supported ( 3 patients) ED – Time to triage (all) 18 weeks performance (non admitted) PICU – WM patients not supported (only 1 patient) ED – time to triage (ambulance) Long waiters - patients not treated within 18 weeks due to insufficient capacity Diagnostic waits over 6 weeks ED – Left without being seen Long waiters - patients not treated within 30 weeks In region Tertiary referrals sent elsewhere (2) ED – Unplanned readmissions Long Waiters - patients waiting over 52 weeks Tertiary patients waiting over 24 hours for a BCH bed (16) Patient Deflectors 18 weeks performance - CAMHS CAMHS Patients that requested a T4 bed and were not admitted (11 patients) Utilisation of our facilities Cancelled operations – national definitions Cancelled operations – breaches of 28 day standard Cancelled operations – all hospital cancellations Cancelled operations - equipment failures or admin errors Cancelled operations - patients cancelled more than twice Long stay patients and patients with delays after being declared fit for discharge 2 Operational Performance Report Month 6 2014/15 Performance for September 2014 How our patients access care 3 Emergency Department 95th % time in A&E: 3.97hrs 95th % time to triage (all): 33 minutes Median time to be seen: 60 minutes 95th % time to triage (ambulance): 13 minutes 0 Patients Deflected Left without being seen: 2.31% ED re-attenders for related condition 2.51% ED overall position: The seasonal aspect of ED demand meant that as expected the August activity was low and is back to higher levels in September. Consequently performance against most targets has deteriorated since last month, although all have been met except the triage target for all patients (not just ambulance.) It is pleasing to note that ED re-attenders decreased from 3.39% last month to 2.51%. Overall therefore performance against our ED standards remains good. % Patients Who Left ED Without Being Seen Standard < 5% Total Time Spent in A&E Standard ≤ 4 hours (95th Percentile) Time to be Seen Standard ≤60 minutes (Median) 4.70 90 7.0 80 4.50 6.0 70 5.0 4.30 4.0 4.10 60 50 40 3.0 3.90 30 2.0 20 3.70 1.0 10 3.50 0.0 A M J J A S 2012-13 2014-15 O N D 2013-14 Target J F M A M J J A S O N D 2012-13 2013-14 2014-15 Target J F M 0 A M J J A S O N D J F M 2012-13 2013-14 2014-15 Target 4 18 week waits Admitted Non admitted Incomplete • 90.3% • 95.02% • 92.5% 18 weeks overall position: all targets were met in September 2014 by a very slight margin for non admitted in particular, where percentage achieved is less than last month. 73 patients were waiting over 30 weeks (compared to 92 last month) and also the number of patients receiving TCIs late in their pathway remain relatively high, so the pressure on waiting times is likely to continue going forward. Addressing our backlog of long waiters resulted in a large increase in non admitted clock stops over 18 weeks in September 14. 206 patients were not treated within 18 weeks due to insufficient capacity. The non admitted clock stops have increased to 90. 18 weeks admitted performance 94.0% 93.0% Patients not treated within 18 weeks due to insufficient capacity 92.0% 91.0% 90.0% 89.0% 90 88.0% There are no patients waiting over 52 weeks. This stems in part from agreed new admin and reporting procedures around where patients request very long pauses on their pathway. Previously we have been reporting these as 52 week waiters Feb-13 41 2 54 0 8 2 105 83 61 56 62 73 128 118 1 118 75 Admitted 97 112 Non admitted 8 90 87 90 97 112 116 Sep-14 3 3 4 Aug-14 2013/14 4 Jul-14 7 46 Jun-14 M Mar-14 F Jan-14 J Dec-13 D 12 8 Oct-13 N Sep-13 O Aug-13 2012/13 S Jul-13 A Jun-13 J May-13 J Apr-13 M Mar-13 A 10 May-14 11 Nov-13 86.0% 60 14 Apr-14 14 Feb-14 87.0% 5 18 week waits % still waiting for clock stop (incomplete) under 18 weeks Fig 2: 18 weeks Current problem, future problem 100.0% 700 98.0% 600 500 96.0% 400 94.0% 300 92.0% 04.10.14 Target 31.08.14 M 03.08.14 F 13.07.14 2014/15 J 22.06.14 D 25.05.14 N 27.04.14 O 06.04.14 2013/14 S 16.03.14 A 23.02.14 J 02.02.14 2012/13 J 12.01.14 M 15.12.13 A 24.11.13 0 03.11.13 88.0% 13.10.13 100 22.09.13 90.0% 01.09.13 200 Performance for patients still waiting for their initial treatment (either admitted or non admitted pathway) has increased slightly this month to 92.5% being within 18 weeks (Fig 1.), compared to 92.1 last month. This remains very close to the target of 92%. Regarding patients waiting for an admission (Fig. 2), the green line, (which is the total of the red and blue lines) illustrates the overall potential problems we have in managing our 18 weeks admitted demand; this has increased steadily since April 2014, with slight decline in July and August. The blue line illustrates patients with a date to come in who are already over 18 weeks or whose TCI date is over 18 weeks. This has reduced slightly. The red line illustrates patients who are waiting 14 plus weeks and do not have a TCI date yet. This is starting to increase again. The challenge of meeting 18 weeks for our patients continues to be significant and all Directorates are reviewing this to see if actions can be taken to help reduce these waits. 6 Whole Inpatient waiting list and long waits 73 RTT patients either still waiting or whose clock stopped after 30 weeks Whole Waiting List Size (not just RTT patients) 8000 All Patients Still Waiting or Whose Clock Stopped Over 30 Weeks 160 7000 Specialty break down of the 59 patients still waiting over 30 weeks 140 6000 120 5000 100 80 140 140 60 40 20 Inpatients Surg/Cardiac Inpatient Outpatients The overall waiting list for surgical and cardiac stands at 2303, with the total inpatient list standing at 4114 and outpatients at 6695. Although there has been a decrease in the lists this month, they remain extremely high when compared with previous periods. The reduction in the size if the inpatient list is marginal, but actions to address outpatient demand and long waiter backlog is now having a good impact on the size of the outpatient list. 73 94 109 116 99 107 104 92 73 Sep-14 Aug-14 Jul-14 Jun-14 May-14 Mar-14 Feb-14 Dec-13 0 Nov-13 24/09/2014 24/08/2014 24/07/2014 24/06/2014 24/05/2014 24/04/2014 24/03/2014 24/02/2014 24/01/2014 24/12/2013 24/11/2013 24/10/2013 24/09/2013 24/08/2013 24/07/2013 24/06/2013 0 57 61 Oct-13 1000 Sep-13 2000 Jan-14 3000 Apr-14 4000 At end of September, there are still 73 patients waiting over 30 weeks (either still waiting or who had their clock stopped in the month), compared to 92 last month. Paediatric Cardiology Paediatric Ear Nose and Throat Paediatric Neurosurgery Paediatric respiratory Paediatric Plastic Surgery Paediatric Surgery Paediatric Trauma and Orthopaedics Paediatric Urology Paediatrics Grand Total 3 6 2 1 15 5 16 8 3 59 The action to address our long waiters is having a positive impact here. Of the 73 patients 14 had their clock stopped over 30 weeks and 59 are still waiting. 7 Diagnostic waiting lists Diagnostic waits overall position: We continue to fail to meet our key target for MRI, although breaches have reduced significantly from the start of this year. There were 17 breaches in September for MRI and also 5 CT breaches. All are GA related. Demand continues to be high and capacity subject to some constraints and therefore some breaches will continue into the future. The chart below indicates that a reduction in demand and the additional capacity created to address our six week wait problem has had an impact on the size of the overall MRI waiting list over the last few months. MRI Waiting list Total WL 1400 GA WL 1200 Patients waiting >6 wks for diagnostic test - actual & forecast 1000 Patients 160 140 120 100 80 60 40 20 0 800 600 400 200 2012-03-… 2012-04-… 2012-05-… 2012-07-… 2012-08-… 2012-09-… 2012-10-… 2012-11-… 2012-12-… 2013-01-… 2013-03-… 2013-04-… 2013-05-… 2013-06-… 2013-07-… 2013-08-… 2013-09-… 2013-11-… 2013-12-… 2014-01-… 2014-02-… 2014-03-… 28/04/20… 29/05/20… 2014-06-… 2014-08-… 2014-09-… Dec-14 Total waiting list additions by week Total external referrals UpperCI Mean TGT (10) 180 160 140 120 100 80 60 40 20 0 Total Additions by week Lower CI Linear (Total Additions by week) 07/09/2014 07/08/2014 07/07/2014 07/06/2014 07/05/2014 07/04/2014 07/03/2014 07/02/2014 07/01/2014 07/12/2013 07/11/2013 07/10/2013 07/09/2013 07/08/2013 07/07/2013 07/06/2013 07/05/2013 07/04/2013 07/03/2013 07/01/2013 The service continues to be under significant pressure, but actions to manage the position are starting to show results, as breaches are significantly lower than at the start of the year. 22 patients breached the 6 week target in September 2014 (17 are MRI breaches and 5 were CT breaches). Breaches are predicted to continue due to the high demand. Predicted breaches for the next three months are shown in the graph above and are predicted to be 27, 35 and 32 breaches. These breaches are all for GA cases and this is the area where we have the most capacity constraints currently as the additional Aston capacity for the non GA cases is starting to come on line. Prediction for Oct to Dec is slightly higher than reported in the August paper as the figs there were under-reported due to a technical issue with the method for extracting data from the RIS System. However work is in hand to allocate additional GA sessions in November due to new anaesthetic capacity coming on line. This would mean that with normal demand and without unexpected capacity issues we should meet this target by then end of November 2014. The SPC chart (right) on total waiting list additions shows that the high level of additions fell in August (average of 120 per week). However this trend has reversed in September with an average of 130 additions per week. 07/02/2013 Nov-14 Oct-14 Sep-14 Aug-14 Jul-14 Jun-14 May-14 Apr-14 CT 27 35 32 Patient numbers MRI Mar-14 Feb-14 Jan-14 Dec-13 Nov-13 Oct-13 0 8 Access to CAMHS Community CAMHS - Waiting Time to Assessment A:- 0-4 wks CAMHS 18 Weeks Performance 100% 100 80% 362 709 95 60% 956 105 90 40% 85 20% 80 1475 B:- 4-8 wks C:- 8-13 wks 43 367 354 233 1066 757 854 881 767 1125 884 2011/2012 2012/2013 D:- >13 wks 8 288 199 1211 430 2013/2014 2014/2015 0% 75 2010/2011 Apr May Jun Jul 2012/13 Aug Sep Oct 2013/14 Nov Dec Jan 2014/15 Feb Mar Target CAMHS continue to achieve their 18 week target with 93.9% of patients seen within target in September (and 97.8% year to date). However the last 2 months have seen a decline in performance. Financial Years In September CAMHS assessment of their patients within four weeks has reduced to 46% from 54% last month, so that performance is worse than for 2013/14 at 52%. The average wait is now 7.9 weeks from 4.3 weeks in 2013/14, and 8 in 2012/13. This is as a result in shortfall in capacity and this is currently being reviewed to ensure all job slots are being delivered. Also to reduce wait times to first appointment the department is trialling telephone calls to patients not responding to their invitation letter. CAMHS Patients that requested a T4 bed and were not admitted (month trend) 18 16 14 12 10 8 6 4 2 0 Apr May Jun Jul 2012/13 Aug Sep Oct 2013/14 Nov Dec Jan 2014/15 Feb Mar Tier 4 referrals (in blue) and gateway assessments (the red line) have increased in September. The green line shows patients not able to access a bed and therefore referred to the Specialised Commissioning Team. The number has increased to 11 in 9 September. Urgent Tertiary and Home Referrals 163 referrals for specialist beds, 148 admitted 2 in region patients unable to get a bed 0 out of region patients unable to get a bed 13 patients no longer required a BCH bed 14 in region patients waited over 24 hours to get a BCH bed 2 out of region waited over 24 hours to get a BCH bed Overall position: Tertiary and home urgent referrals totalled 163 in September. Two patients were refused a bed (both in region) and 16 patients waited over 24 hours which continues to be lower than average. Overall 90.5% of requests were met within the required clinical timescale. Activity levels - The level of urgent referrals (163) continues to be relatively low in September. Urgent Tertiary and Home Referrals 250 200 150 225 175 170 188 191 172 182 197 177 188 181 173 163 169 209 230 217 179 159 163 100 50 0 Feb-13 Mar-13 Apr-13 May-13 Jun-13 Waiting time vs. clinical target time Clinicians can request the patient to be admitted in up to 48 hours, dependent on their assessment. The graph shows the timescales requested for admittance and time of decision to admit. Overall 90.5% of requests were met in September (compared to 91.9% in August). Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14 Apr-14 May-14 Jun-14 Home Tertiary Total Jul-14 Aug-14 Sep-14 Performance vs clinical target time for patients provided a bed - home and tertiary referrals 70 100% 97% 89% 60 78% 50 80% 40 60% 30 40% 20 20% 10 0% 0 within 12 hours Met 12-24 hours Up to 48 hours Target Time Not met % patients meeting tgt time 10 Urgent Tertiary and Home Referrals Referrals Sent Elsewhere Two referrals were sent elsewhere in September 14. Referrals sent elsewhere for 14/15 at 28 is now 78% of the entire 13/14 financial year total, indicating that the management of these urgent referrals has been challenging. This has been due to high overall demand for beds in early Summer 2014 in particular. Referrals Waiting over 24 Hours The number of children waiting over 24 hours for a bed after a tertiary referral continues to be below average. 90.5% of referrals were managed within the clinical target time which is lower than last month (91.9%). Tertiary and Home Urgent Referrals Sent Elsewhere Paediatrics T&O Plastic Surgery Resp Med Neurology Nephrology Medical Oncology ENT Clin Haem Cardiology Hepatology YTD 14/15 Tot 13/14 Trend - Tertiary and Home Referrals Waiting Over 24 Hours for a Bed 50 45 0 5 10 15 20 Long Term Trend Tertiary Refusals 40 35 30 25 18 16 14 12 10 8 6 4 2 0 20 15 10 5 0 Aug-09 Nov-09 Feb-10 May-10 Aug-10 Nov-10 Feb-11 May-11 Aug-11 Nov-11 Feb-12 May-12 Aug-12 Nov-12 Feb-13 May-13 Aug-13 Nov-13 Feb-14 May-14 Aug-14 Aug-14 Jun-14 lower ci Apr-14 Feb-14 Dec-13 Avge Oct-13 Aug-13 Jun-13 Apr-13 Feb-13 Avge Dec-12 Oct-12 Total Over 24 Hr Waits upper ci 11 PICU Demand and KIDS Service 1 West Midlands patient could not be supported within Region 3 non West Midlands patients could not be supported within Region 6 additional non West Midlands patients were supported at BCH PICU demand overall: Referrals in September have increased compared to the low level in August. However only 4 patients not be supported within the local network and had to be taken out of region. 250 There were 96 referrals to KIDS in September 2014 of which 33% of referrals were avoided , 43% were admitted to BCH, 20% were referred to other WM hospitals and 4% went out of the region (compared to 3% in previous month when referrals were very low). Year on Year Comparison of Total Referrals to KIDS 200 150 100 Referrals to KIDS Service Taken Out of Region (Leics or Other Non WM Provider) 50 0 Apr May Jun Jul Aug 2012/13 Oct 2013/14 Nov Dec Jan Feb Mar 2014/15 Outcome of Referrals to KIDS - Trend Aug-14 Jun-14 Apr-14 Feb-14 Dec-13 Total Oct-13 40% Aug-13 Jun-13 Apr-13 Feb-13 50% Dec-12 Oct-12 60% Sep 30 25 20 15 10 5 0 Avge 30% 20% 10% 0% Avoided Admission BCH UHNS and Other WM Out of Region The red line shows that BCH took fewer referrals in the first part of Winter 2013, but is now at more normal level. Despite the increase in referrals in September, more referrals were avoided. Therefore admissions taken OOR has not increased significantly. For the winter periods patients are more likely to be taken out of Region. However in June 14 in particular, due to high demand for beds, more patients were taken out of region but this has now returned to normal levels. 