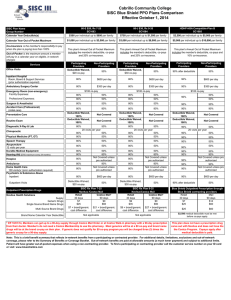
SISC Plan Name Group Number Participating Non-Participating
advertisement

Cabrillo Community College SISC Blue Shield PPO Plans Comparison Effective October 1, 2015 80-E $20, Rx 7-25 SC1083 SISC Plan Name Group Number HDHP-HSA Compatible-Plan B SC1085 80-J $30, Rx 9-35 SC1084 $300 per individual up to $600 per family $750 per individual up to $1,500 per family $3,000 per individual up to $5,000 per family $1,000 per individual up to $3,000 per family $3,000 per individual up to $6,000 per family $5,000 per individual up to $10,000 per family This plan's Annual Out of Pocket Maximum includes the member's deductible, co-pays and 20% co-insurance. This plan's Annual Out of Pocket Maximum includes the member's deductible, co-pays and 20% co-insurance. This plan's Annual Out of Pocket Maximum includes the member's deductible, co-pays and 10% co-insurance. Participating Providers Deductible Waived, $20 co-pay Non-Participating Providers Participating Providers Deductible Waived, $30 co-pay Non-Participating Providers Participating Providers Non-Participating Providers 50% 90% after deductible 50% Inpatient Hospital Room, Board & Support Services (prior authorization required) 80% $600 per day 80% $600 per day 90% $600 per day Ambulatory Surgery Center 80% $350 per day 80% $350 per day 90% Calendar Year Deductible(s) Calendar Year Out of Pocket Maximum Co-insurance is the member's responsibility to pay when the plan is paying less than 100% Out of Pocket is the maximum amount a member will pay in a calendar year on eligible, in-network charges Services Office Visits Emergency Room (non-emergency) Facility Expenses: Professional Expenses: Surgeon & Anesthetist Accident Care (Professional) (initial care) $100 co-pay Routine Exam Diagnostic X-Ray & Lab $100 co-pay 80% 50% 80% 50% 50% 80% 50% 80% 50% 80% 50% 90% 50% 80% 80% 80% 80% 90% 90% Not Covered Not Covered 80% 20 visits per year 80% 80% Not Covered Speech Therapy Acupuncture 12 visits per year Durable Medical Equipment Hearing Aid ($700 maximum every 24 months) Hospice 80% Ambulance Home Health Care 100 visits/yr (prior authorization required) Psychiatric & Substance Abuse Inpatient 80% Chiropractic Physical Medicine (PT, OT) Outpatient Visits Outpatient Prescription Drugs Navitus Health Solutions Supply Generic Drugs Single Source Brand Name Drugs Multi Source Brand Drugs $350 per day $100 co-pay 80% Deductible Waived, 100% Deductible Waived, 100% Preventative Care 50% Deductible Waived, 100% Deductible Waived, 100% Not Covered Not Covered Not Covered Not Covered 80% 20 visits per year 80% 80% 80% 50% 80% 50% 80% 50% 80% 50% 80% 80% Not Covered 80% Not Covered unless pre authorized 80% Not Covered unless pre authorized 80% 80% Not Covered 80% Not Covered unless pre authorized 80% Not Covered unless pre authorized 80% Not Covered 80% $600 per day Deductible Waived, 50% $20 co-pay SISC Rx Plan 7-25 Navitus /Costco Mail Retail Costco Mail* 30 days 90 days $7 $0 $25 $60 $7 + brand/generic $21 + brand/generic cost difference cost difference 80% 80% 80% Not Covered Not Covered 80% $600 per day Deductible Waived, 50% $30 co-pay SISC Rx Plan 9-35 Navitus/Costco Mail Retail Costco Mail* 30 days 90 days $9 $0 $35 $90 $9 + brand/generic $27 + brand/generic cost difference cost difference 90% Deductible Waived, 100% Deductible Waived, 100% 50% 50% Not Covered Not Covered 90% 20 visits per year 90% Not Covered 90% Not Covered 90% 50% 90% 90% 90% 90% 90% 90% Not Covered 50% Not Covered 90% Not Covered unless pre authorized 90% Not Covered unless pre authorized 90% $600 per day 90% after deductible 50% Blue Shield Outpatient Prescription through Blue Shield contracting providers Retail Mail 30 days 90 days $7 $14 $25 $60 $25 $60 Brand Name Calendar Year Deductible Not applicable Not applicable $3,000 medical deductible must be met before co-pays apply. Prescription Drug Out-of-Pocket Maximum (individual/family) $1,500/$2,500 $2,500/$3,500 Prescriptions are part of the medical and subject to the medical Out-of-Pocket Maximum * Eff 10/01/14, Members can get up to a 90-day supply through Costco Mail Order or at Costco Walk-in pharmacy with a 90-day prescription from their doctor. Member's do not need a Costco Membership to use the pharmacy. Most generics will be at a $0 co-pay and brand name drugs will be at the brand co-pay on their plan. If generic does not qualify for $0 co-pay program you will be charged three (3) times the generic co-pay for a 90-day supply. This plan does not have a prescription drug carve out with Navitus and does not have the the Costco Program. Copays apply after medical deductible is paid. Note: This is a brief benefit summary that reflects in-network benefits from a participating or contracted provider. For additional details, limitations, exclusions and out-of-network coverage, please refer to the Summary of Benefits or Coverage Booklet. Out-of-network benefits are paid at allowable amounts (a much lower payment) and subject to additional limits. Patient will have greater out-of-pocket expenses when using a non-contracting provider. To find a participating or contracting provider call the customer service number on your ID card or visit www.blueshieldca.com