12 Operational Performance Report Month 6 2014/15 Performance for September 2014 Utilisation of our facilities 13 Cancelled operations trends Cancelled operations overall position: the number of cancelled operations flagged as nationally reportable in September 2014 is 26 and is below the monthly average and total for last month (28). Five of these cancellations were as a result of accommodating a liver transplant. For the second month running there were no breaches of the 28 day standard. Hospital cancelled operations on the day as percentage of elective operations has reduced again to 1.13%, (from 1.39% last month). The graph below shows this percentage is variable each month. Cancelled Operations On The Day - National Definition As a % of Electives Nationally Reported Cancelled Ops Jul-14 Apr-14 Jan-14 Oct-13 Jul-13 Jan-13 Oct-12 Jul-12 Apr-12 Jan-12 Oct-11 Jul-11 Apr-13 4 2 2 0 0 0 Sep-14 Contract Trajectory 0 1 4 3 Aug-14 Avge % Cancelled 0 2 Jul-14 0.0 3 7 5 Jun-14 10 6 May-14 0.5 7 Apr-14 20 Mar-14 1.0 11 Feb-14 30 Jan-14 1.5 Cancelled operations as a percentage of elective operations was 1.13%, lower than the last month (1.39%) The contract trajectory shown is for 1314, as one has not been agreed yet for 1415. Dec-13 40 lci 2stdev 16 Nov-13 2.0 18 16 14 12 10 8 6 4 2 0 Oct-13 50 uci 2stdev Breaches of 28 Day Cancelled Operations Standard Sep-13 2.5 mean Aug-13 % Cancelled 3.0 Data Jul-13 3.5 Apr-11 Apr May Jun 2012/13 Jun-13 28 350 300 250 200 150 100 50 0 -50 -100 May-13 54 All Hospital Cancelled Operations Apr-13 66 The total number of nationally reportable cancellations in September was below average at 26. In 48 mid month 2 elective lists were switched to Trauma, which should have a 28 26 positive effect on both cancellations and patient experience. A Trauma coordinator is now in place to Jul Aug Sep Oct Nov Dec Jan Feb Mar assist in identifying lists and 2013/14 2014/15 Avge for 3 years beds for these patients. Similarly we have created a surgical flow co-ordinator Percentage of Operations Cancelled on the Day post for 6 months to help 80 ensure we utilise as much capacity as possible in a 70 time of growing demand for our services 60 Total Cancelled 80 70 60 50 40 30 20 10 14 All Hospital cancelled operations year to date by specialty All Hospital cancelled operations year to date by reason Admi nistrative Error, 0.9% All Hospital Cancelled Operations 2014/15 Year to Date Other Dir 3, 0.6% Other Dir 4, 9.7% Ana esthetist una vailable, 3.0% Plastic Surgery, 13.0% Other, 4.7% Surgeon una vailable, 3.6% Other Dir 2, 6.5% T&O, 6.4% Hepatology, 4.0% Urology, 6.3% Haematology, 4.6% Cardiology, 3.8% La ck of theatre ti me, 5.0% Emergencies/Trau ma , 24.9% ICU/HDU beds una vailable, 5.7% Unfi t with acute i l lnes (Hosp Ca nc), 5.7% Cardiac Surgery, 8.8% Radiology, 7.6% Bed Shortage, 18.6% Opera tion not necessary (Hosp Ca nc), 13.1% Ophth, 4.3% Paed Surgery, 12.5% ENT, 11.8% Pa ti ent not suitable for OP, 14.8% Nationally Reportable Cancellations by Reason – Sep 2014 The hospital has cancelled 1288 operations so far in 2014/15. The Surgical Directorate has the most cancellations (825– 64.0%) with Plastics, Paediatric Surgery, ENT and Cardiac Surgery being the largest single specialties. The biggest reason for the YTD cancellations is Trauma and Emergencies (25%), bed shortages with 18%, patient not suitable for operation (15%) and operation not necessary 13%. For September the biggest reason is to accommodate emergencies and trauma (31%). Actions in place to try and alleviate this are outlined in the previous slide. Equipment failure Bed shortage Emergency/Trauma (of which 5 due to liver transplant) List overrun Admin Error ICU bed shortage Total 0 6 14 3 1 2 26 15 Multiple cancellations Patients cancelled more than once in same specialty during 2014/15 90 35 Cancelled Operations Associated With Patients cancelled more than once in same specialty during 2014/15 80 30 70 25 60 20 50 15 40 10 30 20 5 10 Twice 3 times 4 times 5 times 6 times 7 times Sep-14 Aug-14 Jul-14 Jun-14 May-14 Apr-14 Mar-14 Feb-14 Jan-14 Dec-13 Nov-13 Oct-13 Sep-13 Aug-13 Jul-13 Jun-13 May-13 Apr-13 0 0 Twice 3 times 4 times 5 times 6 times 7 times Strategic Objective – patients cancelled more than twice (Hospital Cancellations Only) In September 2014 27 patients had an operation cancelled who had previously had an operation cancelled at least once in the same specialty in the previous 12 months. These 27 patients had 62 cancellations between them in total in the previous 12 months in the relevant specialty. Six patients had an operation cancelled in September 2014 for the third or more time (NB cancellations have to be in the same specialty and in the previous 12 months to be counted) Strategic objective: Year to date hospital cancelled operations are running 321% higher than the equivalent year to date figure for 2013/14. (Target 10% reduction) Classification changes account for this in part. Strategic objective: For nationally reportable, one operation was cancelled due to admin error, and none due to equipment failure or unavailability (Target is zero) 16 Fit For Discharge Days Long Stay Patients From Summer 2013 to June 2014 there was an increasing number of longer stay patients in the hospital, as can be seen by the trend lines illustrating the numbers over 7, 30 and 90 days at any particular point in time. This had a significant impact on bed availability and cancelled elective operations. General Paediatric patients in particular were a problem area. In July and August 14 this cohort of long stay patients was significantly reduced, freeing up capacity on the wards overall and reducing the number of cancelled operations due to bed shortages. However this trend has reversed in September for those staying over 7 days and slight increase in those staying over 90 days 140 Inpatient Long Stayers by days 120 CAMHS - Long Stay Patients at end of September - Fit for Discharge Days Patient 5 Patient 3 Patient 1 0 100 200 300 Before fit for discharge 400 500 600 After fit for discharge 6 CAMHS patients were fit for discharge at end of September and are the same patients reported last month. All were waiting for placements. In total these six cases have been fit for discharge for 975 days. At time of writing this report one had been discharged and another was due for discharge. Long Stay patients at end of September - days fit for discharge 100 Patient 3 80 Patient 1 0 60 100 200 Before fit for discharge 40 20 03/10/2013 16/10/2013 29/10/2013 11/11/2013 24/11/2013 07/12/2013 20/12/2013 02/01/2014 15/01/2014 28/01/2014 10/02/2014 23/02/2014 08/03/2014 21/03/2014 03/04/2014 16/04/2014 29/04/2014 12/05/2014 25/05/2014 07/06/2014 20/06/2014 03/07/2014 16/07/2014 29/07/2014 11/08/2014 24/08/2014 06/09/2014 19/09/2014 02/10/2014 0 'GT7 ' GT30 'GT90 300 400 500 After fit for discharge 4 patients were waiting for discharge at end of September. Two patients were waiting for a care package (with one of these also having social issues), one needs social care and the final patient is waiting transfer to DGH. In total these 4 patients have been fit for discharge for 333 days. Assuming an average length of stay (excluding day cases) of 4 days, another 83 patients could have been seen at the hospital if these patients had been discharged, as they became fit. It is pleasing that delayed discharges have been decreasing over the last couple of months. 17 Item 14.219 Surgical Directorate Business case for a Mobile ‘Visiting Hospital’ 1 SECTION 1 EXECUTIVE SUMMARY NAME OF BUSINESS CASE: Proposal for a temporary theatre and ward unit on site. TYPE OF BUSINESS CASE: This case proposes the placement of a mobile theatre and ward unit known as a ‘Visiting Hospital’ on site that provides additional capacity for elective surgical admissions which will support a reduction in waiting times and achievement of the 18 week standard. 2 SECTION 2 BUSINESS NEED (WHY DO WE NEED TO CHANGE?) The Business Need – why do we need to change? The Trust has continued to be challenged with the size of the inpatient waiting list and there is a mismatch between capacity and demand. Despite undertaking a series of actions to increase efficiency and capacity the elective surgical waiting list has continued to grow. This is making it difficult to achieve access standards and there have been a growing number of patients waiting beyond 18 weeks for their definitive treatment. Recently due to National pressures to meet 18 weeks, commissioners have requested providers to submit recovery plans to reduce backlogs and sustain 18 week performance. Whilst it is known that through the Surgical Flow project further efficiency improvements can be made this case aims to provide a solution that will respond to helping reduce the backlog and put us in a much stronger position for changes to be made. The purpose of this business case is to propose the positioning of a temporary Visiting Hospital, which is a combination of a modular operating theatre and a modular ward at the front of the hospital. The next generation project will see the development of a clinical build which will accommodate additional theatres and associated bed capacity. However, once agreed this will take 2 years for it to become operational. BACKGROUND Work was undertaken with IMAS in 2013 to refresh the capacity and demand modelling undertaken in 2012, which continued to demonstrate a mismatch. Furthermore there has been a growing year on year demand in the majority of surgical specialties. To support this increase in demand additional weekend lists have been accommodated and in week capacity secured at the Birmingham Treatment Centre. Whilst this additional capacity has been accommodated it has significantly stretched resources and often fluctuates dependent on the availability of staff. Equally the utilisation of BTC is variable due to the limitations of case mix and age restriction. The current situation and existing arrangements Activity The following table provides the last 3 years elective Surgical (D4) activity which demonstrates the year on year increase, which has been delivered through a combination of new ways of working, additional weekend lists and capacity at the Birmingham Treatment Centre. 11/12 11,267 12/13 11,804 13/14 12,418 Demand A review of referrals and source has been undertaken. The below charts show the growth in referrals across 3 the high volume surgical specialties (Figure 1) and by CCG (Figure 2), comparing 2013/14 monthly average against Q1 2014/15 average. Figure 1 Figure 2 Capacity & Demand Gap Modelling of the ideal waiting list size to sustain and comfortably meet the 18 week standard was undertaken in November 2013 and Table 1 below highlights the challenges faced. Table 1 Ideal OPWL Size Actual OPWL Size Variance Ideal IPWL Size Actual IPWL Size Variance Urology 181 525 -344 153 277 -124 ENT 247 755 -508 300 412 -112 Paed Surgery 139 257 -118 222 243 -21 Plastics 202 328 -126 204 251 -47 Orthopaedics 210 386 -176 75 246 -171 Specialty It has been calculated that to reduce our backlog to our ideal WL size this would require 1 theatre operating for 6 months. To close our demand and capacity gap there is a requirement for an additional theatre. This is demonstrated in table 2 overleaf. 4 Table 2 Specialty Ideal WL Size to achieve 18 weeks Current RTT WL Size (excluding Planned) Backlog Additional Capacity Required to meet current Demand and 18 weeks (excl dealing with Backlog) 5 Sessions * Paediatric Surgery 200 264 64 = 32 theatre sessions Urology 153 272 2 sessions ENT 290 424 Plastics (inc CLEFT) 204 284(exc Laser) 119 = 40 theatre sessions 134 = 45 theatre sessions 80 = 40 theatre sessions Orthopaedics 75 239 0 Total 922 1483 164 = 82 theatre sessions 239 sessions Comments/Actions * Major /Minor split of cases needs further work as this could change the additional capacity required. 2 sessions 1 session Further work to review this by sub-specialty to understand where we need to focus the capacity. 10 sessions Cancelled Operations The Trust experienced significant pressure during the spring/summer months in terms of bed capacity and a number of elective admissions were cancelled across many specialties, particularly in April, where the highest numbers of on the day cancellations were reported (Figure 3). To avoid further cancellations on the day throughout May and June the surgical directorate were regularly cancelling patients the day before to avoid further disruption and anxiety (Figure 4). Figure 3 Figure 4 These cancelled operations have added further pressure onto the inpatient waiting list that is shown in Figure 5 overleaf. The specialties where there has been the largest increase are within ENT and Orthopaedics. 5 Figure 5 Whilst the Trust has achieved 18 weeks since April 2013 this continues to be challenged. Figure 6 below shows the 18 week performance of the surgical specialties (D4) since April 2013. Figure 6 92 90 88 Performance % 86 Target % 84 82 80 6 Figure 7 below shows the growth in the number of patients waiting 18+ weeks (dated & undated) since August 2012 to Sept 2014. Figure 7 There is currently no flexibility in the existing theatre plan with all theatres utilised to their full capacity Monday to Friday. There are a couple of exceptions where there are treatment rooms available but the types of cases are limited due to the size, specification and location of these. This means that when there is staff shortage, increase in emergencies or liver transplants, elective activity is often cancelled. Trauma demand has also increased year on year and when there are peaks in demand elective cases will be cancelled as trauma lists overrun into elective afternoon sessions. Figure 8 below shows the trauma demand for the past 3 years. Figure 8 New Ways of Working The surgical flow project will undoubtedly provide efficiencies with theatre scheduling and utilisation. However, it is recognised that the outputs of this will take time to be realised. The introduction of preassessment for all elective admissions and an admissions lounge will all help to improve flow of patients and utilisation of capacity. The mobile unit will provide an option for these changes to take place and provide the capacity needed to get us into a better position. 7 Fit with the Trust’s Strategic Objectives Our Vision The surgical directorate have a shared vision to provide excellent care that is nationally and internationally recognised with services that are innovative and which strive for improved patient outcomes through research and development. This involves strengthening partnerships with colleagues and stakeholders internally and externally within the health economy, wider community and our networks. We will place babies, children, young people and their families at the heart of what we do in a Directorate where performance stands out with high quality cost effective care. We wish to develop a new hospital with appropriate facilities for the local population and beyond, retaining and attracting the best calibre of consultants, nurses and other health professionals wanting to share in our success and vision. We have 4 strategic aims to • • • • Build the profile and reputation of services through listening and engaging with key stakeholders Enhance access and care with coordinated patient journeys Ensure that the services have the required resources, capabilities and capacity to meet demands and deliver high quality care To achieve a sustainable financial position Our vision and aims underpin the Trust’s Strategic objectives. We will have made year on year reductions in avoidable waiting at all stages of care The additional capacity this case will provide will ensure that we can improve on our 18 week performance and provide timely care for our patients. We will work with our partners to establish a range of mature clinical networks We wish to develop further hub and spoke arrangements for a number of our high volume specialties. This will compliment this case and ensure we can continue to meet the demand to our services. We will be able to demonstrate that no child has experienced avoidable harm Supporting this case will reduce waiting time for patients. We will admit children and young when they need us to and deliver services which are safe, effective, compassionate, innovative and child-centred in a healing environment In addition this proposal would fit with the long term goals of delivery of safe and effective services and delivering the best outcomes for children young people and their families. 8 SECTION 3 OPTIONS ANALYSIS Long list of options Option 1 – Do nothing – Continue to operate WLI and use of BTC Option 2 – Mobile Ward & Theatre Unit ‘Visiting Hospital’ with a link corridor into the main hospital Option 3 – Mobile Ward & Theatre Unit ‘Visiting Hospital’ without link corridor to the main hospital Option 4 – Increase provision off site, utilising other NHS or private provider facilities. Option 5 – Management of Demand Excluded Options Option Reason for Exclusion Option 3 Excluded based on reputational and safety factors Option 4 This already happens with the BTC but case mix and age restrictions limit utilisation. Option 5 Demand data has been shared with Commissioners and discussions are ongoing. However, the unit is to help manage patients currently waiting and therefore this option would not have the immediate impact. Short list of options Option 1 – Do nothing – Continue to operate WLI and at BTC Option 2 – Mobile Ward & Theatre Unit ‘Visiting Hospital’ with a link corridor into the main hospital 9 Options Analysis The analysis below appraises the mobile unit over a 26 month period starting February 2015 to March 2017 in line with the opening of the new clinical build in April 2017. FINANCIAL ANALYSIS £'000 Yr 0 Yr 1 Yr 2 14/15 15/16 16/17 2 months 12 months 12 months BENEFITS TOTAL working ref Income 1 311 1,635 466 2,412 Loss of car park 2 -31 -98 -98 -228 280 1,536 367 2,184 Total Benefits COSTS 0 Revenue 0 Pay 3 171 1,024 1,024 2,218 Hire of unit 4 894 0 406 1,300 Consumables 5 18 98 38 155 B Braun 6 3 14 6 22 Facilities 7 6 35 35 75 Utilities 8 1 4 4 9 Reduction in premia pay 9 -8 -47 -591 -645 Reduction in BTC hire 10 -34 -202 -202 -437 One off costs: 0 Theatre Trays 11 153 0 0 153 Framework registration 4 6 0 0 6 Cleaning equipment 12 5 0 0 5 Capital: 0 Works - corridor 13 21 124 145 289 Works - MDC door 14 0 1 1 1 CCTV 15 0 2 2 4 1,235 1,053 867 3,155 -955 484 -500 -971 Total Costs Net (Costs) / Benefits 10 Notes 1. Income An options appraisal has been undertaken that has evaluated how the unit could be used and the proposed case mix. These are shown in Appendix 1. This case mix takes account of current demands, including backlog and risks to RTT delivery. The growth in terms of demographics and market share have been assessed in conjunction with the planned efficiencies through Newton, which are shown below: Activity Specialty Urology ENT T&O Plastics Paed Surg Maxfac Ophthalmology Target improvement 7% 13% 8% 9% 9% 7% 8% Additional 98 92 81 79 0 0 22 Repatriation of BTC 0 93 Weekend activity 0 196 0 66 43 12 17 The impact of this has necessitated evaluation of further specialities to ensure that there is sufficient activity demand to maximise utilisation of the mobile unit. Once all backlog and unmet demand is absorbed then the activity will be an in week repatriation of premium weekend activity and urology activity currently delivered at Birmingham Treatment Centre (BTC). The income has been calculated using the average tariff by speciality for new activity only. The financial impact of repatriating activity is reflected in a reduction in costs. 2. The loss of car park income relates to the 27 car park spaces which will be removed at the front of the site. Expenditure 3. Pay The unit will operate 5 days a week between 8am and 6pm. Nursing and operating department practitioners can be supplied directly from Vanguard. It is recommended that at least one member of Vanguard personnel is hired to maintain an onsite presence and be responsible for the day to day functioning of the unit, which includes daily stock keeping. If this service is purchased then the unit can be deemed a healthcare facility and VAT payable on the hiring of the unit and staffing can be recovered, which is a significant financial advantage. Recruiting the remaining staff will provide in house capability and a phased approach which will maximise development and service delivery. This will also mean that a trained and embedded theatre team will be available in readiness for the new theatres contained within the Next Generation project. a. Consultants and Juniors: An increase of 10 sessions per week will require 2 Anaesthetists which have been costed at mid-point. Although the additional ENT sessions can be met through existing consultant workforce, locum consultants will be required for Urology, Trauma and T&O. These are included in the financial analysis with further junior support for Trauma and T&O. 11 b. Theatre and recovery/ward staff: Theatre staff will work a 4 day week, 8am – 6pm through a standard 10 session week rota. It is recognised that recruitment to posts will require an implementation and training programme with potential reliance on bank and agency in the interim. Bank and agency pay costs have therefore been used in the financial analysis for the following manpower: Theatre Team: Surgical Nurse ODP – hired from Vanguard Anaesthetic nurse Nurse Nurse Recovery staff: Recovery practitioner Recovery Nurse CSW – Ward CSW - Ward Band 6 5 5 3 2 Number 1 1 1 1 1 5 2 5 3 2 1 1 1 c. Administration: A full time band 3 ward clerk has been included at mid-point and will act in a coordinator role, managing all referrals to the mobile unit. d. The increase in activity will require additional clinical support services, which has been estimated as: Department Labs Labs Labs Imaging Ambulatory Care Ambulatory Care Ambulatory Care Ambulatory Care Service Histopathology Microbiology Blood Science Radiology Phlebotomy Pharmacy Technician Physio WTE 0.2 0.5 0.3 0.6 0.25 0.2 0.5 0.5 e. Cleaning and portering pay costs have also been incorporated in the financial analysis. Non-Pay 4. Hire of unit: A reduced weekly hire charge for the combined operating theatre and ward unit has been negotiated which presents better value for money the longer the unit is on site. The maximum reduction to £11,000 per week is available when hired for 18 months or longer. A further 10% reduction can also be guaranteed when procured through the North of England NHS Commercial Procurement Collaborative. BCH does not currently have access to this framework so a £6k registration fee will apply. The financial analysis assumes full payment of 18 months hire on arrival of the unit with the hire charges after this period paid in respective months. As detailed above, VAT is recoverable if the unit is deemed a healthcare facility. This requires certain criteria to be met which include Vanguard staff stocking the unit daily. Sourcing the ODP through the contract will achieve this however the final contract will need to be reviewed by the Trust’s VAT advisors before this can be guaranteed (initial discussions have already taken place which we have acted upon in deciding how the unit will operate). The risk of not recovering VAT is low as this is adopted at other providers accommodating 12 a Vanguard unit. The charges in the financial analysis and in the table below are therefore excluding VAT. Framework Fee Cost Saving (from original quote) over duration Per week Per week Price via Procurement Framework 6 months £15,000 £15,000 £13,500 £6,000 £33,000 12 months £15,000 £14,000 £12,600 £6,000 £118,800 18 months or longer £15,000 £13,000 £11,700 £6,000 £251,400 Original quote Revised quote Duration 5. Consumables are estimated at £3k per week for one theatre plus £30 per patient for drugs which is the average cost year to date. This applies to new activity only as the consumables for current weekend and BTC activity are already within baseline. 6. The sterilisation of theatre trays has been calculated using suggested case mix, volume, tray category and current contract price. These costs apply to new activity only as already in place for current BTC and weekend activity. 7. Facilities: costs include linen, waste, post, catering, patient transport, disposables and post. 8. Utilities: Additional charges for electric and water 9. Reduction in premium pay: The analysis assumes 23 weekend sessions are transferred in week during 15/16 with a further 300 sessions being transferred in 16/17. The associated saving in premium rates are therefore included. 10. Reduction in BTC hire: Repatriating 72 sessions per year of urology activity from BTC will eliminate hire charges of £2,800 per session. No formal SLA is in place for this service hence no notice period exists. One-off costs 11. Theatre trays: The case mix in option 2 has been reviewed and extra trays identified. Expansion of specialities may lead to further trays being required, however this is dependent on speciality and timing of the additional sessions. Although the full cost has been included in the financial analysis, trays have a useful estimated life in excess of 2 years and can therefore be used in the new theatres contained within the next generation project 12. A cleaning machine will be required as the current machines cannot be used due to mobility restrictions. Capital 13. A corridor is required to link the operating theatre to the ward unit and full connection to the main hospital. The design and construction fees have been depreciated against a 26 month duration and cover: a. Fees for the design, planning application and building regulations. b. Site set up costs and building work for an enclosed corridor and fire exit ramps. This includes all mechanical and engineering required. c. Water connection from the hospital boundary to MDC. 13 d. e. 5% contingency. Provision of £5,000 for removal of the corridor 14. The outside door at MDC will need to be widened to provide an emergency route or transfer patients who may not recover as anticipated and need to stay overnight. This will also make the door compliant with DDA regulations. The current width presents a risk as it is not wide enough to allow a standard bed trolley to pass through it. 15. Additional CCTV provision is recommended and has been factored into the analysis and depreciated over the life of the current system. Further considerations: In the first 12 months, over 80% of activity relates to current backlog or growth after Newton efficiencies. During this period the deficit reduces month by month as additional income is received. As repatriation of current activity replaces backlog activity the income reduces without cost reductions only partially offsetting this. At this point the deficit begins to increase and continues over the remaining period. Although an 18 month contract is needed to guarantee the full reduction in hire charges a review of activity will be required at the 12 month point to assess growth assumptions and any potential opportunities. At this stage a decision will be made on whether the Mobile Unit will be required through to April 2017. Affordability: The Trust has been successful in negotiating additional monies for Winter and RTT. These will be received during 2014/15 and will have to be used in that timeframe. This affords us the opportunity to utilise part of these monies to fund the 2014/15 deficit. The impact of this decision and the resultant I&E positions in 2015/16 and 2016/17 are outlined in the table below. Year 0 Year 1 Year 2 Overall 2014/15 2015/16 2016/17 £000 £000 £000 £000 Original Position -955 484 -500 -971 Confirmed RTT and Winter Funding 955 955 Total Impact on Existing Planned Surplus 0 484 -500 -16 Original Surplus 4761 4008 4221 Revised Surplus 4761 4492 3721 The case will provide a further benefit to the Trust’s finances in 2015/16 and as a result the planned surplus increases to £4.492m. As the case presently stands there is a reduction in the planned surplus in 2016/17 to £3.721m. However, with the review at 12 months a further assessment of the impact on 2016/17 will be undertaken so this is the worst case scenario. Overall, with the utilisation of the RTT and Winter monies the case has a net deficit of £16k. In cash terms this case essentially has a nil impact (an overall reduction of £16k) so does not impact upon the affordability of the Trust’s strategic ambitions around Next Generation. A further consideration, although not factored into the case is the positive impact this will have on the potential for the Trust to incur contract penalties. This unit will provide greater resilience and lessen the risk of this being incurred. 14 Evaluate how well each option meets the evaluation criteria using the table below. Option description Option 1 – Do nothing Option 2 Evaluation Criterion Raw Score (1-5) Raw Score (1-5) 1 3 Achievability (See table below) 2 4 Risk of doing (See RISK ASSESSMENT SCORING) 3 1 Financial Viability (See table below) 1 5 OVERALL SCORE (SUM TOTAL) 7 13 Strategic fit (See STRATEGY SCORING table below) 15 STRATEGY SCORING Rank the options against each of the below objectives of the Trust. A score of 5 for example would mean that the option has a high strategic fit, whilst a 1 is a low strategic fit. Short term objectives All children referred for inpatient care will be admitted within 24h of referral We will have made year on year reductions in avoidable waiting at all stages of care All children presenting at our Emergency Department requiring inpatient admission will be admitted within 4 hours We will be able to demonstrate that no child has experienced avoidable harm We will work with our partners to establish a range of mature clinical networks We will develop at least one annual campaign at local, regional and national levels centred on children’s rights, health and wellbeing issues Long Term Objectives Option 1 – Do nothing Option 2 0 3 1 4 0 2 1 3 0 0 0 0 Option 1 Option 2 We will admit children and young when they need us to and deliver services which are safe, effective, compassionate, innovative and child-centred in a healing environment We will work with our partners to deliver care as close to home as possible Our intentions will be delivered by advocacy for the best outcomes for children, young people and their families TOTAL SCORE 1 3 0 0 3 3 6 18 SCORE FOR INSERTION IN SUMMARY TABLE (DIVIDE TOTAL BY 8 AND ROUND TO NEAREST WHOLE NUMBER) 1 2 16 Criteria Achievability Financial Viability (See EXCEL WORKBOOK) Score of 1 (Low) Score of 5 (High) The investment requires significant change management, reorganisation and additional capacity and resources. There is no / limited evidence of similar projects delivering success. There is existing capacity and capability within the organisation and the timescales and scope are realistic and achievable. Costs significantly outweigh benefits (additional income and efficiency savings) and the required investment exceeds available resources. Benefits outweigh costs and the required resource is available to deliver the whole proposal. 17 RISK ASSESSMENT SCORING Results Option 1 Option 2 Measurement of Consequence (1 to 5) 4 2 Measurement of Likelihood (1 to 5) 4 3 Raw Risk Assessment (i.e. Consequence x Likelihood) 16 6 Overall score from above divided by 5 and rounded to nearest whole number 3 1 Taking the scores from total score from the now completed first table, the options can be evaluated against each other. OPTIONS EVALUATION Options Evaluation Score Ranking Proposed Solution? (Yes / No) An explanation should be provided here where the proposed solution is not the option with the highest score. Option 1 Do Nothing Option 2 7 2 No 13 1 Yes 18 SECTION 4 PROPOSED SOLUTION Project Scope Visiting Hospital providing mobile theatre and 8 bedded ward area with a link corridor to the main hospital for 18 months In Scope: Providing additional capacity for Urology, ENT, Orthopaedics and Trauma Out of Scope: A Task & Finish Group was set up to develop this case. An options appraisal was undertaken to review how the unit could be used and the case mix. As previously described the preferred option is Option 2 which is shown below:Monday Tuesday Wednesday Thursday Friday Mobile Urology Plastics ENT MaxFac/Dental ENT Theatre 8 Plastics All-day Trauma Spinal All-day Trauma Plastics/Maxfac Theatre 6 Trauma/T & O El Ortho Trauma/T & O El Ortho Trauma/T & O Theatre 2 Cardiac Cardiac Emergency Plastics Cardiac A standard operational procedure is currently being developed that will provide a process for patient admission into the unit. The unit will be linked to Medical Day Care which will provide an entrance for patients/parents on admission. The link corridor to the main hospital provides an emergency route or a transfer route for patients who may not recover as anticipated and need to stay overnight. The benefits of this mobile unit are:• • • • • • • • Provide additional capacity for Trauma, Orthopaedics, ENT & Urology Reduction in cancelled operations due to trauma Provides associated bed capacity to compliment additional theatre activity Reduction in waiting times for patients Support achievement of 18 week standard Reduction in backlog (patient waiting over 18 weeks) Will bridge the gap between demand and capacity Will enable flexibility for the management of liver and trauma activity 19 • Enables new ways of working through the surgical flow to be embedded STAKEHOLDER MAPPING TEMPLATE Stakeholder Group Patients GP’s Consultant staff Parents / carers Perceived Benefits Improved Access Improved Access Manageable work load Better access and treatment for patients Changes Needed Increase capacity Increase capacity Improve theatre and clinic utilisation Increase capacity Perceived Resistance None Negative None None None Neutral Positive C R C R C R C R C= CURRENT COMMITMENT R= REQUIRED COMMITMENT Stakeholder Analysis Patients: Patients are key and at the centre of all that the Trust does. This business case would improve patient access and reduce waiting times. GPs: Will experience easier referral streams into the service due to an increase in capacity. Parents / Carers: Although they are not the patient, parents and carers are key to the success of the Trust. This project will improve the treatment of patients and in turn the experience of parents and carers. 20 SECTION 5 RISK ASSESSMENT Summary Risk Table Risk Description Score Responsible Individual Cost* (£) Locum/Agency Recruitment of theatre & anaesthetic staff VAT applied to the hiring of the mobile unit is not recoverable Mitigation Strategy Use of Vanguard staff 4 Use of Vanguard staff to stock unit £260K (over 26 years) Final contract to be reviewed by VAT advisor Unknown Risk of council tax increasing as use and income generation of land will change *Cost of dealing with the risk if it were to materialise. 21 SECTION 6 BENEFITS ANALYSIS Summary Benefits Table Ref Critical Benefits C1 Increase in weekday and job planned theatre time delivering required activity at a lower cost C2 Improved capacity and reduction in 13 week outpatient, 18 week RTT and 26 week inpatient targets C3 Provide additional trauma capacity Measurement Basis Base / current Value Target Value Target Date Improved performance against target 13 weeks – 100% 100% December 2013 26 weeks – 99.6% 100% Base Value / current Target Value Reduced overruns Reduced cancelled operations Ref A1 A2 Additional Benefits Improved reputation of the Trust due to improved access targets Provides flexibility in theatre plan to undertake additional weekend lists reduce backlog and/or provide private capacity A3 Maintains market share A4 Fits with Trust Strategy and Medium Term Estate projections A5 Minimises risk of contractual penalties enforced by the commissioners in term of cancelled A6 Recruitment and training of Anaesthetists and theatre team will result in an embedded team being A7 Measurement Basis - - One off costs which include theatre trays and cleaning machine can be utilised in the next generation - - - - - - Residual value after 2 years of £122k 22 Target Date SECTION 7 PROJECT DELIVERY Project Plan Table Milestone Activity Responsible Individual Start Date CSD, ASD and CFM approval LC Sept 14 Operational Leadership Team (OLT) Approval (if required) Investment Committee Approval (if required) Capital Planning Group (CPG) Approval (if required) Finance and Investment Committee (FIC) Approval (if required) Completion Date LC 7/10/14 LC 16/10/14 End of Oct 2014 Post Implementation Review 1 23 End Date 6/10/14 14/10/14 Time Requirement SECTION 8 FUNDING Funding Table Total Funding Required Funding for Capital or Revenue Spend? Source of Funding Funding constraints £0.35m Capital Winter/RTT monies Commissioner support £0.016m Over 3 years Revenue Growth/Backlog Repatriation Winter/RTT Commissioner support The FRC is asked to approve the funding requirements above. 24 Approvals required and / or date obtained APPENDIX 1 OPTION 1 Monday Tuesday Wednesday Thursday Friday Plastics Plastics Urology Plastics Plastics/MaxFac Theatre 8 ENT/Urology (?alternate) All Day Trauma Spinal All-Day Trauma ENT Theatre 6 Trauma/T & O El Ortho Trauma/T & O El Ortho Trauma/T & O Cleft Cleft Cleft Cleft Cleft Mobile Theatre 9 pm session OPTION 2 Monday Tuesday Wednesday Thursday Friday Mobile Urology Plastics ENT MaxFac/Dental ENT Theatre 8 Plastics All-day Trauma Spinal All-day Trauma Plastics/Maxfac Theatre 6 Trauma/T & O El Ortho Trauma/T & O El Ortho Trauma/T & O Theatre 2 Cardiac Cardiac Emergency Plastics Cardiac OPTION 3 (with Existing Theatre Plan) Mobile Monday Tuesday Wednesday Thursday Friday Urology Ortho/PS&U ENT Plastics ENT OPTION 4 Mobile Theatre 8 Theatre 6 Theatre 7 Monday Tuesday Wednesday Thursday Friday AM ENT ENT Urology ENT ENT PM ENT Plastics Urology Plastics ENT AM Plastics Trauma Spinal PM Plastics Plastics Spinal Plastics Plastics/Maxfax AM Trauma EL Ortho Trauma EL Ortho Trauma PM Ortho EL Ortho Ortho EL Ortho Ortho AM ENT Trauma ENT Trauma ENT PM ENT ENT ENT ENT ENT 25 Trauma Plastics/Maxfac Board of Directors Item 14.220 Thursday 30 October 2014 Enc 04 Strategic Objective/ Enabler Every child and young person requiring access to care at BCH will be admitted in a timely way, with no unnecessary waiting along their pathway Report Title Resources report period 1st April 2014 – 30th September 2014 Sponsoring Director Chief Finance Officer Author(s) Director of Finance and Procurement, Chief Officer for Workforce, Head of Informatics Previously considered by Finance and Resource Committee Situation This report is to communicate the various aspects of Trust performance in the financial year to date, period ending 30 September 2014, and to identify any key risks that are evident within the organisation. The contents of this report will form the basis of the Trust’s Quarter 2 (Q2) Return to Monitor. The Trust is also required to report its predicted status for Governance and Mandatory Services. Background The Trust is required to comply with the finance related legal issues contained within our Terms of Authorisation as well as other key financial targets. This includes: • • • • Not breaching the Private Patient Cap (a legal requirement); Performing at plan for Monitor’s Continuity of Service Risk Rating leading to an overall CoSRR of 4; Minimising triggering the additional financial indicators; and the Risk Assessment Framework, which may result in formal discussions with Monitor. Delivery against these targets is driven by: • • The volume and mix of demand experienced by the Trust; and How the Trust uses its most valuable resource, its staff, in responding to that demand. The report explores each of these areas in turn and the impact on the financial position and performance. Assessment Monitor Declarations The key ongoing governance issue which impacts upon the Trust’s Monitor Governance rating is the performance against the 18 week target for admitted patients. Performance in month was, at 90.3%, above the 90% threshold. This, and the continuing level of performance of the other metrics, enable the Trust to forecast a Green Governance rating. From a financial perspective the ratings will be a 4 under the Continuity of Service Risk Rating. Under the old Compliance Framework a FRR of 4 would also have been reported. These remain strong performances. Activity Activity performance in the year to date against plan and compared to 2013/14 is as follows: Activity Type Against Plan Against 2013/14 Emergency Department +5.0% +4.8% Emergency/Non-Elective -4.8% -8.2% Planned Care +3.2% +4.4% Outpatients +5.0% +8.9% From a financial perspective income has overperformed by £0.6m in the month. This is the second month of above plan performance some of which was a result of the discharge of some long stay patients. These discharges and the increasing level of drug and device recharges are masking the financial impact of the level of cancelled operations and the causes of these cancellations as reported in the Performance Report. Workforce Demand remains high and this has brought into sharp focus the short to medium term capacity issues faced by the Trust. Sickness levels increased in the month and stood at 3.06%. The cumulative rate remained at 3.44% meaning both measures are above the Trust’s 3% target albeit fractionally in the in-month case. The combined substantive and bank staff level increased by 16wte in September. Bank use decreased by 12wte whilst substantive staffing increased by 28wte. Compared to September 2013 substantive wte have increased by over 5%. Engaging with staff, especially during periods of pressure, is important and appraisals are one indication of how well this is working in the Trust. The reported appraisal rate is now 82%, an increase of 3% on the position reported in August. Finance The end of the second quarter sees the Trust continuing to perform below plan. An inyear surplus of £2.7m sounds strong. However, it falls short of the plan submitted to Monitor, and is well below the levels reported in the final 6 months of 2013/14 and we have to be mindful that the plan we set was at the lower-end of expectations. September is traditionally a transition month where income increases from the lows of the summer months into October and November when financial performance is usually strong. Controlling the costs of care that we provide remains central to our financial success as downward pressure continues on the tariffs we are paid. Our savings levels are below target in September. The key areas of shortfall include trust-wide schemes (contract penalties, future fit and drugs) and it is vital that all trust-wide schemes are delivered given that these constitute 50% of the plan this year. We have to secure the level of savings that we anticipate this financial year to ensure affordability of the Next Generation project and having plans exceeding 100% of our target is a positive move to achieving this. The delivery of Directorate CIP savings has reduced significantly in September and October sees a large increase in month on month targets. The key issue financially in Quarter 1, which has continued into Quarter 2, has been the impact of cancelled operations on clinical income, which is £0.2m under target. This is an improvement in month due to the discharge of long stay patients and increasing levels of drug and device expenditure. Our cash balances are above plan. The September position was the Trust’s largest ever closing cash balance although this has been partly assisted by an underspend on the capital programme. The Capital Programme was ratified by the Finance and Resource Committee in July. Expenditure levels in Quarter Two are lower than expected due to delays on several key schemes. The overall forecast is to meet the revised target of £12.8m. Forecast The revised forecast at year end is now a surplus of £4.8 million. This is the first time this year that the original plan has been uplifted. The driver behind this £0.4m increase is the receipt of additional winter and RTT monies. Although the majority of these are covered by an offsetting revenue cost, there is a need to commit £0.4m of the cash received to capital. This funding cannot be spent twice so it has to be recorded against I&E. Monitor Month Data Collection On September 15th all FTs were written to outlining a new monthly data collection exercise predicated on the emerging signs of pressure on NHS finances. This requires a return to the DH confirming the Trust’s Forecast Outturn positions on revenue and the overall level of capital expenditure. This is again included within the Resource Report. Recommendations The Board review, discuss and approve the Resources Report. The Board of Directors is asked to approve a forecast Governance (Green) and Continuity of Service Risk Rating (“4”) for inclusion in the Monitor Q2 Return, which must be submitted by October 31. Key Impacts Strategic Objectives Staff and finance are key enablers to meeting the Trust’s strategic objectives. CQC Registration (state outcome) N/A NHS Constitution NHS Constitution has a pledge regarding 18-week waits. Other Compliance (e.g. NHSLA, Information Governance, Monitor) Monitor metrics are considered in the report. Equality, diversity & human rights N/A Trust contracts N/A Other N/A Resources Report October 2014 Phil Foster Theresa Nelson Paul Franklin Director of Finance and Procurement Chief Officer for Workforce Head of Informatics 1 Reporting on resources use. 1. Summary 2. Governance - Monitor Assessments and Declarations 3. Financial Performance 4. Income and Expenditure 5. Efficiency 6. Liquidity 7. Workforce 2 Summary. September 2014 The second quarter has concluded with the Trust continuing to perform slightly below financial plan. The year to date surplus of £2.7m is a relatively strong position but it does fall short of the plan submitted to Monitor and is also below the average monthly surplus reported in the second half of 2013/14. Achievement of the Trust’s planned £4.4m surplus is expected and this is confirmed by the forecast outturn assessment, but this will use some of the reserves set aside. With the receipt of additional winter and RTT monies some of which will have to fund capital expenditure the overall forecast has been increased by £0.4m to £4.8m. However, the plan was widely accepted as being a downside case which makes the combination of continued underperformance and Directorate positions a worrying scenario. The operational difficulties at the Trust with regards to PICU and acute bed capacity and numbers of long stay patients, are leading to high levels of total cancelled operations. This is having a direct impact on clinical income which remains below plan. October is a month of expected higher activity and the financial target for that month reflects that. Controlling the costs of care that we provide remains central to our financial success as downward pressure continues on the tariffs we are paid. Our savings levels are below target in September despite starting the year more strongly than in 2013/14. It is crucial that the trust-wide schemes are delivered but these too are being impacted by the operational difficulties being experienced. We have to secure the level of savings that we anticipate this financial year to ensure affordability of the Next Generation project and having plans exceeding 100% of our target is a positive move to achieving this. September has seen a smaller fall in savings delivery than previous months but the in-month targets rise from October onwards and this is reflected in a reduced achievement percentage. Bank usage in September was 17% lower than the equivalent period last year although substantive staffing levels are 5.2% higher. Appraisal rates are at 82%, which is 3% higher than the level reported in the August report. In-month sickness increased by 0.08% to 3.06%. Year to date sickness has remain static at 3.44%. Our cash balances remain strong although their performance has been assisted by a lower than planned capital spend due to delays in key schemes. 3 2. Governance – Monitor Assessments and Declarations 4 Our Month 6 regulatory position remains strong. Quarter 1 - 2014/15 The ratings for Quarter 1 have been confirmed by Monitor. Monitor Quarter 1 2014/15 (Confirmed) Finance risk rating - Continuity of Service Risk Rating Governance risk rating Finance risk rating - Compliance Framework Month 6 – Quarter 2 Based on this performance the predicted measureable Month 6 performance is Green. Plan Actual G (4) G (4) G G G(4) G(4) Monitor Quarter 2 2014/15 (Predicted) Finance risk rating - Continuity of Service Risk Rating Governance risk rating Finance risk rating - Compliance Framework Plan Actual G (4) G (4) G G G(4) G(4) The Continuity of Service Risk Rating for September is a 4 (the highest level). For information under the old Compliance Framework regime a FRR of 4 would have been reported in Month 4. A continuation of the above will result in the Trust achieving its planned Risk Ratings for 2014/15. Forecast ratings for the year are included in Section 2 – Financial Performance. 5 Monthly Reporting Collection Data. On 15 September Monitor wrote to all FTs outlining the requirement for a new monthly data collection process. For October (and therefore reporting of September’s figures) the information requested is required to be returned by October 24th. The requirements and the September figures are outlined below. DH monthly reporting data from Birmingham Children's Hospital NHS FT as at 30 Sep 2014 Question No Question text 1 What is the trust's Surplus / (deficit) before impairments and transfers by absorption 2 What is the trust's Capital Expenditure, net of disposals, on an accruals basis Plan value from 14-15 APR or latest re-planned value in £m at 30 Sep 2014 Actual Value in £m at 30 Sep 2014 Forecast value in £m as at 31 March 2015 only enter numbers below only enter numbers below only enter numbers below 2.825 2.710 4.761 12.579 4.017 12.834 6 2. Financial Performance 7 Financial Summary. Governance The Monitor Financial Risk rating is 4 per plan, with liquidity remaining strong. This 4 is per the Continuity of Service Risk Rating (CoSRR) and also the former Compliance Framework. Income and Expenditure The I&E position is below the Monitor plan and the revised plan at £2.710m. The Forecast position for the Trust has increased to £4.761m. This includes the I&E benefit of the proportion of additional winter and RTT monies that will be used to finance capital expenditure to enable the use of a mobile theatre at the Trust. Efficiency The EBITDA and Income Surplus margins are 5.2% and 4.2% , respectively. Both of these are marginally below plan. CIP at a Directorate level and Trust-wide level is below plan. This remains the primary financial focus and will be a key component of Directorate recovery plans. Performance is at 81% and is forecast to drop to 76%. Productivity measures associated with income are mixed with income per wte above plan for the second month in succession. Liquidity Cash balances are above plan in September mainly as a result of a shortfall in capital expenditure. 8 Financial Balanced Scorecard. FINANCIAL BALANCED SCORECARD - SEPTEMBER 2014 Plan Governance Continuity of Service Risk Rating * I&E Liquidity Efficiency Actual Variance YTD 4 4 0 Continuity of Service Risk Rating * Forecast 4 4 0 Governance Risk Rating YTD Green Green Governance Risk Rating Forecast Green Green I&E Position (£m) In-Month 0.66 0.58 -0.09 I&E Position (£m) YTD 2.82 2.71 -0.11 I&E Position (£m) Forecast 4.38 4.76 0.38 Profitability - EBITDA (£m) YTD 6.55 6.33 -0.22 Profitability - EBITDA (£m) Forecast 11.82 12.16 0.34 Debt Service Cover Rating * YTD 4 4 0 Debt Service Cover Rating * Forecast 4 4 0 Cash (£m) YTD 49.20 51.00 1.80 Cash (£m) Forecast 45.49 46.49 1.00 Capital Expenditure (£m) YTD 5.70 4.00 -1.70 Capital Expenditure (£m) Forecast 12.74 12.84 0.10 Liquidity Rating * YTD 4 4 0 Liquidity Rating * Forecast 4 4 0 CIP Achievement (£m) In-Month 0.72 0.69 95% CIP Achievement (£m) YTD 3.61 2.92 81% CIP Achievement (£m) Forecast 9.46 7.14 76% Income per £1 Pay Expenditure (£) YTD 1.61 1.58 98% Income per wte (£) In-Month 72.78 73.19 101% Contract Penalties/CQUIN Loss (£m) YTD 0.00 -0.21 -0.21 Contract Penalties/CQUIN Loss (£m) Forecast 0.00 -0.38 -0.38 RAG * Note - for those Monitor Ratings - 4 is the Highest Rating 9 3. Income and Expenditure 10 Income and Expenditure against Plan. The Trust’s I&E position has improved slightly in September with an overall deficit against plan of £0.15m now being reported. This is an improvement of £0.15m. Headlines are: • The Trust is reporting a reducing (£0.2m from £0.8m) deficit against Clinical Income. This is a third month of improvement and reflective of the increased clinical activity throughout the Trust; • Part of the clinical improvement is associated with drugs and devices income for which there is a direct offsetting cost; • Pressures continue to be felt in Directorates and mainly arise from operational performance issues around cancelled operations and previously high levels of long stay patients. The impact of this clinical income performance is being particularly felt in Specialised Services and Surgery. • Activity performance is covered in further slides within this section; • Additional Directorate pressures are experienced through the phasing and delivery of CIP targets and the costs of agency staffing. CIP performance is detailed in 4. Efficiency section. • CIP performance is causing operational financial difficulties with the majority of Directorates overspent; • The continued use of temporary staffing is adding unfunded costs into system. The spend in this area over the first 6 months exceeds £3.9m and equates to 5.1% of the overall pay bill for the first half of the year (7.6% for the equivalent period last year); 2014/15 I&E to September 2014 Income from activities Other Income Operating Expenses EBITDA Interest Receivable Depreciation Profit/(Loss) on Asset Disposal Impairment PDC Dividend Interest Paid Net Surplus/(Deficit) Annual Revised YTD Plan Plan per Annual Plan per LTFM LTFM £'000 £'000 £'000 217,995 217,517 109,864 19,666 22,949 9,603 -225,841 -228,684 -112,921 11,820 11,782 6,546 243 247 122 -4,624 -4,559 -2,312 0 0 0 0 0 0 -2,762 -2,762 -1,381 -300 -326 -150 4,377 4,381 2,825 Revised YTD Plan £'000 109,760 11,570 -114,770 6,561 124 -2,280 0 0 -1,381 -163 2,861 YTD Actual £'000 109,518 11,927 -115,114 6,331 86 -2,302 0 0 -1,263 -141 2,710 Variance £'000 -242 356 -345 -230 -38 -22 0 0 118 22 -151 • A detailed I&E breakdown is included as Appendix One. • A detailed breakdown of expenditure by cost category is included as Appendix Two. 11 Income and Expenditure Forecast. The half-way point of the year has generated a more detailed forecast. This is included as Appendix Three. The forecast has been generated through a detailed assessment of clinical income derived through the SLAM system followed by a thorough review and assessment at Directorate level. This position is predicated on a number of assumptions and these will continue to be developed in the coming months. The revised forecast at year end is now a surplus of £4.8 million. This is the first time this year that the original plan has been uplifted. The driver behind this £0.4m increase is the receipt of additional winter and RTT monies. Although the majority of these are covered by an offsetting revenue cost, there is a need to commit £0.4m of the cash received to capital. This funding cannot be spent twice so it has to be recorded against I&E. This is based on the following factors: • The second half of the year has a greater level of CIP schemes to be delivered; • Achievement of the Newton efficiencies; • A continuation of contract penalties and provision for CQUIN shortfalls; • A reduced level of donated asset benefit due to scheme delays; • Impact of reduced PICU income as a result of less than 31 beds being open; • Reduced income associated with partially completed spells; 2014/15 Forecast Income from activities Other Income Operating Expenses EBITDA Non-Operating Inc & Expenses Net Surplus/(Deficit) • • • • • Annual Revised Year-End Plan per Annual Plan Forecast LTFM £'000 £'000 £'000 217,995 217,517 218,585 19,666 22,949 24,968 -225,841 -228,684 -231,392 11,820 11,782 12,162 -7,443 -7,400 -7,400 4,377 4,381 4,761 Variance £'000 1,068 2,019 -2,708 380 0 380 Continued premium rate expenditure; No benefit of any provisions made during 2013/14; The receipt of, but no gain from, additional winter monies; Impact of ED Observation changes; Next Generation costs. The forecast position will be updated on a monthly basis with review by the CFO on the 10th working day as part of the monthly reporting schedule. 12 Emergency activity profile. Emergency Department (ED) attendances in September have increased following the expected August reduction in activity. The September level is 7.6% above last year however so this is higher than would be anticipated as we start to move towards Winter. Overall activity has increased by 4.8% year to date compared with last year. ED attendances 6000 5000 4000 3000 Regarding performance vs plan, Activity is 7.4% above plan for the month and 5.0% above plan in 14/15 so far. 2000 1000 0 A M J 2011/12 J A S O 2012/13 N D J 2013/14 F M 2014/15 2014/15 Emergency department activity against plan 5000 4500 4000 3500 3000 2500 2000 1500 1000 500 0 A M J J A S 2014/15 actual O N D J F M 2014/15 plan Emergency inpatient FCE activity in month has increased by 4.6% compared with September 2013. This is the first month this financial year where activity has been higher than for the same month last year. Overall there has been a decrease of 8.2% in YTD figures compared to the same period last year. When compared to plan, emergency FCE activity is 4.8% behind plan YTD, but with September activity levels being 7.6% above the planned level. Both Paediatric Surgery (11%) and Orthopedics (28%) are significantly above plan in both month 6 and year to date. In month 6 Paediatrics also shows a large increase. We have previously referred to the reduction in the zero day length of stay patients being admitted from the ED Department and assigned to the A&E specialty as an admission. If these are excluded activity is 4% above last years levels. However in Sep 14 these are higher than in previous months, and this has contributed to the first overall monthly increase vs plan for emergency inpatient activity in 2014/15. Emergency /Non Elective FCEs 2000 1500 1000 500 0 A M J J 2011/12 2000 A S 2012/13 O N D J 2013/14 F M 2014/15 2014/15 Emergency/non elective FCEs activity against plan 1500 1000 500 0 A M J J A 2014/15 actual S O N D J F M 2014/15 plan 13 Planned activity profile. 2014/15 All Elective FCE activity against plan (incl Reg Day Admissions) All elective FCEs 3000 3000 2500 2500 2000 2000 1500 1500 1000 1000 500 500 0 0 A M J 2011/12 J A 2012/13 S O N 2013/14 D J F 2014/15 M A M J J A 2014/15 actual S O N D J F M 2014/15 plan Elective activity in September was 12% higher than in September 2013 and YTD activity also shows a 4.4% increase over 2013/14. Elective activity is now 3.2% above plan YTD, with activity being 9.4% above plan in September 2014. Paediatric Surgery, ENT and Gastroenterology all had high levels of activity in month. In the year to date, combined Haematology/Haemoglobinopathy/Oncology activity is 307 FCEs or 12% above plan with Plastic Surgery 116 FCEs or 12% below plan. Neurology (48%) and Neurosurgery (24%) are significantly over plan with 601 FCEs having been carried out year to date versus a plan of 448. 14 Outpatient activity profile . There is a 13.4% increase for new attendances in September and 11.0% increase for follow up patients when compared with September 2013. New OP attendance 4000 3500 3000 YTD activity shows that new attendances have increased by 0.6% and follow ups YTD have increased by 6.7% when compared to 2013/14. 2500 2000 1500 1000 500 0 A M J J 2011/12 A S O 2012/13 N D J F 2013/14 M 2014/15 Follow up OP attendance 12000 Against plan, all outpatient activity was 10.9% above plan in September 2014 and overall 5.0% ahead of plan YTD. Areas with the biggest absolute growth are T&O, Cardiology, Paediatric Surgery, Respiratory Medicine and ENT. Outpatient procedures performed in September are 34.4% higher than for September 13 and 39.6% higher YTD than in 2013/14. In terms of HRGs this relates to minor Ear Procedures, minor dental procedures and Electrocardiograms 10000 8000 6000 4000 2000 Outpatient Procedures 1400 1200 1000 800 600 400 200 0 A M J 2011/12 J A S 2012/13 O N D J F M 2013/14 2014/15 2014/15 outpatient activity against plan (excl AHP CNS and Phone) 16000 14000 12000 10000 8000 6000 4000 2000 0 0 A M 2011/12 J J A 2012/13 S O N 2013/14 D J F M 2014/15 A M J J A 2014/15 actual S O N D J F M 2014/15 plan 15 4. Efficiency 16 Profitability against Target. The EBITDA (Earnings Before Interest, Taxation, Depreciation and Amortisation) Margin remains below target (5.2% compared with 5.5%). This is a narrowing of the gap experienced in Month 5 (5.1% actual compared with 5.6% plan) with the actual EBITDA margin having improved. In monetary terms EBITDA was also below the YTD Monitor Plan, with a small in-month movement. The coming 2 months will see an increase EBITDA margin requirement as these are historically strong months. EBITDA Margin 8.0% 7.5% 6.8% 7.0% 6.5% 6.0% 6.0% 5.8% 6.2% 5.5% Actual 5.1% 5.2% Plan for Year 5.0% 4.5% 4.0% Apr May Jun The I&E Surplus Margin also continues to be below plan (2.2% compared with 2.4%) which reflects the EBITDA margin. This too is an improved % position and a narrower gap from plan compared with Month 5. As with the EBITDA margin the next 2 months sees an expected increase in the margin. Jul Aug Sep Oct Nov Dec Jan Feb Mar I&E Surplus Margin 5.0% 4.5% 4.0% 3.5% 3.0% 2.5% 2.0% 1.5% 1.0% 0.5% 0.0% 3.9% 2.7% 3.0% 3.2% 2.1% 2.2% Actual Plan for Year Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar 17 Productivity. Income Generated per £1 of Pay Expenditure Two productivity metrics have been produced for the first time in September. These assess the: • Income Generated per £1 of Pay Expenditure; and • Monthly income per wte. With staff costs equating to over two thirds of the Trust’s operating expenditure the return on pay expenditure is vital to the Trust’s productivity and profitability. Cumulative income per £ of pay expenditure is performing ahead of the 2013/14 but remains below plan in 2014/15. The September performance was the nearest performance to plan in the year to date. 1.75 1.70 1.65 £ 1.60 1.55 1.50 Apr The monthly income per wte has, having commenced the year with 4 consecutive months of sub-plan performance, recovered since August and has delivered above plan performance. May Jun Jul Aug Sep Oct Nov #REF! Inc/£1 Pay In-Month 2014/15 Inc/£1 Pay - Cumulative 2014/15 Inc/£1 Pay - Cumulative Plan 2014/15 Dec Jan Feb Mar Inc/£1 Pay - Cumulative 2013/14 Monthly Income per wte since April 2013 85 83 81 79 77 £ 75 73 71 69 67 65 Income per wte - actual Income per wte - plan 18 CIP. This is the CIP position at the halfway point of the year. The overall target reflects the following: • Directorate targets; • Trust-wide scheme targets; and • Residual balance of the underlying legacy position from 2013/14. Headlines from Month 6 are as follows: • Overall schemes identified exceed the annual target – this is an improved position compared to 2013/14; • The majority of schemes have been risk assessed within Directorates; • Quality Impact Assessments are behind schedule but with the PMO’s involvement increasing this will improve in future months; • Corporate and CSS are the areas furthest from target for overall schemes; • The September performance in Surgery has deteriorated due to a revision of previous periods’ savings; • The shortfall on the trust-wide schemes is within Contract Penalties (where pressures are evident for Diagnostics, 18 weeks and CQUIN), Drugs (although this has improved in September) and Future Fit where workforce savings are not materialising in line with the plan; • Phasing throughout the year remains back-ended. CIP Information provided for the first time this month includes: • Forecast actual position in monetary and % terms; and • The level of recurrent plans (per recent KPMG audit recommendation). Directorate Annual Target CAMHS Corporate CSS Medicine SSD Surgery Trustwide Totals £389,526 £723,251 £666,136 £1,324,237 £1,390,984 £725,583 £4,240,000 £9,459,716 Identified Plans £388,640 £568,985 £633,716 £1,533,625 £1,420,330 £740,282 £4,240,000 £9,525,578 YTD Plan YTD Actual £194,311 £256,434 £250,312 £763,733 £709,009 £257,647 £1,181,000 £3,612,446 £190,546 £161,979 £342,519 £680,126 £540,234 £141,502 £864,489 £2,921,396 YTD Variance % Plan To Date % Annual Target -£3,765 -£94,455 £92,207 -£83,607 -£168,775 -£116,145 -£316,511 -£691,050 98% 63% 137% 89% 76% 55% 73% 81% 49% 22% 51% 51% 39% 20% 20% 31% Forecast Actual £ £343,454 £371,164 £574,645 £1,356,624 £997,900 £291,668 £3,225,000 £7,160,455 Forecast Actual % 88% 51% 86% 102% 72% 40% 76% 76% Recurrent Plans £350,050 £359,726 £451,101 £992,784 £937,792 £220,938 £3,110,000 £6,422,392 19 5. Liquidity 20 Cash and Capital. The Capital performance in September was £1.6m behind plan. The forecast spend for the year is £12.8m. However, scheme delivery in a number of areas is behind plan with catch-up unlikely to be until Quarter 4. Key categories of deficit at Month 6 are: • Estates (£0.3m); • Parkview Development (£0.3m); • Medical Equipment (£0.7m); and Patient Experience (£0.1m). • Further detail on this is included as Appendix Five. Mar-16 Jan-16 Feb-16 Dec-15 Oct-15 Nov-15 Sep-15 Jul-15 Aug-15 Jun-15 Apr-15 2014/15 Plan May-15 Mar-15 Jan-15 Feb-15 Dec-14 Oct-14 Actual Nov-14 Sep-14 Jul-14 Aug-14 Jun-14 The cash position is included within the Balance Sheet which is included as Appendix Four. Apr-14 The graphical analysis includes a cash forecast through to March 2016. This period sees a reduced cash balance as the Parkview development continues along with the first year of the clinical block. 55,000 50,000 45,000 40,000 35,000 30,000 £k 25,000 20,000 15,000 10,000 5,000 0 May-14 The Trust’s Liquidity remains significantly above the Continuity of Service threshold of 4. 2014/15 Cash Position and Rolling Forecast Mar-14 Cash is now 3.7% above plan at Month 6. This equates to £1.8m and is primarily a result of reduced capex (see below). Rolling Forecast 2014/15 Cumulative and Forecast Capital Expenditure against Plan and Monitor Margins 16,000 14,000 12,000 10,000 £k 8,000 6,000 4,000 2,000 Apr May 14/15 Actual Jun Jul 14/15 Forecast Aug Sep 14/15 85% Oct Nov 14/15 115% Dec Jan Feb Mar 14/15 Plan - Original 21 6. Workforce 22 Workforce Report Summary September 2014 Sickness Summary – In month sickness is 3.06%, which is lower than this time last year and in line with our 3% target. Long term sickness (%) has decreased to 1.58%, these staff are being supported through our processes. Short term sickness has increased slightly between July and August 2014 and is at 1.48%. The top 3 reasons for sickness during August are), Anxiety/Stress (608.89 WTE days lost) Musculoskeletal (526.71 WTE days lost and Gastrointestinal (319.91 WTE days lost). We will be launching our new staff confidential support service in early November which provides staff and manager support in the managing of stress related sickness. Bank/Agency Usage – There has been an decrease of 16.23WTE during September 2014 to 178.13 WTE, compared to August. Admin usage has decreased to 84.22 WTE and it continues to be high in the Medical Secretary profession (13.94 WTE) and also in Health Records (12.90 WTE). Top 3 Clinical departments using bank are: •PICU (16.98 WTE) – due to overall increase in acuity and gaps in establishment. Job advertised during September – 6 (4.80WTE) 4 New posts and 2 replacements. •Theatres (9.67 WTE) – Due to double running costs due to new staff who are supernumerary on rotation and vacancies filled but not yet in post. No recruitment activity during September. • Ward 7 (7.44 WTE) – Increased bank usage due to 2 long term patients needing 1:1 care, until new staff have started bank cover is needed. No recruitment activity during August. PDR Summary - PDR % has seen an increase this months and is now at 82%. Directorates are continuing to identifying hotspot areas, sending out email reminders to managers and supplying their DMT’s with monthly figures. Turnover Summary -12 month Turnover % for the Trust has decreased slightly for the 12 month period ending September 2014 but remains above the Trust KPI (9%) at 11.10%. All Directorates with the exception of Clinical Support and Surgical have a 12 month turnover % above the Trust 9% KPI target. The main reasons for leaving during September are voluntary resignation due to Relocation (10.80 WTE), to undertake further education (4.76 WTE) and due to work life balance (2.80 WTE). 23 Workforce Dashboard Trust Target CSS Medical Specialised Surgical CAMHS Corporate Trust (Previous Month) Trust (Current Month) Sickness % (YTD) <3.00% 3.18% 4.46% 3.32% 3.13% 2.84% 3.16% 3.44% 3.44% ▬ Sickness % (Month) <3.00% 2.22% 3.44% 2.73% 3.24% 3.20% 3.66% 2.98% 3.06% ▲ Indicator Trend 79 102 110 61 34 75 451 461 ▲ LT Sickness % 0.70% 2.18% 1.42% 1.71% 1.25% 1.99% 1.73% 1.58% ▼ ST Sickness % 1.52% 1.26% 1.31% 1.53% 1.96% 1.67% 1.25% 1.48% ▲ £27,828.51 £57,851.37 £41,856.94 £29,503.89 £19,014.22 £39,929.77 £214,023.55 £215,984.70 £168,755.55 £32,775.92 £198,350.36 £155,715.28 £91,513.43 £186,633.41 £912,739.25 £1,128,723.95 346.37 702.26 645.43 437.58 281.93 601.72 2922.90 3015.29 ▲ 86.34% 84.26% 86.31% 83.69% 78.07% 71.37% 82.34% 82.00% ▼ Starters FTE 12.15 26.28 19.00 12.60 2.41 29.55 90.21 101.99 ▲ Leavers FTE 8.33 27.94 14.91 11.25 2.50 5.93 91.16 70.86 ▼ 8.74% 11.68% 11.45% 9.88% 13.11% 12.16% 11.64% 11.10% ▼ ▼ Episodes Cost of sickness Cost of sickness YTD FTE days lost sickness PDR's % Rolling Turnover % 90% <9% In Month Turnover % Headcount WTE in post 1.53% 1.00% 0.60% 1.00% 0.61% 0.70% 1.07% 0.91% 574 511.07 725 658.74 841 770.29 474 436.01 316 284.93 610 561.11 3509 3194.47 3540 3222.15 Active Recruitment 7 7 12 4 3 10 72 43 ▼ 5.20 42.92 43.64 28.93 4.22 53.22 194.36 178.13 ▼ 3.58% 5.11% 4.63% 5.05% 4.00% 1.89% 3.92% 4.09% ▲ 4 14 12 5 40 45 ▲ 0 1 n/a Bank Usage Maternity Leave % Staff in Difficulty 6 4 Org Change Please note that sickness is still one month behind so we are currently reporting on Augusts data Current months WTE may be slightly lower due to new starters from the 2nd induction still being inputted onto ESR. Employee Relations - On going or started during reporting month Consultant Appraisals % is now a rolling 12 month figure Turnover % is based on permanent staff leavers only 0 1 0 0 0 0 24 Sickness Absence BCH Monthly Sickness % Long and Short Term Sickness % 4.00% 3.50% 3.00% 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 2.50% 2.00% 1.50% 1.00% 0.50% 0.00% 0.70% 1.58% 14/15 1.71% 1.31% 1.53% 284 Dir 3 Specialised Services 284 Dir 4 Surgical Directorate 1.25% 1.52% 1.48% BCH Trust Sickness 13/14 1.42% 2.18% 1.26% 284 Dir 1 Clinical Support Services 284 Dir 2 Medical Directorate Short Term Sickness Trust Target 1.99% 1.96% 284 Dir 5 CAMHS Services 1.67% 284 Dir 6 Corporate Long Term Sickness BCH Sickness Comparison 13/14 April May June July August September October November December January February March 2.85% 3.13% 3.39% 3.58% 3.22% 3.36% 3.74% 3.65% 3.43% 3.73% 3.76% 3.69% 3.67% 3.23% 2.98% 2.98% 3.06% Number of Episodes Monthly Sickness % Cumulative 12 Month Sickness % 461 3.06% 3.44% 79 2.22% 3.18% 102 3.44% 4.46% 110 2.73% 3.32% 61 3.24% 3.13% 34 3.20% 2.84% 75 3.63% 3.16% 14/15 BCH Sickness Absence - August 2014 BCH Total Clinical Support Services Medical Directorate Specialised Services Surgical Directorate CAMHS Services Corporate Sickness remains steady at 3.44%, this is due to a number of long term sickness cases, this will further reduce as there are two stage 3 meetings to be held. Anxiety/stress/depression still remains the main reason for sickness but this is due to one long term case due to an employee relation case. Challenge and confirm meetings are held on a quarterly basis and a number of audits in hot spot areas have been undertaken by the HR Compliance Manager. This has reduced from last month’s figures; this is shared evenly over long and short term episodes. The hot spot areas are Neonatal Surgical Ward and Wards 9 and 10, again with a number of gastrointestinal problems. Support and Challenge meetings have been arranged for the directorate with hotspot as a priority. Two long term sickness cases, one due to family bereavement. There are a number of short term sickness cases and majority are due to gastrointestinal problems. HR Advisor attends the ward managers meeting at Parkview on a monthly basis and sickness percentages are discussed at the Senior Management Team Meeting monthly. 25 Bank/Agency Usage Apr 14 May 14 June 14 July 14 Aug 14 Sept 14 CSS 4.66 6.01 6.50 7.22 5.96 5.20 Medical 39.14 42.61 53.40 49.18 49.53 42.92 Specialised 44.95 47.57 44.09 44.79 42.32 43.64 250 Surgical 26.57 26.80 22.32 35.96 32.41 28.93 200 CAMHS 9.07 8.65 10.21 7.87 14.69 4.22 Corporate 46.05 44.09 48.10 53.98 49.45 53.22 Total 170.44 175.73 184.63 199.00 194.36 178.13 Trust Bank/Agency Usage (WTE) Yearly Comparison 214.52 178.13 WTE 150 100 2013/14 2014/15 50 * The latest month is an indicative figure and about 95% accurate. The previous month figure will be updated each month 0 Top 3 reasons for Bank/Agency usage 1. Vacancy – 125.94 WTE 2. Sickness – 21.91 WTE 3. Specialist Skills Required – 8.73 WTE Admin bank and agency usage = 84.22 WTE. Bank/Agency Usage September 2014 Top 3 reasons for Admin usage are Vacancy, Backlog and Teaching/Training. Directorate Admin bank and agency is as follows: 1.06 CSS - 2.26 WTE - Labs, Diabetes and Surgical Day Care 37.25 Priority 7 47.28 Medical – 6.14 WTE - Primarily Medical Secretary Areas (4.94 WTE) Specialised – 6.16 WTE – Cardiac Service, PICU and Liver Surgical - 18.49 WTE - Primarily Medical Secretary Areas (9.00 WTE) 14.41 A&C Non Reg CAMHS – 3.71 WTE - East Locality and Tertiary Psychology Reg Medical Corporate – 47.46 WTE – Health Records (12.90), Finance (5.23) and Patient Access Call Centre (4.34) 26 PDR - AFC Staff CSS The Directorate continues to focus on PDRs. Completion rates are regularly discussed at the weekly Directorate Executive Team meetings and departmental managers discuss their plans for adhering to the Trust’s PDR completion target at their regular business meetings which HR now attends. A monthly workforce report, including PDRs, is now produced for the Directorate and this is discussed in detail at a weekly Directorate Management Team meeting. Medical The medical directorate has prioritised this area as an area of focus. Each service has presented their plans to ensure all outstanding staff have a completed PDR before the end of September. It is projected the directorate will meet the 90% target at latest, the end of October. Any areas that have not made progress by the end of September, will receive support to facilitate the proposed achievement. Priority 3 Apr May June July August Sept BCH 82.93% 82.58% 83.58% 83.31% 82.34% 82.00% Clinical Support Services 88.81% 84.74% 88.08% 89.49% 85.58% 86.34% Medical Directorate 83.77% 82.97% 86.34% 82.97% 83.08% 84.26% Specialised Services 83.66% 85.38% 86.54% 86.62% 88.00% 86.31% Surgical Directorate 86.60% 87.24% 84.78% 85.42% 83.62% 83.69% CAMHS Services 86.40% 84.42% 76.52% 74.79% 71.00% 78.07% 71.68% 72.41% 75.51% 76.55% 78.56% 71.37% Corporate Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Add Prof Scientific & Technical 88.60% 85.57% 83.59% 86.04% 79.03% 87.66% Additional Clinical Services 83.50% 76.50% 81.68% 85.85% 85.26% 85.06% Estates & Anciliary 79.71% 77.66% 76.97% 88.29% 82.30% 84.87% 77.69% 80.00% 89.23% 76.75% 88.24% 84.50% 76.11% 82.79% 85.82% 72.98% 84.80% 83.94% Healthcare Scientists 77.24% 78.05% 83.87% 90.32% 88.71% 88.33% Nursing 83.45% 83.33% 85.04% 84.45% 84.73% 84.78% Table 1 Admin & Clerical AHP's Table 1 shows via staff group the Appraisal compliance. Compared to last months data all staff groups with the exception of Admin and Estates have seen an increase in their PDR. Admin & Clerical now have a % less than 75%. Specialised Specialised are the only directorate to have seen an increase in their PDR % this month. Theatres PDR rate is now at 92% and PICU 91%. PICU has been working to improve their PDR rates by introducing the following: • With the introduction of PICU now working in three staff teams, the band 7 leaders have more responsibility for their teams and their development . • In the local PICU band 6 leadership days they have introduced a session on importance of appraisals. • Senior band 5 staff are now developing skills to support/undertake PDR’s for a specified group of staff Corporate HR will continue to email Corporate HODs and copying in chief officers requesting that appraisals are undertaken. Letters have recently been sent out from the Director of Workforce requesting recovery plans. CAMHS The CAMHS SLT have discussed this % during their meeting in August. The action from the meeting was that managers will be emailed about their PDR and mandatory training % and new PDR dates will be emailed to the directorate PA so that ESR can be updated. The CAHMS % should see an increase over the coming months. The directorate will be undertaking a forward look approach to ensure dates are scheduled for PDR’s until end of March 2015. Surgical PDR rates for the Surgical directorate have been at 83% for the last 3 months; there are 3 key areas within the directorate where rates are low, one of the main reasons is the spikes in sickness absence and extra support is being given to these areas. There is a directorate focus to improve the PDR rates using the following tools: Monthly HR PDR reports sent to the departments, introduction of confirm and challenge sessions, review by DMT Managers of PDR data inputting. The wards discuss PDR;s rates at weekly band 7 meetings, and in August one of the wards reached 97% PDR compliance. 27 Staff in Difficulty Staff in Difficulty Cases (January 14 to September 14) 70 Number of Cases 60 61 53 54 50 40 37 35 52 40 38 44 30 20 10 0 January February March April May June July August Sept Breakdown of Cases September 14 A large proportion of the staff in difficulty cases continue to be due to conduct and performance issues. Managers are becoming more effective at dealing with inappropriate behaviour and measuring against the Trust values. 44 Cases 31% 40% Disciplinary Grievance Managers are identifying and managing staff in difficulty more effectively. This is supported by bespoke development in managing performance. Harassment Performance 22% 7% 28 BCH Nursing Staffing: • • Physical Environment: September saw the reopening of Ward 9 after the refurbishment in time for the predicted increase in surgical activity. Ward 15 managed the scheduled closure of HDU bed spaces. • Staffing: Traditionally September is traditionally a low point in head count for Registered Nurses working for the trust as we await the autumn NQN cohort to start. This year we have experience an increase in retention. These combined that we expect to be in a strong position by the year end. In the next two months it will remain challenging as we both continue to deliver our activity levels whilst supporting and training the new intake. The second cohort of CSW Development Trainees commenced in Sept whilst the successful candidates in cohort one have been placed into positions. • Temporary Staffing: We have seen a correlating reduction in nurse bank expenditure linked to the reduction in activity levels. • No Red shifts were recorded for the second month in a row as the enclosed national data set demonstrates. Nursing Workforce Summary Monthly Ave: Jul-14 Aug-14 Sept-14 Act vs. Plan Acuity Skill Mix Vacancy Annual Leave Mat Leave Sickness Bank 100.9% 95.5% 102.95 91.9% 97.1% 92.05 79.6% 79.9% 79.7% 3.5% 4.7% 4.8% 16.9% 18.8% 14.4% 7.3% 7.9% 8.1% 4.6% 4.5% 4.0% 7.7% 8.7% 8.1% 29 Nursing Workforce September 2014 Nursing Workforce Dashboard: Ward79.13 Nursing Staffing Actual vs Planned Patient Acuity Level Registered Care Staff Registered Care Staff Day Day Night Night Burns Actual vs Planned % 138.6% Actual vs Planned % 121.4% Actual vs Planned % 137.7% Actual vs Planned % 81.8% Actual vs Planned % 132.4% Neonatal Surgical 134.2% 121.2% 131.3% 133.3% 131.5% Sept-14 Total Planned Resources Unplanned: Actual & Response No of Times Raised to HoN No of Green shifts No of Amber shifts No of Red shifts 88 2 0 81.5 10.9 0.84 11.1 7.6 1.6 52.8 2.2% 0 85 5 0 77.6 7.3 -0.41 10.8 9 3.3 72.4 5.6% 0 0 Unfilled Registered Vacanc Leave Mat Roster Skill Mix% y WTE % Leave % % Sicknes Bank Fill Bank s % Used Ward 1 95.7% 90.2% 98.8% N/A 96.1% 73 17 0 81.5 2.7 -1.6 17.1 11.4 1.6 71.2 9.0% Ward 5 100.5% 140.0% 101.7% 92.6% 107.1% 73 17 0 74.3 14.1 2.6 13.8 9.1 0.9 58.5 9.4% 0 Ward 9 102.3% 100.3% 103.6% 110.7% 103.2% 86 4 0 78.4 12.4 -1 16.5 8 1.2 66.3 8.8% 0 Ward 10 98.1% 91.5% 100.9% 103.2% 98.5% 88 2 0 77.2 3.3 -1.3 12.4 11.7 3.9 81.8 3.2% 0 ED 104.2% 99.4% 95.3% 100.0% 99.8% 80 10 0 78.5 7.9 9.8 20.7 4.5 7.2 81.5 17.5% 0 PAU 95.7% 103.3% 101.8% 95.6% 98.6% 87 3 0 83.4 9.3 -1.7 16.9 9.4 5.4 58.7 9.0% 0 Ward 2 90.1% 92.5% 96.3% 92.3% 92.7% 75 15 0 84.3 8.9 1.8 17.6 15.4 7.1 75.9 23.1% 0 Ward 7 98.2% 105.4% 96.5% 108.0% 99.8% 87 3 0 77.3 5.8 -4.2 13.2 3.9 1.4 77.9 18.4% 0 MHDU 103.5% N/A 105.8% N/A 104.6% 86 4 0 100 3.4 -3 11.8 9 0.8 23.1 1.3% 0 Ward 15 100.8% 99.5% 107.9% 133.3% 103.7% 79 10 0 84.1 23.5 6.6 18.7 5.9 5.5 41.7 10.5% 0 ODC* 103.2% 86.9% N/A N/A 97.8% 44 0 0 74.6 10.8 -1.62 7.7 17.2 1.2 63.9 13.5% 0 Ward 8 102.2% 86.9% 100.8% 150.6% 104.1% 81 9 0 85.9 14 0.8 11.4 18.4 4.2 74.0 2.5% 0 Ward 11 98.7% 104.7% 102.3% 111.1% 100.7% 83 7 0 92.6 6.8 -1 14.5 2.1 5.5 59.4 7.5% 0 Ward 12 103.4% 123.1% 101.8% 150.0% 105.5% 82 8 0 83.8 8.4 1.2 17.8 4.9 5.3 68.5 2.3% PICU 96.1% 86.7% 95.6% 106.5% 95.9% 80 10 0 90.2 45.9 45.71 13.7 6.1 4.8 0 0 0 MDC* 159.0% 136.5% N/A N/A 156.0% 44 0 0 87.8 21.1 -0.3 14.8 4.8 3.1 SDC* 125.3% 110.5% N/A N/A 121.45 44 0 0 74.3 28.9 -6.6 15.6 4 6.0 Ashfield 109.7% 94.2% 94.8% 91.4% 99.4% 90 0 0 68.0 20.1 -1.6 16.2 5.7 1.5 52.5 1.0% 0 Heathlands 92.8% 97.3% 111.9% 155.5% 104.4% 74 16 0 36.0 -7 15.8 6.5 7.5 18.8 1.2% 0 97.8% 103.6% 114.3% 119.0% 106.3% 88 2 0 58.1 60.7 30.0 5.1 9.5 4.2 8.1 102.8% 102.5% 101.4% 110.3% 102.7% 1697 144 0 79.73 15.1 2.0 14.4 8.1 4 Irwin Trust Average: 0 93.9 62.8 8.3% 8.1 0 0 •Excluded from National Upload 30 Nursing, Midwifery and Care Staff Staffing September 2014 Submission to NHS England Main 2 Specialties on each ward Registered midwives/nurses Ward name Specialty 1 Burns Neonatal Surgical Ward 1 Ward 5 Ward 9 Ward 10 ED PAU Ward 2 Ward 7 MHDU Ward 15 Ward 8 Ward 11 Ward 12 PICU Ashfield Heathlands Irwin 171 - PAEDIATRIC SURGERY 171 - PAEDIATRIC SURGERY 171 - PAEDIATRIC SURGERY 171 - PAEDIATRIC SURGERY 171 - PAEDIATRIC SURGERY 171 - PAEDIATRIC SURGERY 420 PAEDIATRICS 420 PAEDIATRICS 420 PAEDIATRICS 420 PAEDIATRICS 420 PAEDIATRICS 420 PAEDIATRICS 420 PAEDIATRICS Specialty 2 160 - PLASTIC SURGERY 171 - PAEDIATRIC SURGERY 361 NEPHROLOGY 100 - GENERAL SURGERY 100 - GENERAL SURGERY 150 NEUROSURGERY 180 - ACCIDENT & EMERGENCY 300 - GENERAL MEDICINE 300 - GENERAL MEDICINE 300 - GENERAL MEDICINE 192 - CRITICAL CARE MEDICINE 303 - CLINICAL HAEMATOLOGY 171 - PAEDIATRIC SURGERY 170 321 - PAEDIATRIC CARDIOTHORACIC CARDIOLOGY SURGERY 170 321 - PAEDIATRIC CARDIOTHORACIC CARDIOLOGY SURGERY 420 192 - CRITICAL PAEDIATRICS CARE MEDICINE 711- CHILD and 711- CHILD and ADOLESCENT ADOLESCENT PSYCHIATRY PSYCHIATRY 711- CHILD and 711- CHILD and ADOLESCENT ADOLESCENT PSYCHIATRY PSYCHIATRY 711- CHILD and 711- CHILD and ADOLESCENT ADOLESCENT PSYCHIATRY PSYCHIATRY Total monthly planned staff hours Total monthly actual staff hours Registered midwives/nurses Care Staff Care Staff Average fill Average fill rate Average fill rate Average fill registered rate - care registered rate - care Total Total Total Total Total Total nurses/midwi staff (%) nurses/midwi staff (%) monthly monthly monthly monthly monthly monthly ves (%) ves (%) planned actual staff planned actual staff planned actual staff staff hours hours staff hours hours staff hours hours 975 1352 319 387 671 924 121 99 1352 1814 384 465 1056 1386 396 528 1151 1100 402 363 1034 1022 0 0 1580 1587 657 919 1265 1287 297 275 1872 1916 475 476 1210 1254 308 341 1833 1799 572 524 1199 1210 341 352 2353 2451 936 931 2244 2138 330 330 1781 1705 423 437 1210 1232 286 274 2002 1803 533 493 1485 1430 429 396 1417 1391 780 822 1254 1210 275 297 1138 1178 0 0 946 1001 0 0 2945 2967 1053 1048 2365 2552 99 132 1885 1926 286 249 1309 1319 275 414 2054 2027 182 191 1452 1485 99 110 1866 1930 351 432 1199 1221 44 66 11876 11407 566 491 9889 9456 506 539 1313 1441 780 735 1182 1121 495 453 988 917 819 797 671 751 242 376 852 833 624 647 561 641 352 419 138.6% 121.4% 137.7% 81.8% 134.2% 121.2% 131.3% 133.3% 95.7% 90.2% 98.8% - 100.5% 140.0% 101.7% 92.6% 102.3% 100.3% 103.6% 110.7% 98.1% 91.5% 100.9% 103.2% 104.2% 99.4% 95.3% 100.0% 95.7% 103.3% 101.8% 95.6% 90.1% 92.5% 96.3% 92.3% 98.2% 105.4% 96.5% 108.0% 103.5% - 105.8% - 100.8% 99.5% 107.9% 133.3% 102.2% 86.9% 100.8% 150.6% 98.7% 104.7% 102.3% 111.1% 103.4% 123.1% 101.8% 150.0% 96.1% 86.7% 95.6% 106.5% 109.7% 94.2% 94.8% 91.4% 92.8% 97.3% 111.9% 155.5% 97.8% 103.6% 114.3% 119.0% 31 Mandatory Training Update Mandatory training compliance at BCH is currently averaging at 80.36% (Vesper: 7/10/14) representing 0.18% decrease since last month. Table 1 below shows the Trust Level Breakdown as at 7th October 2014 and the trajectory since Mar 2014. In terms of capacity and mandatory training updates, the amount of face to face places planned for 2014 has been over and above requirements however as reported previously, there is low engagement with staff. Please see Table 2 for further information. Despite 66% of training now being available on Moodle and numbers increasing month on month through Moodle training, it is not resulting in a positive trajectory at present. A more detailed review of the mandatory training data across the Trust suggests there are key staff groups that are impacting heavily on compliance. The Admin and Clerical group have now moved up the table sitting second only to Nursing and Midwifery which is disappointing as this staff group can update all mandatory training topics online. See Table 3 for information. Plan to Improve To improve compliance we have implemented a number of improvements including reminder emails, processes for data query handling and register tracking and audit to ensure data is entered in a timely manner. Data queries do exist however, not in sufficient numbers to impact significantly on the downward trend displayed in Table 1. The targeted approach for Child Protection L2 back in June 2014 saw a significant increase with compliance reaching circa 89%. This approach along with great support from managers enabled this to be achieved so we will be completing a more detailed analysis of data to deliver this targeted approach to weaker areas and groups. This will form part of the wider recovery plan. Table 1 Table 2 Table 3 32 BIRMINGHAM CHILDREN'S HOSPITAL NHS FOUNDATION TRUST Income and Expenditure Summary (Working Document) For the Period Ended: 30/09/2013 Annual Plan to Monitor £'000 Appendix One Revised Annual Plan £'000 In Month Budget £'000 In Month Actual £'000 In Month Variance £'000 YTD Plan to Monitor £'000 Revised YTD Budget £'000 Year To Date Actual £'000 Year To Date Variance £'000 Income NHS Clinical Income Elective Inpatients Elective Day Cases Non-Elective Outpatients ED Other Royal Orthopaedic Total NHS Clinical Income 25,894 16,964 33,478 23,029 4,843 113,102 475 217,785 25,685 16,705 32,831 22,281 4,868 114,461 475 217,306 2,125 1,382 2,651 1,837 390 9,808 40 18,233 2,115 1,426 2,717 1,914 408 10,060 40 18,680 (10) 44 66 76 18 252 0 447 13,257 8,685 17,023 11,576 2,429 56,789 0 109,759 12,750 8,291 15,908 11,024 2,340 59,104 238 109,655 12,691 8,555 16,305 11,482 2,448 57,431 238 109,150 (60) 264 397 458 108 (1,672) 0 (505) 211 211 211 211 18 18 110 110 92 92 106 106 105 105 369 369 263 263 7,038 2,300 (2,081) 2,546 1,696 1,843 1,021 1,049 4,254 0 0 19,666 7,038 2,300 0 2,938 1,951 1,944 735 1,310 4,733 0 0 22,949 587 230 0 464 162 206 66 101 315 0 0 2,131 304 (7) 0 510 150 199 76 113 603 0 0 1,947 (283) (237) 0 46 (12) (7) 10 11 287 0 0 (184) 3,519 1,150 (1,041) 1,273 848 922 510 525 2,127 0 (230) 9,603 3,519 920 0 1,572 978 1,168 373 694 2,346 0 0 11,570 3,238 683 0 1,775 923 1,049 407 673 3,180 0 0 11,927 (282) (237) 0 203 (55) (119) 33 (21) 833 0 0 356 237,663 240,466 20,381 20,737 356 119,468 121,331 121,445 114 Pay Clinical Support Services Directorate Medical Directorate Directorate of Specialised Services Surgical Directorate CAMHs Corporate Pay Inflation Reserve Other Pay Reserves Phasing Adjustment Total Pay 20,381 31,397 40,377 22,854 14,605 19,154 4,158 0 0 152,926 21,075 32,892 40,500 23,162 14,152 20,329 0 1,723 0 153,833 1,832 2,728 3,356 2,116 1,172 1,599 0 0 0 12,803 1,802 2,845 3,378 2,041 1,171 1,682 0 0 0 12,920 30 (117) (22) 74 1 (83) 0 0 0 (117) 10,191 15,699 20,189 11,427 7,302 9,577 2,079 0 (2,331) 74,132 10,472 16,400 20,131 11,851 7,112 9,938 0 (8) 0 75,896 10,536 16,681 20,351 12,297 6,941 10,124 0 0 0 76,930 (64) (281) (220) (445) 171 (186) 0 (8) 0 (1,034) Non-Pay Clinical Support Services Directorate Medical Directorate Directorate of Specialised Services Surgical Directorate CAMHs Corporate Leases Non-Pay Reserves and Developments Bad Debts Total Non-Pay 7,892 19,781 12,760 5,628 1,365 13,586 244 11,659 0 72,915 9,230 21,346 12,624 5,950 1,674 16,785 218 7,025 0 74,851 1,199 1,768 958 592 135 1,377 20 252 0 6,301 1,253 1,750 1,242 620 154 1,622 5 0 0 6,646 (54) 18 (284) (27) (19) (245) 15 251 0 (346) 3,946 9,891 6,380 2,814 683 6,793 122 8,161 0 38,789 5,621 10,997 5,932 3,176 833 8,525 98 3,693 0 38,874 5,807 11,073 7,419 3,276 897 9,493 221 (1) 0 38,184 (186) (76) (1,488) (100) (64) (968) (123) 3,694 0 689 225,841 228,684 19,104 19,566 (462) 112,921 114,770 115,114 (345) 11,822 Non NHS Clinical Income Road Traffic Act (RTA) Income Total Non NHS Clinical Income Other Income Teaching and Research Donated Assets Other Central Income Clinical Support Services Directorate Medical Directorate Directorate of Specialised Services Surgical Directorate CAMHs Corporate Other Income Reserves Other Total Other Income Total Income Central income only Operational Expenditure Total Operational Expenditure EBITDA 11,782 1,277 1,171 (107) 6,547 0 4,624 2,762 (243) 300 4,559 2,762 (247) 326 0 380 230 (21) 27 0 376 211 (15) 23 0 4 19 (6) 4 0 2,312 1,381 (122) 150 6,561 5.4% 0 2,280 1,381 (124) 163 6,331 5.2% 0 2,302 1,263 (86) 141 (230) Loss on Disposal of Fixed Assets Depreciation Dividends on PDC Interest Receivable Interest Payable Retained Surplus/(Deficit) For Period 4,379 4,382 661 575 (85) 2,825 2,861 2,711 (151) 0 (22) 118 (38) 22 Appendix Two Analysis of Expenditure by Cost Category Plan Actual Variance Variance £m £m £m % YTD YTD YTD YTD YTD YTD 3.82 16.21 8.09 27.89 9.27 10.40 3.64 15.55 7.85 26.59 9.52 9.88 -0.18 -0.66 -0.25 -1.30 0.24 -0.53 -4.7% -4.1% -3.0% -4.7% 2.6% -5.1% YTD YTD YTD YTD YTD YTD 0.00 0.03 0.04 0.07 0.05 0.02 75.90 0.00 0.80 0.36 2.07 0.55 0.12 76.93 0.00 0.77 0.32 2.00 0.51 0.10 1.03 1.4% Total Non-Pay 13.84 10.18 14.86 38.87 14.19 10.96 13.04 38.18 0.35 0.77 -1.82 -0.69 2.6% 7.6% -12.2% -1.8% Total Operating Expenses 114.77 115.11 0.34 0.3% 2.28 1.38 0.16 2.30 1.26 0.14 0.02 -0.12 -0.02 1.0% -8.5% -13.7% 118.59 118.82 0.23 0.2% Pay Substantive Staffing Senior Management (including Board) Medical Consultants Other Medical Staffing Nursing Admin, Maintenance and Support Workers Professional/Technical and AHPs Bank, Agency and Locum Staffing Senior Management (including Board) Medical Consultants Other Medical Staffing Nursing Admin, Maintenance and Support Workers Professional/Technical and AHPs Total Pay Non Pay Below the Line Drugs Clinical Supplies Other Operating Expenses Depreciation and Amortisation PDC Dividend Expense Interest Expense on PFI Total Expenditure YTD YTD YTD YTD YTD YTD Appendix Three Trust-Wide Forecasts 2014/15 Forecast Income from activities Elective Inpatients Elective Day Cases Non-Elective Outpatients ED Other ROH Total Income from Activities Other Income Operating Expenses EBITDA Interest Receivable Depreciation Profit/(Loss) on Asset Disposal Impairment PDC Dividend Interest Paid Net Surplus/(Deficit) Trust-Wide Forecasts Directorate summary: Clinical Support Services Medicine Specialised Services CAMHS Surgery Corporate R&D Total Annual Plan per Monitor £'000 Revised Annual Plan £'000 Year-End Forecast Variance £'000 £'000 25,894 16,964 33,478 23,029 4,843 113,102 475 217,785 19,877 -225,841 11,822 243 -4,624 0 0 -2,762 -300 4,379 25,685 16,705 32,831 22,281 4,868 114,461 475 217,306 23,160 -228,684 11,782 247 -4,559 0 0 -2,762 -326 4,382 26,135 17,237 33,688 23,211 5,093 112,746 475 218,585 24,968 -231,392 12,162 247 -4,559 0 0 -2,762 -326 4,761 450 532 857 930 225 -1,715 0 1,279 1,808 -2,708 380 0 0 0 0 0 0 380 Pay -208 -98 -196 260 -1,655 -62 0 -1,960 Non-Pay 53 -291 -3,627 -79 -213 -1,356 0 -5,515 Income 158 -94 -203 -103 96 1,180 0 1,032 Total 3 -484 -4,026 77 -1,773 -239 0 -6,442 Appendix Four Balance Sheet as at 30th September 2014 30th September 2014 £000 Non-Current Assets PPE - owned PPE - PFI Intangible Assets Non-Current Financial Assets Other Receivables Non-Current Total Non-Current Assets 101,870 1,019 253 550 1,698 105,391 Current Assets Inventories NHS Trade Debtors Non NHS Trade Debtors Debtor re Capital Receipts Provision for irrecoverable debts Prepayments Accrued Income Cash at GBS Cash And Cash Equivalents - non-GBS Total Current Assets 3,659 3,285 3,627 (1,707) 2,880 3,489 50,916 99 66,247 Current Liabilities Deferred Income NHS (Trade) Creditors Non-NHS (Other) Creditors Other creditors Capital Creditor Tax and Social Security Provisions<12 Months PDC Creditors Accruals (5,145) (4,875) (6,107) (2,788) (865) (3,102) (1,370) (11,225) Total Current Liabilities (35,476) Net Current Assets 30,771 Total Assets Less Current Liabilities Accr&Def Incm Non-Current Provisions for Liabilities and Charges PFI Liability Total Assets Employed 136,162 (667) (3,587) (1,676) 130,231 Financed by: Taxpayers' Equity Retained earnings Public Dividend Capital Revaluation Reserve (29,588) (87,723) (12,920) Total Taxpayers Equity (130,231) Appendix Five Capital Programme - Year to Date and Forecast Positions Area Pre-Commitments Including Parkview CT Scanner Gamma Camera Electrical Infrastructure Estates Building IT Medical Equipment Strategic Development Other Patient Experience Facilities Central Function Other Contingency Total BCH Spending Externally funded schemes Respiratory Services Sensory Garden Theatre Project Transnasal navigation system ePMA Cryoconsole FibroScan Total BCH Charity Funded Total Capital Spending Monitor Plan Resubmitted Plan Annual Forecast Forecast Variance YTD Plan YTD Actual % of Scheme Total YTD Variance £000's 5,818 2,098 866 754 800 1,500 360 3,395 1,650 0 848 170 150 300 0 228 13,571 £000's 5,985 2,098 866 754 800 1,501 250 1,406 1,675 0 965 280 150 307 0 228 11,782 £000's 6,317 0 0 0 0 1,461 267 1,533 1,634 0 825 173 148 329 0 176 12,037 £000's 332 (2,098) (866) (754) (800) (41) 17 127 (41) 0 (140) (107) (2) 22 0 (52) 255 £000's 3,118 712 866 0 390 513 40 472 990 0 332 113 60 158 0 0 5,465 £000's 2,551 363 855 0 392 252 0 461 292 0 282 28 16 238 0 0 3,838 £000's 43% 17% 99% 0% 49% 17% 0% 33% 17% #VALUE! 29% 10% 11% 77% n/a 0% 33% £000's 567 349 11 0 (1) 261 40 12 698 0 50 86 44 (80) 0 0 1,627 0 0 0 0 1,469 0 0 1,469 15,040 1 9 0 0 786 0 0 796 12,577 (2) 8 0 24 638 20 100 787 12,824 (4) (0) 0 24 (148) 20 100 (8) 247 #VALUE! 9 0 0 153 0 0 #VALUE! #VALUE! #VALUE! 8 0 24 136 0 0 #VALUE! #VALUE! #VALUE! 97% n/a n/a 17% n/a n/a #VALUE! #VALUE! #VALUE! 0 0 (24) 17 0 0 #VALUE! #VALUE! Item 14.222 Strategic Objectives Applicable Trust Board 30th October 2014 Enc 05 2. Every child and young person requiring access to care at BCH will be admitted in a timely way, with no unnecessary waiting along their pathway. 3. Every member of staff working for BCH will be looking for, and delivering better ways of providing outstanding care, at better value. Report Title Discussion document to inform the September 2014 Finance and Resources Committee: interim review of the Next Generation Patient Pathways Programme Sponsoring Director David Melbourne Authors Phil Foster, Nick Barlow, David Melbourne Previously considered by Original business case to Board of Directors February 2014, following Finance and Resources Committee Purpose A business case was approved by the Board in February 2013 to appoint Newton to support the Trust in this work. Newton have presented to the Finance & Resources Committee on progress (September). This discussion document has been prepared to inform the Board of progress, risks and opportunities to maximise the value delivered by the Next Generation Patient Pathways Programme, specifically the outpatients and surgical flow projects. Appendices: - Introduction to the outpatient and surgery projects from January 2014 - One page project health summaries for outpatients and surgery - Earned value management reports showing activity progress against plan - Benefits tracking – financial opportunity, target and actual by service and project - ‘HEIDI’ examples Background The outpatient and surgical flow projects started in April 2014 as major components of the Next Generation Patient Pathways Programme. The core operational work in surgical flow will be complete by the end of October, with the outpatient project running until the new year. David Melbourne is the executive sponsor, Claire Burden is the operational lead. The combined financial targets for these projects are: - Part year effect for the financial year 14/15 of £960k 1 - Full year target of £1.6m with a stretch of £2.5m assuming a 3.5 hour clinical session, or Full year target of £3.0m with a stretch of £4.0m assuming a 4 hour clinical session Clinical teams are engaging well in both areas and significant operational improvements continue to be made (5% increase in theatre productivity to date, reduced waiting times in main outpatients for example, see below for more highlights). The projects are now progressing towards the benefits realisation phase, where services will make use of the capacity that is being released to turn it into cashable improvements (“dark green dollars” as described by the Health Institute). With this in mind, services currently have firm plans through these projects for: - Part year effect for the financial year 14/15 of between £0.6m and £1.1m - Full year effect of between £1.6m and £2.1m These numbers are closer to the target level than stretch. The ambition is clearly to deliver improvements at the upper end of the range. This document outlines the levers (with supporting information for discussion) to increase the savings levels towards the stretch values. Key Points to Note Operational Highlights - Trust-wide theatre utilisation at record levels in July and August for the last 12 months - With some specialties showing even greater improvement (see Urology graph for example) - Percentage of outpatients who have to wait less than 15 minutes from arrival to being ready to see the clinician is up from one-third to two-thirds Only 1 clinic per month starting late due to delays in the flow through main outpatients Clinic start and end times now being captured for more than 64 clinics/week (and increasing) using the clinic tracking tool. This information is crucial to the complete redesign of all templates. This is the first time this kind of data has been captured in outpatients to drive improvement as a matter of course Service redesign process being run with 27 specialties – capacity & demand modelling complete with 20, service redesign meetings run with 16, workshops run with 9 and agreement of changes with 6 (covering ~90 templates and 50,000 slots p.a.) New slot availability based booking tool trialled for two specialties leading to extra new attendances. Now rolling out across all specialties Launch of the ‘HEIDI’ system (‘Hospital Efficiency Improvements Driven by Information’) – provides transparency of performance and opportunities for improvement by area, team and clinician. Used to drive scheduling processes across surgery and outpatients - - - - 2 Financial Overview The table below presents the current financial overview of the programme. The row labelled ‘current plans’ represents the improvements which services have firm, declared plans for in relation to these projects. FY14/15 Target Full Year Effect Surgery £700k-1.3m for 3.5hr sessions £1.6-2.3m for 4hr sessions Outpatients £900k-1.2m for 3.5hr sessions £1.4-1.7m for 4hr sessions Total £1.6-2.5m for 3.5hr sessions £3.0-4.0m for 4hr sessions £960k £0.7m - £1.0m (would jump up if session length change can be agreed) Surgery Current plans Outpatients Total £0.9m - £1.1m £579k - 1.1m £1.6m - 2.1m and climbing Governance Structure The projects report to the Next Generation Programme Board (TLT) through the following structure: Monthly to coordinate and drive the programme, escalate risks & opportunities Chair: Sarah-Jane Marsh, attendees: Executive team, Clinical Directors, programme leads Next Generation Programme Board (extends across Facilities, People, Technology) Provides clinical challenge & assurance Every 6 weeks Lead: Claire Burden Attendees: Stream leads for OP and surgery plus ~10 clinicians EQuIP Clinical Panel Weekly to drive project Clinical lead: rotates (Tony Lander, Ingo Jester, Suren Arul, Neil Bugg) Ops lead: split (TBC for on the day efficiencies, Tom Adamson for scheduling, Keely McDougall for data quality, Claire Morgan for pre-op) Finance lead: Adele Struebig Multiple attendees clinical and ops Exec CIP Meeting BCH/Newton Contract Review Surgical Flow Group Outpatient Mgmt. Group Task and Task and finish groups Task and finish groups finish groups Task and Task and finish groups Task and finish groups finish groups Weekly to drive delivery of CIP, to escalate areas/services for challenge Chair: Phil Foster, attendees: Michelle McLoughlin, Vin Diwakar, Matthew Boazman, Kevin Sample, Tim Atack, Lukas Mol Every 6 weeks to review earned value, benefits tracking, feedback and BCH/Newton partnership Attendees: Phil Foster, Claire Burden, Nick Barlow, Lukas Mol Weekly to drive project Clinical lead: Gill Derrick Ops lead: Neil Barnett Finance lead: Adele Struebig Multiple attendees clinical and ops Legacy and Sustainability The benefits which these projects are delivering include: - For patients and families: o Shorter, more effective and efficient pathways o Improved experience in clinics o Shorter waiting times, greater access to our services o Improved clarity of communication, “the BCH way” o Smoothing and matching of demand to capacity - For staff: o Reward from successful delivery of a major change programme, building momentum and confidence for Trust wide transformation o Greater satisfaction, reduced frustration from efficient processes 3 Less time spent being reactive, more time proactively looking forward Building Team BCH – in terms of cross functional teamwork, values, sense of belonging, capacity, capability o Transparency and data quality – access to and value of information about your own service delivery Operational: o Shorter, more effective and efficient pathways o Reduced waiting times and improved access to care o More efficient processes to manage capacity and demand o Development of a model for change o Improved data quality for reporting, measurement and driving improvement Financial: o An improved service delivered in a more cost effective way o Enabling opportunities for growth o Maximise market opportunities and value for money o See above for numbers o o - - These benefits are being embedded to leave a legacy through a number of methods, including: - High levels of clinical engagement throughout the identification, design and implementation phases to provide guidance, build a sense of pride and ownership - Implementation of daily, weekly and monthly improvement cycles to embed changes as part of business as usual with clear accountability. To ensure that all changes are monitored, reviewed and actions taken as required to drive continuous improvement. - Information tools which provide a high degree of insight into the service being provided by every team. This is achieved through the ‘HEIDI’ tools (‘Hospital Efficiency Improvements Driven by Information’). The information presented is personalised, highly relevant and drives actions. - Learning and development – the core team have been trained in basic improvement techniques and been able to put these into practice through these projects. This team are now becoming trainers themselves to ensure that this knowledge and skill set grows within the organisation. The wider project teams have been involved in workshops and have used techniques which can be applied to a wide range of challenges. The biggest sustainability risk is within the surgery project. Early results look good and there are some brilliant people involved, but the team does not have a consistent enough core team (refer to governance structure above) to give total confidence that the improvements will go from strength to strength after the main part of the implementation. This project needs a strong clinical lead (one name, not split ownership) to finish delivery, manage the transition to business as usual and drive even more improvement. Risks & Opportunities to Maximise Value Delivered With the current setup, this programme will deliver at target levels and it will be remembered as a good programme. With the right ambition, there is an opportunity at this point to increase value delivered to well in excess of target levels, closer to the stretch values. If we can do this, this work will be remembered as a great programme which delivered an amazing set of outcomes and set BCH up for Trust wide transformation in the years to come. The changes will require difficult conversations and moral courage to make them happen. The top opportunities to maximise value delivered by this programme are below (extracted from the project risk register): 4 - Surgical flow team strength and consistency. Operational strength poses a risk to sustainability, clinical leadership poses a risk to total value delivered. Absolute clarity around session length in surgery. Enabling this change will unlock hundreds of thousands of pounds worth of additional opportunity Acknowledgement that bed constraints will become a bottleneck for flow through the pathway again in the future, identify how to ease this constraint A forum to escalate opportunities to (for example outpatient template changes) when services need to be more ambitious with their plans Recommendations Note the project successes in combination with the financial overview. Explore and discuss the levers to maximise the value delivered by this programme, challenge and support the core team to enable these changes to happen. 5 Appendices to Patient Pathways Interim Review Trust Board October 2014 Page 1 Appendices 1. 2. 3. 4. 5. Introduction to the outpatient and surgery projects from January 2014 One page project health summaries for outpatients and surgery Earned value management reports showing activity progress against plan Benefits tracking – financial opportunity, target and actual by service and project ‘HEIDI’ examples Page 2 Appendix 1 – Introduction to the outpatient and surgery projects from January 2014 • Outpatients – – • Surgical Flow – – • Executive summary introduction Outline project plan Executive summary introduction Outline project plan Key deliverables and benefits Page 3 Executive Summary – Outpatients Understanding opportunities through studies and data analysis • • • Approach Q-matic and Attendance data for Apr-12 to Oct-13 Clinic Tracker to capture live start and finish times Clinic studies across departments and sites Clinic Templates Patient Waits & Flow in Department Booking & Capacity and Demand Findings • • 48% of clinic time is spent face to face with patients – <2hrs Opportunity to better utilise clinic time & reduce waits through full template review • • Flow in department reduced by inconsistent template structure Existing process not optimised to ensure short wait times & productivity • • Poor visibility on un-used slots, difficulties to drive a pro-actively driven booking process OP Room capacity on specialty level doesn’t match demand Benefits Patient: Improved access to care, reduced waiting lists, fewer DNAs and on-the-day cancellations Staff: Fewer over-runs, reduced demand and more even work load through the day, reduced delays Operational: Greater visibility to better plan resources, ability to flexibly match capacity to demand Financial: £1.2M - £1.4M pa through income and WLI cost avoidance due to fewer sessions to meet demand Delivery 6-8 months to setup a data driven clinic template review process with the specialty CDs / DMs, optimise existing booking process and improve visibility of booking through PASplus+ booking and reporting systems, capacity & demand modelling, optimise flow in OP department and set-up a Trust-Wide performance review structure. Page 4 Project Plan – Outpatients M1 M2 M3 M4 M5 M6 M7 M8 M9 M10 Kick-off sessions Establish project team and project board Project Setup & Governance PID Delivery plan, project milestones, results glidepath KPI Dashboard Change, risk, and issue logs PASplus+ OP Module PASplus+ OP Module Improvement Project - Outpatients Booking Efficiency, Templates, Vacant Slots, Utilisation Provide visibility of opportunity Trust-Wide Standardisation of Outpatient Service Support standardisation of Clinic Session length to match Job-Plan Clinic Utilisation Tracker Template Visibility Matching Capacity and Demand Template review training Training Trust Team Consultant Review and Objection Handling Outpatient Improvement Cycle Process training Vacant slot booking tools Drive Booking Efficiency Review Process Removing Over Capacity Clinics Newton Led: Clinic studies Specialty engagement meetings Phase 1 Specialties Template reviews On-the-day problem fixes Ensure appropriate resource seeing patients to maximise capacity • Specialtiy group 2 • Newton-led with greater support from DM Phase 2 Specialties • Ongoing work lead internally by the trust team with appropriate support from Newton Phase 3 Specialties Page 5 Executive Summary – Surgery In session studies - 48hrs of live studies Approach Historical data analysis Time with Team • - ORMIS and iPM Apr 12 to Oct13 • Booking Visibility Schedule Mismatch Operational & clinical (surgeons, nursing, theatres, anaesthetics) Bookings team On-the-day Delays Findings • 74% of session time spent operating • Lack of visibility of lists and anticipated performance • No data driven review process Benefits Delivery • Mismatch between Capacity & Demand • Lack of clarity over start-times and Finish Times • Delays in starting lists and turnarounds lead to over-runs and cancellations • Poor staff and patient experience • OTD cancellations Patient: Improved access to care, reduced waiting lists and fewer on-the-day cancellations Staff: Fewer over-runs, increased accountability from all in team for performance, reduced delays Operational: Greater visibility to better plan resources, continuous review of performance and causes of lost time Financial: £1.3M - £1.6M pa through income and WLI cost avoidance due to fewer sessions to meet demand 5-7 months to optimise existing booking process and improve visibility of booking through PASplus+ booking and reporting systems, capacity & demand modelling, optimise morning start procedures and set-up a performance review structure to value, prioritise and tackle the greatest sources of lost time and causes for over-runs. Page 6 Project Plan – Surgery M1 Project Governance • • • • • M2 M3 M4 M5 Kick-of f sessions Establish project team and project board PID Deliv ery plan, project milestones, results glidepath Change, risk, and issue logs Improvement Project - Theatres • Finalise installation requirements Performance Reporting Development - Booking - Live View (24hr) of Theatres - Performance Reporting • DB/Serv er procurement & setup • Hardware lead time • Installation & conf iguration • Test • Acceptance • Workshops, training • Setup action meetings • Start steering using perf ormance reporting Support improvement cycle • Dev elop,agree, and implement theatre SOPs • Challenge and lost time, sy nchronise theatre sessions and MDTs, etc.; capacity balancing • Focus on start time and issues Drive Theatre On-the-Day Efficiencies Drive Booking Efficiency & Implement Improvement Cycle Capacity and Demand Planning - Elective, Emergency & Trauma lists • • • • • Improv e v isibility of waiting list, perf ormance, and booking ef f iciency Driv e appropriate booking rev iews, daily , weekly , monthly Improv e clarity on cancellation of sessions and improv e uptake Implement perf ormance reports Driv e improv ement cy cle with local team • Capacity and demand modelling f or electiv e lists • Optimise capacity to Emergency & Trauma demand • Improv e v isibility of waiting list, utilisation of sessions and in-session utilisation to driv e capcacity and demand planning on a regular basis Page 7 M6 M7 Key Deliverables & Benefits Financial Opportunity (p.a.) Project Outpatients Surgical Flow Key Workstreams Key Benefits 3.5 hours 4 hours • Improve flow through department • Booking performance • Prioritised template review • Capacity & demand matching • Patients: Improved access to care, reduced waiting lists, fewer DNAs and on-the-day cancellations • Staff: Fewer over-runs, reduced demand and more even work load through the day, reduced delays • Operational: Greater visibility to better plan resources, ability to flexibly match capacity to demand £900k £1.2M p.a. £1.4M £1.7M p.a. • • • • • Patients: Improved access to care, reduced waiting lists and fewer on-the-day cancellations • Staff: Fewer over-runs, increased accountability from all in team for performance, reduced delays • Operational: Greater visibility to better plan resources, continuous review of performance and causes of lost time £700k £1.3M p.a. £1.6M £2.3M p.a. £1.6M £2.5M p.a. £3.0M £4.0M p.a. Reduce on-the-day delays Improve start procedure Improve booking process Capacity & demand matching Opportunity Page 8 Appendix 2 – One page project health summaries • • Outpatients one page project health summary as of 18 September 2014 Surgical Flow one page project health summary as of 18 September 2014 Page 9 Next Generation – Patient Pathways – Outpatients - Status “Improving the experience of moving through our hospital systems to help children get home quicker” Project Sponsor: David Melbourne Patient Pathways clinical panel: Operational owner: Claire Burden Reporting to: Patient Pathways (Clinical Panel), and in turn to (TLT) Gill Derrick, Fiona Reynolds, Oliver Gee, Ian Wacogne, Phil Debenham, Bryan Healy, Gary Williams, Marion Harris, ASD rep Outpatient Management Group: Phil Debenham, Andrea Jester, Gill Derrick, Neil Barnett, Yvonne Millard, Angie Hall, Alex Borg, Liz Meredith, Sue Hobday, Debra Fitzgerald, Sian Holmes, Charlotte Reynolds, Tom Adamson/Lacey Bennett, Bo Dury, Shahab Raza, Georgina Mann Work stream Problem No visibility of clinic 1. Measures utilisation and poor & Visibility visibility of unused slots 2. Service Redesign Average patient-facing time is <70% of 3.5hr clinic time Objectives - Install and implement clinic tracking tool Install and implement booking visibility tool - Redesign clinics & templates to ensure resources are fully utilised while improving patient and staff experience PLAN Apr May Jun Jul Aug Sep Oct Nov RAG Update - Clinic tracker rolled out Booking tool installed,providing slotcentric view of short term available capacity - Agreed demand and WLI numbers through target forms Redesign of clinic templates in progress (specialty by specialty) - 3. Patient Flow Long patient waiting times and ~9% of clinician time waiting for patients - - Eliminate clinic late starts due to flow issues Reduce average & max patient wait times Improve patient non-wait experience - 4. Booking Efficiency ~15% of slots unbooked - Improve booking efficiency by driving a proactive booking process - Process improvements in main OP implemented Reduced patient pre-clinic time to 14min 30sec Eliminated late starting clinics due to patient hold ups Roll out of best practice to other OP locations Successful trial of booking tool use in call centre to avoid unfilled slots for new appointments Improved booking process drafted to integrate all parties involved Roll out to other specialties Risks and Issues: • • Current template design and booking processes very show large inconsistencies. This reduces transparency of the clinic redesign impact. Risk of keeping status quo or reduced capacity if not enough challenge is provided Potential capacity not being considered in areas where no pressure in service • Page 10 Sustainability of service redesign process is hard to ensure. Slow cycle means it is hard to trial. Lack of template change process governance poses risk to stability. Next Generation – Patient Pathways – Surgical Flow - Status Ensuring the best use of theatre resource whilst improving patient experience and maximising flow Work stream Problem Data Quality Theatre reports inconsistent, with limited understanding of the data source Scheduling processes Manual and inefficient process of ensuring lists are correctly booked On-the-day efficiencies Over 1000 hrs. per year of theatre time lost to late starts - - Improving flow and Realising the scheduling alone may not value realise financial benefit Preassessment No consistent preassessment service across the trust PLAN Objectives - Apr May Jun Integrate HEIDI surgery software to give new and accurate reports Make ORMIS complete and correct Use HEIDI booking tool for automatic visibility of over- and under-booked lists Redesign theatre scheduling processes to ensure the best use of lists Reduce late starts and turnarounds, giving confidence to book lists fully Use new reports to continually improve Aug Sep Oct RAG Update - http://Heidi-surgery is live Ophthalmology, gastro and IR clinicians already using HEIDI to look at how they run their lists - HEIDI booking tool now used to coordinate D4 scheduling with theatres – directly drives booking efficiency - Identifying 1st and 2nd patient on list before the day of surgery to fix list start Structured ‘morning flow procedure’ drawn up and being shared with all involved departments - Convert productivity improvements into financial value - To provide pre-assessment service for every child requiring GA or sedation Trust-wide theatre list productivity – last 10 weeks Jul Clarity by specialty through target forms on activity trends and WLI usage Need to setup actions against % improvements Progress working with specialties to define their pre-assessment needs and identify current practice Risks & issues: • Lack of project and change management skills with the trust team members on this work stream could lead to poorly sustained results. Currently heavily supported by Newton workstream owner • Theatre lists are bookable for 7 hours per day – yet we staff for 9.5 hours, which typically endable 8 hours of bookable list time. Clinical ownership is needed to challenge the current working practice and plan how to improve this. • Bed constraints could limit theatre productivity gains – work planned to look at how scheduling changes could affect long term demand on beds Page 11 1. Appendix 4 – Benefits tracking – financial opportunity, target and actual by service and project • • • Outpatients benefits tracking Surgical Flow benefits tracking Combined programme cash flow forecast Page 13 Outpatients Benefits Tracking 17/09/2014 Outpatient Assessment Target Form Target form Difference to Specialty Scope Target (4 hrs) completed Value Assessment Cardiology 1 £133.9k draft £86.7k -£47.2k Cardiac Surgery £.0k Clinical Haematology 1 £148.9k signed £33.8k -£115.2k Oncology 1 £24.9k signed £13.3k -£11.6k Dermatology 1 £23.8k signed £35.6k £11.8k Gastroenterology 1 £62.3k draft £65.5k £3.3k General Paediatrics 1 £106.8k signed £129.6k £22.8k Neurology 1 £89.3k signed £101.4k £12.1k Rheumatology 1 £24.0k signed £36.6k £12.6k Cranio £.0k Dental 1 £6.2k signed £2.9k -£3.4k ENT 1 £63.3k draft £35.9k -£27.4k Max Facs 1 £.0k draft £11.7k £11.7k Neurosurgery 1 £27.7k draft £18.6k -£9.1k Ophthalmology 1 £82.4k signed £42.5k -£40.0k Plastic Surgery 1 £45.1k draft £28.5k -£16.6k Paediatric Surgery 1 £68.3k signed £34.9k -£33.4k T&O 1 £88.7k signed £28.1k -£60.6k Urology 1 £56.0k signed £24.6k -£31.4k Cleft 1 £11.2k no form -£11.2k Nephrology 1 £51.8k no form -£51.8k Hepatology and Hepa 1 £.0k Endocrinology 1 £43.0k draft £36.7k -£6.2k Respiratory 1 £32.7k draft £23.0k -£9.7k Retinoblastoma 1 no form £.0k Burns 1 no form £.0k Diabetics draft £.0k Metabolic Disease signed £.0k Thoracic Surgery 1 no form £.0k Spines ? £.0k Interventional Radiolog ? £.0k Slot Utilisation £240.0k draft £292.6k £52.6k Total £1430.0k £1082.4k Page 14 Remarks No improvement target % on form - estimated value Pressures on specialty mean that value cannot be realised as expected Block Contract Lot of clinics overrunning. Needs further checking Target form value lower as ~2000 FU activity = pre-admission clinic Removed fracture clinic activity Target form not yet completed Target form not yet completed Block Contract Block Contract Bringing slot utilisation up to 95% across all specialties delivers £293k Surgical Flow Benefits Tracking 17/09/2014 Surgical Flow Assessment Target Form Target form Difference to Specialty Scope Target (3.5 hrs) completed Value Draft Identified Assessment Cardiology ! £68.0k no form £.0k -£68.0k Cardiac Surgery ! £163.0k no form £.0k -£163.0k Clinical Haematology £.0k Oncology £.0k Dermatology £.0k Gastroenterology 1 draft £27.0k £58.6k £27.0k General Paediatrics £.0k Neurology £.0k Rheumatology £.0k Cranio 1 £.0k £.0k Dental 1 £2.0k draft £3.2k £1.2k ENT 1 £91.0k draft £144.8k £195.7k £53.8k Max Facs 1 £6.0k draft £6.2k £3.9k £.2k Neurosurgery 1 £12.0k draft £18.7k £6.7k Ophthalmology 1 £20.0k draft £22.5k £31.9k £2.5k Plastic Surgery 1 £60.0k draft £95.4k £170.1k £35.4k Paediatric Surgery 1 £85.0k draft £83.4k £158.4k -£1.6k T&O 1 £44.0k draft £61.7k £189.1k £17.7k Urology 1 £105.0k draft £109.5k £191.6k £4.5k Cleft 1 no form £.0k Nephrology £.0k Hepatology and Hepat 1 £7.0k draft -£7.0k Endocrinology £.0k Respiratory £.0k Retinoblastoma 1 £.0k £.0k Burns 1 £.0k £.0k Diabetics £.0k Metabolic Disease £.0k Thoracic Surgery £.0k Spines ? £5.0k draft £6.4k £1.4k Interventional Radiolog 1 £15.0k £.0k Total £668.0k £578.8k Remarks Not requested - out of scope Not requested - out of scope small 7% late starts, 6% early finish.Aim 50% improvement// Util :73% to 80% small Block Contract, possibly a WLI reduction saving only long turnarounds an issue. 'Ideal' lists with minimal early start, minimal early finish, a 4% late starts, 6% early finish. Aim 50% improvement // Util :75% to 80% 8% 8% 5% 7% 5% late starts, late starts. late starts, late starts, late starts, 2% overruns, so 6% useful. Aim 50% impr. // Util :78% to 81% Take a 50% improvement // Util :71% to 75% 4% early finish. Aim 50% improvement // Util :74% to 79% 5% early finish. Aim 50% improvement // Util :77% to 83% 5% early finish. Aim 50% improvement // Util :75% to 80% small Block Contract, possibly a WLI reduction saving only Block Contract, possibly a WLI reduction saving only Wrapped up into Paediatric Surgery not BCH based activity 12% late starts, 2% early finish. Aim for 50% improvement // Util :66% to 73% £1014.3k August SF savings run rate £526k (based on draft baselines) Page 15 Combined Programme Cash Flow Forecast Page 16 Appendix 5 – ‘HEIDI’ Examples • • Screenshots Example of scheduling process changes showing role of HEIDI Page 17 HEIDI - Reporting Home by Site/Spec/Surg/Anaes Page 18 HEIDI - Daily Gantt View of Lists Page 19 HEIDI – Weekly/Monthly Trends Page 20 Example of scheduling process changes showing role of HEIDI Previously With HEIDI in place Relets Relets Relet Record (Excel) Rotas ORMIS (Trust system) D4 list planning ORMIS (Trust system) Theatres schedule (Excel) D4 list schedule (Excel) = ? Relet Record (intranet) Rotas HEIDI (Trust system) Theatres Scheduling D4 list planning Page 21 = Theatres Scheduling